

Original Article - Year 2024 - Volume 39 -
Application of the Deltopectoral Flap in the Reconstruction of Large Head and Neck Defects: Two Case Reports
Aplicações do retalho deltopeitoral na reconstrução de grandes defeitos da cabeça e pescoço: Relato de dois casos
ABSTRACT
Introduction The deltopectoral flap was first described by Aymard in 1917 for nose reconstruction but became prominent after 1965 when Bakamjian began to use it for pharyngoesophageal reconstructions.
Methods This study is a retrospective analysis of patients undergoing surgery in 2022. Among them, we selected two patients subjected to cervicofacial reconstruction with deltopectoral flap. Their assessment included age, gender, lesion etiology, defect location, number of surgical procedures performed per patient, postoperative complications, and the personal satisfaction of the subjects.
Results Patients underwent cervicofacial reconstruction after tumor resection, and both required more than a surgical time for pedicle refinement and transection. One patient had a defect in an operative wound after repositioning the remnant in the donor area leading to a hypertrophic and hypochromic scar in the surrounding region. In these two cases, the deltopectoral flap supplied thin skin, with similar texture and color to the cervicofacial region, a consistent and predictable pedicle, good defect cover, flap safety and reproductivity, a fast surgical technique, and no need for patient positioning change during the procedure.
Conclusions The deltopectoral flap remains a significant therapeutic option in reconstructing large head and bone defects despite the advent of microsurgery. It allows for efficient and reliable tissue transfer with small deformities in the donor area, allowing an acceptable aesthetic reconstruction.
Keywords: plastic surgery procedures; head and neck neoplasms; surgical flaps; therapeutics; postoperative complications
RESUMO
Introdução O retalho deltopeitoral foi descrito pela primeira vez por Aymard em 1917 para a reconstrução do nariz. Todavia, recebeu destaque a partir de 1965, quando Bakamjian começou a utilizar o retalho para reconstruções faringoesofágicas.
Métodos Análise retrospectiva de pacientes operados em 2022. Dentre estes, foram selecionados dois pacientes que foram submetidos à reconstrução cervicofacial com retalho deltopeitoral. Os pacientes foram avaliados em relação à idade, sexo, etiologia da lesão, localização do defeito e número de tempos cirúrgicos realizados por paciente. Foram ainda analisados complicações pós-operatórias e satisfação pessoal dos pacientes.
Resultados Os pacientes foram submetidos à reconstrução da região cervicofacial após ressecção tumoral e ambos necessitaram mais de um tempo cirúrgico para refinamento e transecção do pedículo. Um dos pacientes apresentou deiscência de ferida operatória após o reposicionamento do retalho na área doadora, evoluindo com cicatriz hipertrófica e hipocrômica em relação às áreas adjacentes. Nos dois casos descritos em nosso estudo, optou-se pela confecção do retalho deltopeitoral por fornecer um retalho com pele fina, textura e cor semelhantes à região cervicofacial, pedículo constante e previsível, bom alcance aos defeitos, segurança e reprodutividade do retalho, técnica cirúrgica rápida e sem necessidade de mudança de decúbito no intraoperatório.
Conclusões O retalho deltopeitoral permanece como importante opção de tratamento na reconstrução de grandes defeitos da cabeça e pescoço mesmo após o advento da microcirurgia. Permite a transferência de tecido de forma eficiente e confiável com pequena deformidade na área doadora, possibilitando uma reconstrução esteticamente aceitável.
Palavras-chave: procedimentos de cirurgia plástica; neoplasias de cabeça e pescoço; retalhos cirúrgicos; terapêutica; complicações pós-operatórias
Introduction
In 1917, Aymard was the first to describe the deltopectoral flap for nasal reconstructions. However, this flap grew in prominence in 1965 when Bakamjian began to use it for pharyngoesophageal reconstructions.1,2
The deltopectoral flap has an axial pattern based on the perforating vessels of the internal thoracic artery in its medial portion and a randomized pattern in its lateral portion.1,2,3
Although the deltopectoral flap lost popularity due to free flaps, it remains an alternative with no microsurgery availability or for patients not eligible for this technique.1,4
Objective
This study presented the applications of the deltopectoral flap for large cervicofacial defect closure, showing two patients undergoing this surgical technique in the Plastic Surgery Service of Hospital Federal da Lagoa, Rio de Janeiro, RJ, Brazil.
Methods
The study was a retrospective analysis of patients undergoing surgery in 2022 with the Head and Neck Surgery team. Among them, we selected two patients submitted to cervicofacial reconstruction with a deltopectoral flap.
Patient assessment included age, gender, lesion etiology, defect location, number of surgical times performed per patient, postoperative complications, and personal satisfaction of the subjects.
This study followed the ethical principles of Helsinki and received approval from the ethics committee of Hospital Federal da Lagoa.
Surgical technique
The flap was rectangular and located in the upper thoracic region from the sternum to the anterior region of the deltoid. The base of the flap was parasternal, 2cm from the sternal border. Its upper limit was the clavicle and its lower limit, parallel to the upper limit, lay between the third or fourth intercostal space.1
Sometimes, the flap length requires an extension to the lateral region of the deltoid to reach the defect. Expanders can promote tissue stretching before tissue transfer. Another strategy to reduce the chances of flap necrosis is previous autonomization of the distal end of the flap, promoting neovascularization in this location.5
The blood supply to this flap comes from the perforating vessels of the internal thoracic artery and contributions of the second and third perforating branches in its medial portion. The lateral portion of the deltoid groove has a random pattern derived from the musculocutaneous arteries of the deltoid and acromial branches of the thoracoacromial artery.1,2
The incision follows the previous marking of the flap and the dissection plane deep to the deltoid fascia in the deltoid region and the pectoral fascia in the thorax, distal to the base. The flap length varies according to the distance to the defect to reach and suture it with no tension. The flap pedicle remains, on average, for 2 to 3 weeks until neovascularization occurs in the recipient area.1
The second surgical procedure sections the pedicle and repositions the flap in the donor area. One may cover the remaining defect on the donor site with skin grafts until its complete healing. The deltopectoral flap often achieves a good aesthetic result with acceptable color and texture.1,6
Patient 1
A 71-year-old male patient presented to the unit with an ulcerated lesion in the left cervical region that had been developing for approximately 4 years (►Fig. 1). We performed the surgical planning for lesion resection and deltopectoral flap creation (►Fig. 2). The appearance after tumor resection showed free margins after post-intraoperative freezing (►Fig. 3). The deltopectoral flap closed the cervical defect (►Fig. 4 In the second surgical procedure, 4 weeks later, we sectioned the pedicle and placed a total skin graft on the remaining defect (►Fig. 5). A 6-month follow-up showed good healing of the flap and the grafted area (►Figs. 6 and 7). Lesion histopathology confirmed the diagnosis of keratotic basal cell carcinoma with pT2N0 staging.
Patient 2
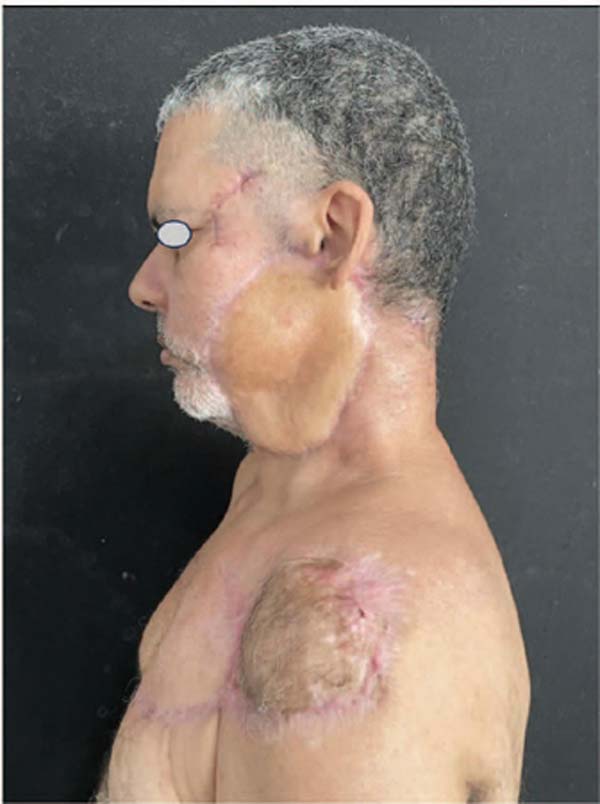
A 51-year-old male patient presented to the unit with a friable, ulcerative-vegetative lesion in the left cervicofacial region that evolved for 6 months and recently experienced accelerated growth (►Fig. 8). We performed surgical planning for lesion resection and deltopectoral flap creation (►Fig. 9). ►Figure 10 shows the immediate appearance after tumor resection. The deltopectoral flap closed the cervicofacial defect (►Fig. 11). In the second surgical procedure, 4 weeks later, we sectioned the pedicle and placed a total skin graft on the remaining defect (►Fig. 12). At a 3-month follow-up, we noted an area of surgical wound dehiscence after flap repositioning in the healing donor area (►Fig. 13). At a 6-month follow-up, the wound healing was complete (►Figs. 14 and 15). Histopathology showed high-grade mucoepidermoid carcinoma of the left parotid with a positive lymph node.
Due to the advanced stage, the patient required adjuvant treatment with intensity-modulated radiotherapy (IMRT) in a total dose of 6,000 cGy divided into 30 sessions. The patient is under monitoring by the Plastic Surgery, Head and Neck Surgery, and Radiotherapy teams.
Results
The patients underwent cervicofacial reconstruction after tumor resection, and both required more than one surgical procedure for pedicle refinement and transection.
No patients presented significant complications, such as partial or total flap necrosis, hematoma, or infection. One of the patients had a surgical wound dehiscence after flap repositioning in the donor area, which evolved with hypertrophic scarring and hypochromia in the adjacent regions.
During the postoperative visits, the differences in texture and color of the flap skin with the recipient area were minor. Both patients were satisfied with the outcome 6 months postoperatively.
Discussion
Some other flap options close head and neck defects, including the pedicled myocutaneous flap of the pectoralis major muscle, the myocutaneous flap of the trapezius muscle, and free flaps, such as the antebrachial flap.7
The pedicled myocutaneous flap of the pectoralis major muscle is a thin and flexible pedicled flap derived from perforators of the pectoralis major muscle, with minimal donor area morbidity and a good combination of color and texture for head and neck reconstructions. However, in some cases, it can be aesthetically unpleasant due to the flap volume.7,8
Nakajima and Fujino described the myocutaneous flap of the trapezius muscle in 1984. It is commonly used in post-radiotherapy patients and repeated surgical procedures because of free flap limitations. The latter is less appropriate in elderly patients due to the prolonged surgical time and the requirement of a specialized team, and the trapezius muscle flap may be an alternative. A disadvantage of this flap is the need to change position during surgery, which can be crucial in cancer patients, limiting its use.7,8,9
Advantages of free flaps include their thinness, resulting in less volume in the donor area; in addition, their vascular pedicle is often constant, and they are well tolerated by radiotherapy.8
Our patients underwent two surgical stages. A potential autonomization before flap transposition to promote neovascularization at the distal end could reduce the chances of necrosis in this area. This procedure can be critical in reconstructions after the failure of a previous flap. However, it would be necessary to wait 7 to 15 days for flap transfer, prolonging the surgical time. Moreover, the wait would further increase the defect in patients with neoplasms with a worse prognosis.10
In the cases described, we selected the deltopectoral flap because it supplied thin skin with similar texture and color to the cervicofacial region, a consistent and predictable pedicle, good defect cover, flap safety and reproductivity, a fast surgical technique, and no need for patient positioning change during the procedure.
Finally, the deltopectoral flap also treats complications such as salivary fistulas, cervical contractures, and postradiotherapy skin necrosis.7
Conclusion
The deltopectoral flap remains a significant therapeutic option in reconstructing large head and bone defects despite the advent of microsurgery. It allows for efficient and reliable tissue transfer with small deformities in the donor area, allowing an acceptable aesthetic reconstruction.
REFERENCES
1. Thomaidis V. Cutaneous Flaps in Head and Neck reconstruction: From anatomy to surgery. Berlin, Heidelberg: Springer; 2014. Disponível em: https://link.springer.com/chapter/10.1007/978-3-642-41254-7_9
2. Vanni CMRS. Retalho miocutâneo de peitoral maior nas reconstruções de defeitos da cabeça e pescoço: estudo anatômico. Orientador: Dr Fábio Roberto Pinto 2011. 155 p. Tese de douturado (Doutorado em ciências médicas) - Faculdade de Ciências Econômicas, Universidade de São Paulo, São Paulo, 2013
3. Shetty R, Barreto E, Paul M K. Incisão em abordagem única por meio de técnica de retalho deltopeitoral para reconstrução de traqueostomia em paciente submetido a radioterapia após laringectomia. Rev Bras Cir Plást 2014;29(02):294–296
4. Kang SK, Qamar SN, Tikka T, Milner TD. Deltopectoral Flap Reconstruction of the Posterior Pharyngeal Wall: A Single Stage Pedicle Flap Alternative Solution to the Free Flap Reconstruction of Circumferential Laryngopharyngeal Defects. Indian J Otolaryngol Head Neck Surg 2022;74(03):416–421
5. Ding J, Li Y, Li W, et al. Use of expanded deltopectoral skin flaps for facial reconstruction after sizeable benign tumor resections. Am J Transl Res 2018;10(07):2158–2163
6. Kerdoud O, Aloua R, Slimani F. The deltopectoral flap in fullthickness cheek defect: A case report. Ann Med Surg (Lond) 2021; 62:119–122
7. Chan RCL, Chan JYM. Deltopectoral flap in the era of microsurgery. Surg Res Pract 2014;2014(5p):420892
8. Portinho CP, et al. Reconstrução microcirúrgica em cabeça e pescoço: uma análise retrospectiva de 60 retalhos livres. Rev Bras Cir Plást 2013;28(03):434–443
9. Yang HJ, Lee DH, Kim YW, Lee SG, Cheon YW. The Trapezius Muscle Flap: A Viable Alternative for Posterior Scalp and Neck Reconstruction. Arch Plast Surg 2016;43(06):529–535
10. Colletti G, Autelitano L, Tewfik K, Rabbiosi D, Biglioli F. Autonomized flaps in secondary head and neck reconstructions. Acta Otorhinolaryngol Ital 2012;32(05):329–335
1. Plastic Surgery Service, Hospital Federal da
Lagoa, Rio de Janeiro, RJ, Brazil
Address for correspondence José Paulo Guedes Saint-Clair, Rua Jardim Botânico, 501, Jardim Botânico, 6° andar, Rio de Janeiro, RJ, Brazil, CEP 22470-050 (e-mail: jose_paulo_lp@hotmail.com; cirurgiaplasticahfl@gmail.com).
Article received: January 06, 2024.
Article accepted: November 16, 2024.
Conflict of Interests
The authors have no conflict of interest to declare.
































 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter