

Case Report - Year 2024 - Volume 39 -
Medial-posterior Thighplasty in S: A New Technique with Better Scar Concealment
Coxoplastia médio-posterior em S: uma nova técnica com melhor ocultação da cicatriz
ABSTRACT
This article presents a new thighplasty technique to solve the discomfort and stigma associated with scars in the groin or other anterior body regions after conventional thighplasties. This study presents a case report of a thighplasty technique performed in post-bariatric patients undergoing intense slimming. This technique relies on an Sshaped skin resection in the posteromedial region of the thigh, with no scar on the anterior part of the body. The patients did not present postoperative complications, and their scars were discrete. In addition, the technique resulted in a large excessive skin reduction in multiple vectors, improving body contour.
The technique involved the unprecedented positioning of the S-shaped scar in the subgluteal and posteromedial grooves of the thighs, with no anterior scar in the groin, significantly improving scar concealment. Since there was no suture line angulation, cutaneous tracing distribution was better, and the chance of wound dehiscence was lower. Meanwhile, it allowed the resection of large amounts of excessive skin in longitudinal and transverse directions under multi-vector traction.
This thighplasty technique is an innovative, unprecedented procedure allowing better scar concealment and probably decreases the complication rate due to the better distribution of the cicatricial tension
Keywords: adipose tissue; bariatric surgery; medial thighplasty; plastic surgery; post-bariatric surgery; subcutaneous fat; surgical flaps; thigh; thighplasty; weight loss; bariatric medicine; surgery; plastic; weight loss; fat substitutes; lower extremity
RESUMO
O objetivo dos autores é apresentar uma nova técnica de coxoplastia que resolva o desconforto e estigma associados a cicatrizes na virilha ou outras regiões anteriores do corpo após coxoplastias convencionais.
O estudo apresenta um relato de caso de uma técnica de coxoplastia realizada em pacientes pós-bariátricas submetidas a intenso emagrecimento, pormeio de ressecção de pele em S realizada na região póstero-medial da coxa, sem cicatriz na parte anterior do corpo. As pacientes não apresentaram complicações pós-operatórias e apresentaram cicatrizes discretas. Além disso, a técnica consegue uma grande redução do excesso de pele, em múltiplos vetores, melhorando o contorno corporal.
A técnica envolve o posicionamento inédito da cicatriz em forma de S nos sulcos subglúteos e posteromediais das coxas, sem cicatriz anterior na virilha, melhorando significativamente o ocultamento da cicatriz. Permite também não ter angulações na linha de sutura, melhor distribuição das trações cutâneas, menor chance de deiscência da ferida, ao mesmo tempo em que permite a ressecção de grandes quantidades de excesso de pele nas direções longitudinal e transversal, com tração em múltiplos vetores.
A técnica de coxoplastia apresentada é um procedimento inovador, inédito, que permite um melhor ocultamento da cicatriz e provável menor incidência de complicações devido à melhor distribuição da tensão cicatricial.
Palavras-chave: tecido adiposo; cirurgia bariátrica; coxoplastia medial; cirurgia plástica; cirurgia pós-bariátrica; gordura subcutânea; retalhos cirúrgicos; coxa; coxoplastia; perda de peso; medicina bariátrica; procedimentos de cirurgia plástica; redução de peso; gordura subcutânea; perna (membro)
Introduction
The increasing global incidence of obesity resulted in a large number of patients undergoing bariatric surgery, which leads to excessive skin and soft tissue and decreased skin tone.1 Excessive fat and skin accumulation often cause social discomfort, local skin lesions due to friction between the thighs, movement difficulty, discomfort in the patient’s sex life, and self-esteem issues.1
The first author todescribe thighplasty was Lewis2 in 1957. In 1988, Lockwood et al.3 revolutionized thighplasty by anchoring the skin flap to Colles’ fascia,4,5,6 increasing surgical stability and decreasing complications.7 Le Louarn (2004) added the critical role of radical liposuction before avulsion resection to minimize lymphatic complications and reduce edema and seroma formation.8
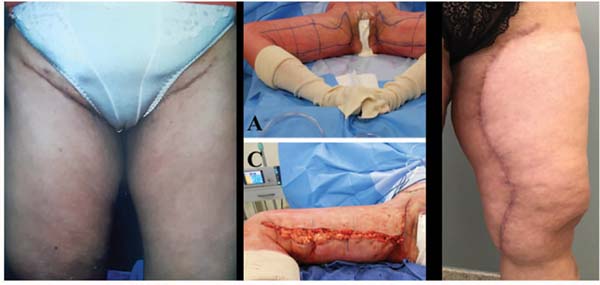
Thigh subcutaneous adipose tissue resection techniques described to date include the J- and T-shaped scar techniques. Longitudinal resection gained prominence for skin traction in longitudinal and transverse directions.9,10,11 However, these techniques still result in anterior transverse scars at the thigh root and groin (►Fig. 1) that can be conspicuous and stigmatizing, especially in intimate life. Thus, despite the advances in current thighplasty techniques, two points remain unsolved: apparent anterior scar at the thigh root and groin and frequent suture dehiscence in scar angles.12
Objective
This study describes a new thighplasty technique with S-shaped skin resection in the posteromedial region of the thigh to further improve the aesthetic outcomes of the procedure by not producing anterior groin scars and angled scars to reduce their dehiscence.
Patient and methods
Inclusion criteria: patients over 18 years old, undergoing post-bariatric thighplasty with weight loss greater than or equal to 30kg, and a body mass index (BMI) below 30. The patients had no comorbidities or risk factors. They read and signed the informed consent form (ICF) authorizing the surgery and data publication for scientific purposes.
For deep vein thrombosis prevention, the patients received enoxaparin, 40mg, for 5 days.
Two female patients underwent post-bariatric surgery thighplasty with S-shaped skin resection. The first subject was 44 years old, weighed 77.5kg, had a BMI of 29.17, and had lost 30kg. The second subject was 39 years old, weighed 70.60 kg, had a BMI of 26.57, and had lost 30kg.
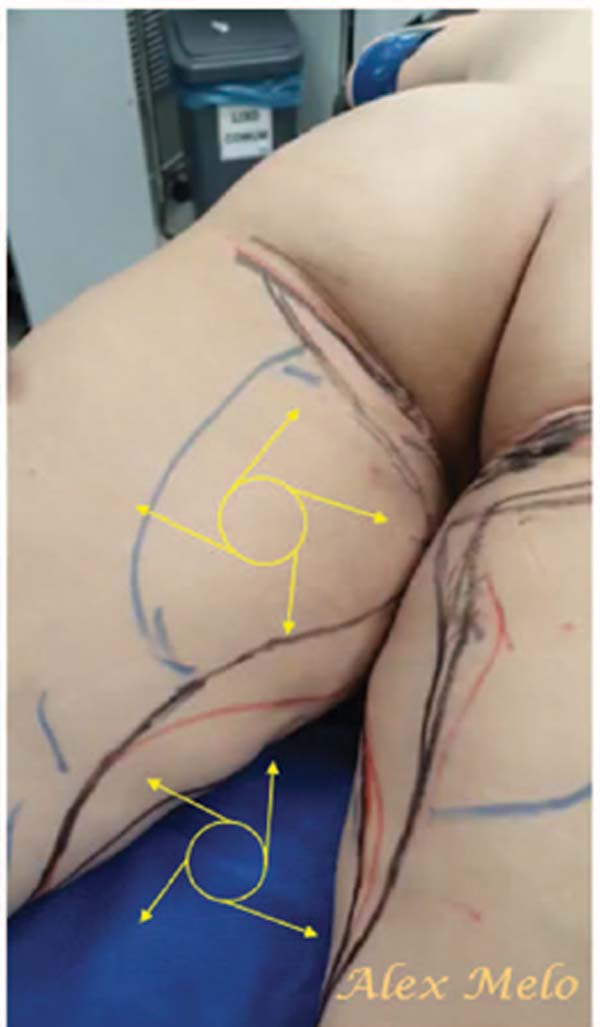
Using a bi-digital maneuver forceps test with tissue invagination, we made a mid-posterior S-shaped marking on the thigh with the patients in the orthostatic position and checked it in the prone position. This S-shaped marking for resection had the upper transverse part of the S in the sub-gluteal groove, and the longitudinal and transverse incisions of the S-shaped skin resection were distributed throughout the thigh (►Fig. 2).
Surgery occurred with the patient in the prone position.
After epidural anesthesia, we performed superficial and deep liposuction of the thighs with a vibro liposuction device radically in the areas for resection.
We performed skin resections by avulsion without detachment to preserve lymphatic circulation. Avulsion resection tends to reduce the incidence of seroma, lymphedema, and hematoma as it spares local circulation11,12 (►Fig. 3).
Results
The surgeries for both patients lasted 4hours each. The patients were discharged from the hospital on the same day and could walk normally. Suture removal occurred after 2 weeks, and the patients were under postoperative monitoring for 6 months. We instructed them not to squat for 2 weeks and to return to physical activities after 1 month.
The surgical technique of posterior medial thighplasty in S considerably reduced excessive skin, improving thigh contour. The mid-posterior resection in S evolved with no complications, including suture dehiscence. In addition, the resulting scar was in the sub-gluteal groove, the posterior region of the body, and the medial region of the thigh, forming a mid-posterior S-shaped scar, sparing the anterior region and the groin. The better scar concealment and the absence of a previous scar are the great achievements of this new technique, which may favor a potential improvement in the personal satisfaction of the patients and an increase in the number of treatments due to a likely greater acceptance by the subjects (►Figs. 4 and 5).
Discussion
Despite advances in thighplasty, the visible anterior scars and high rate of wound dehiscence remain unsolved.12 The new thighplasty using the S-shaped skin resection described here removes large amounts of excessive skin in the longitudinal and transverse directions without anterior groin scarring. The two cases described by the authors presented no wound dehiscence, probably because the angles were S-shaped, avoiding flaps with acute angles, which are more prone to ischemia and suture dehiscence.
Inelastic scar contractures frequently occur in the longitudinal component of the L and T-shaped scars from other thighplasties, often leading to linear fibrosis and noticeable scars potentially restricting local movement (contracture). In addition, they are more prone to ischemia, increased tension loading, suture dehiscence, and skin necrosis. These undesirable consequences are less likely to occur with S-shaped skin resections, as they do not create right or sharp angles. Furthermore, skin resection with an S-shaped incision on the cylindrical surface of the thigh simultaneously removes excessive longitudinal and transverse skin along the thigh in multiple vectors13 without requiring a separate straight-line vector, a step often needed for the T and L-shaped incisions (►Fig. 6).
The proposed technique solves the discomfort and aesthetic deficiencies resulting from scars from conventional thighplasties. Since the scars from the new technique are posterior and positioned in the sub-gluteal folds, they are perfectly hidden even with the thighs in abduction. Moreover, the technique may present a lower risk of dehiscence and skin retraction, as the S-shaped scars have no angles. Furthermore, it has the same, or even higher, potential for removing large skin amounts transversely and longitudinally. Lastly, it allows for better traction distribution from the root of the thigh to the knees. (►Figs. 7 and ).
Conclusion
The thighplasty technique presented here is an innovative and unprecedented procedure with an S-shaped resection, without suture angulations, and with better scar tension distribution. This results in better scar concealment since they are in the subgluteal and medial folds of the thigh. In addition, the new technique may reduce the chance of wound dehiscence, allowing extensive skin resection in the transverse and longitudinal directions in multiple vectors.13
This case report is the initial step in our studies to scientifically prove the virtues of this new surgical approach.
REFERENCES
1. Bertheuil N, Thienot S, Chaput B, Varin A, Watier E. Quality-of-Life assessmentafter medial thighplasty in patients following massive weight loss. Plast Reconstr Surg 2015;135(01):67e–73e
2. Lewis JR Jr. The thigh lift. J Int Coll Surg 1957;27(03):330–334
3. Lockwood TE. Fascial anchoring technique in medial thigh lifts. Plast Reconstr Surg 1988;82(02):299–304
4. Lockwood TE. Superficial fascial system (SFS) of the trunk and extremities: a new concept. Plast Reconstr Surg 1991;87(06): 1009–1018
5. Lockwood TE. Transverse flank-thigh-buttock lift with superficial fascial suspension. Plast Reconstr Surg 1991;87(06):1019–1027
6. Fowler ME, Lockwood TE. Medial Thigh Lift Coupled with Liposuction Produces Results Patients Desire. Plast Surg Nurs 1988;8 (04):146–149
7. Xie SM, Small K, Stark R, Constantine RS, Farkas JP, Kenkel JM. Personal Evolution inThighplasty Techniques for Patients Following Massive Weight Loss. Aesthet Surg J 2017;37(10):1124–1135
8. Le Louarn C, Pascal JF. The concentric medial thigh lift. Aesthetic Plast Surg 2004;28(01):20–23
9. Armijo BS, Campbell CF, Rohrich RJ. Four-step medial thighplasty: refined and reproducible. Plast Reconstr Surg 2014;134(05): 717e–725e
10. Labardi L, Gentile P, Gigliotti S, et al. Medial thighplasty: horizontal and vertical procedures after massive weight loss. J Cutan Aesthet Surg 2012;5(01):20–25
11. Hurwitz DJ. Medial thighplasty. Aesthet Surg J 2005;25(02): 180–191
12. Gusenoff JA, Coon D, Nayar H, Kling RE, Rubin JP. Medial thigh lift in the massive weight loss population: outcomes and complications. Plast Reconstr Surg 2015;135(01):98–106
13. Fantozzi F. Brachial lifting using the balanced triple-vector (BTV) technique with dual opposing flaps. Eur J Plast Surg 2014;37(02): 95–102
1. Plastic Surgery, Origen, Belo Horizonte, MG,
Brazil
2. Plastic Surgery, Hospital Felício Rocho, Belo
Horizonte, MG, Brazil
Address for correspondence Alexandre Melo dos Santos, Rua dos Aimorés, 462/418, Funcionário, Belo Horizonte, MG, Brazil (e-mail: plasticabhz@gmail.com; plasticabhz@gmail.com).
Article received: May 14, 2024.
Article accepted: September 29, 2024.
Conflict of Interest
The authors have no conflict of interest to declare.















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter