

Articles - Year 2003 - Volume 18 -
Surgery for Clefts: Helpful Details
Cirurgia de Fissurados: Detalhes que Facilitam
ABSTRACT
The number of patients with clefts seen at Rio de Janeiro Federal University's Clementino Fraga Filho University Hospital (HUCFF) has increased greatly in recent years. Based on the experience at our Service, we have observed technical specificities in relation to traditional sugery that have made the intraoperative and postoperative follow-up periods significantly easier. These "complements" are not usually described in detail in published articles and frequently lead to more questions than the sugical technique itself. We have therefore chosen to write a text aimed at complementing the knowledge usually given in publications, especially intra and postoperative care and the material used for sutgeries.
Keywords: Palate cleft - rehabilitation; lip cleft - rehabilitation; palate cleft - surgery; lip cleft - surgery
RESUMO
O número de pacientes fissurados atendidos no Hospital Universitário Clementino Fraga Filho (HUCFF), da Universidade Federal do Rio de Janeiro, tem crescido muito nos últimos anos. Tendo como base a experiência deste Serviço, foram observadas particularidades técnicas, em relação à cirurgia tradicional, que facilitaram o per-operatório e o acompanhamento pós-operatório de modo expressivo. Esses "complementos" não costumam ser descritos detalhadamente nos artigos publicados e muitas vezes despertam mais dúvidas do que a técnica cirúrgica propriamente dita. Sendo assim, optamos pela elaboração de um texto que possa complementar os conhecimentos normalmente passados pelas publicações, ressaltando-se cuidados per e pós-operatórios e material utilizado em cirurgias.
Palavras-chave: Fissura palatina - reabilitação; lábio fissurado - reabilitação; fissura palatina - cirurgia; lábio fissurado - cirurgia
The treatment of lip and palate clefts is currently multidisciplinary, performed by a team of plastic surgeons, dentists and speech therapists, among other professionals. The substantial increase in the amount of patients with clefts seen at Rio de Janeiro Federal University's Clementino Fraga Filho University Hospital (HUCFF) in recent years led us to create a subdivision named the Clefts Project (Pró-Fendas HU), responsible for treating patients with congenital malformations, mainly lip and palate clefts and microtia. We organize the participation of all the specialties necessary for adequate follow-up within the Unit.
The experience in the Service has led us to observe technical specificities in relation to traditional surgery that make intraoperative and postoperative follow-up care substantially easier.
These specificities may be used by anyone, and in our environment result in fewer complications and facilitated care to the patient.
We have noticed that many technical details that are part of our routine are object of greater interest to residents and visitors. These "complements" are not usually described in detail in published articles and frequently lead to more questions than the surgical technique itself.
The plastic surgeon who is beginning to work with cleft patients should necessarily observe the means used by more experienced professionals in order to reach satisfactory results. In addition to learning the stages of surgery, it is essential to know how to perform them adequately.
Therefore, we have chosen to write a text that may complement the knowledge usually given in publications.
OPERATIVE TECHNIQUE
ANESTHESIA
We use general anesthesia with orotracheal intubation for all lip and palate cleft surgeries. An armored tube is preferable due to its flexibility and smaller chance of kinking. It should be positioned in the median line of the mouth, without dislodging the tongue or lip commissures.
Additionally, the surgeon performs infiltration with 0.5% lidocaine, with 1/200,000 adrenaline for the lip, and 1/100,000 for the palate.
PATIENT PREPARATION
After consent from the anesthetist, the patient is put in the supine position, neck in hyperextension and the table in Trendelenburg (Rose position). A pad under the shoulders helps position the body.
No sudden movements or any movement without the acknowledgment of the anesthetist should be performed considering that most patients are very young and are intubated with uncuffed orotracheal tubes. Accidental extubation may occur easily and should be avoided.
We routinely use pharyngeal packing.
Antisepsis is petformed with chlorhexidine followed by alcohol chlorhexidine on the face, and chlorhexidine, in the oral cavity. The whole face is exposed, including in palatoplasties. Eyelids should be kept closed with the aide of tape.
UNILATERAL LIP CLEFT
We prefer the Millard(l) technique. It is the most commonly used technique worldwide and produces very satisfactory results. As a routine, we associate the nose detachment and repositioning recommended by McComb(2).
Skin incision markings should be well planned to attain adequate approximation of borders and lip balance. In order to determine the limits of the skin incision, we measure the normal filtral crest with a piece of suture attached to two Halstead forceps (mosquito) and transfer it to mark the C flap. The same measurement is used to mark the lateral advancing flap (Fig. 1).
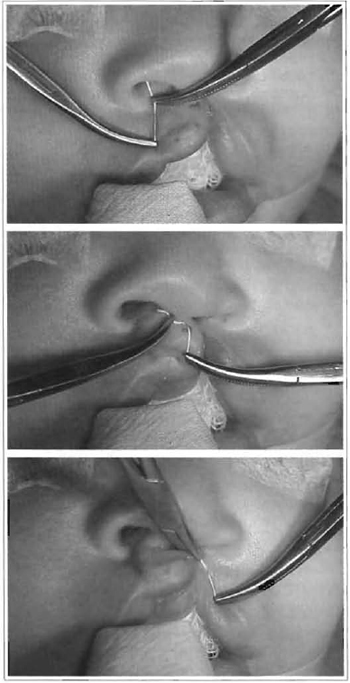
Fig. 1 - The flexibility of the suture fixed to the forceps facilitates the marking of skin flaps that have the same size as the normal filtral crest.
Surgical stages follow Millard's description, with the detachment of the nasal base performed in the subperiosteal plane to the level of the piriform fossa.
Detachment of the nasal dorsum practically reaches the whole hemi-dorsum affected by the cleft and is performed at the subcutaneous plane(2).
Mucosa and muscular syntheses are performed with absorbable monofilament polyglecaprone 25 (monocryl®), ranging from 4-0 to 5-0 in width.
After repositioning flaps, skin synthesis is either performed with 6-0 polyglactin 910 (vicryl rapideâ) or with a skin adhesive made of 2-octil cyanoacrylate (dermabondâ).
Needles are sharp and measure between 1.1 em and 1.5 cm.
The padded sutures for nasal support, described by McComb, are performed with some modifications. We use a straight needle with vicryl rapideâ 4-0 that enters through the nostrils, crosses the alar cartilage next to the dome and exits the skin at the root of the nose. The suture returns through the same skin orifice, passes the alar cartilage at another site and exits within the nostril. Another similar suture is performed in order to pull up the lateral portion of the nasal alae. When sutures are tied, the suture hook is pulled and invaginated into the subcutaneous. We do not use any type of suture padding (Fig. 2).
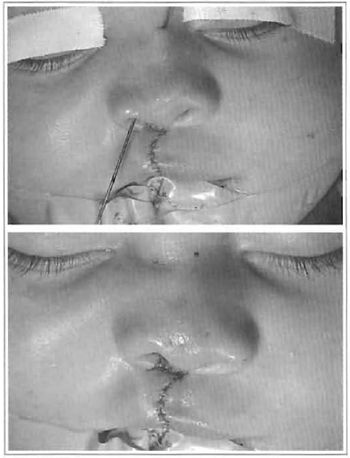
Fig. 2a-b - The nasal sutures recommended by McComb have been slightly changed. The needle returns through the same exit orifice. The suture is invaginated in the subcutaneous and there is no need for padded sutures.
BILATERAL LIP CLIFT
We use the one stage Spina(3) technique or the twostage Millard technique according to the presentation of the case.
Relevant technical details are similar to those described for the unilateral cleft, that is to say: sutures, detachments and support sutures.
PALATOPLASTY
After antisepsis and placing surgical drapes, we position the mouth gag. The orotracheal tube should be central in relation to the tongue and fitted into the central piece of the mouth gag.
A piece of rubber tube, approximately 3.0 cm long, is put between the tongue depressor and the teeth.
Sutures pull the uvulae towards the mouth gag, keeping the palate firm (Fig. 3).
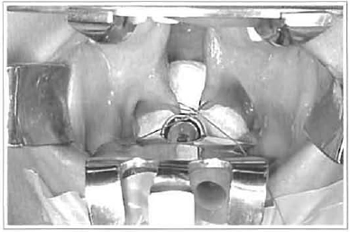
Fig. 3 - Details that translate into safety and comfort during palatoplasty: oropharyngeal packing; a rubber rube between the mouth gag and teeth ; and a surure pulling the uvula in the opposite direction.
We do not infiltrate the whole palate at once, but only the side we will begin to work on.
The techniques used for closing the palate vary according to the presentation of each case. The most commonly used techniques are Veau and WardillKilner for complete clefts and Von Langenbeck for incomplete ones.
Tissue detachment is performed with different types and shape detachers (Fig. 4).
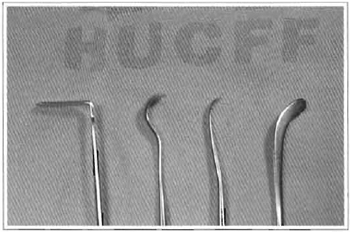
Fig. 4 - Adequate detachers make lip and palate flap release easier.
We normally suture the nasal mucosa immediately after it is released, before detaching lateral flaps, using simple monocryl® 5-0.
Muscles are released completely, repositioned and drawn together with simple or U sutures. The oral mucosa is detached according to the technique used and sutured with U sutures. Monocryl® 4-0 is used in both cases.
All palatoplasties are sutured with a 3/8 or 1/2 circleshaped sharp needle. We prefer to use a semicircular needle with a compound curvature and a more angular first third for the anterior portion of the palate (Fig. 5).

Fig. 5 - A compound curvature needle makes sutures of the anterior portion of the palate easier.
When mucoperiosteal flaps are released, leaving a raw area in the mouth, we pack these sites with an absorbable hemostatic regenerated cellulose compound (surgicel®) (Fig. 6).
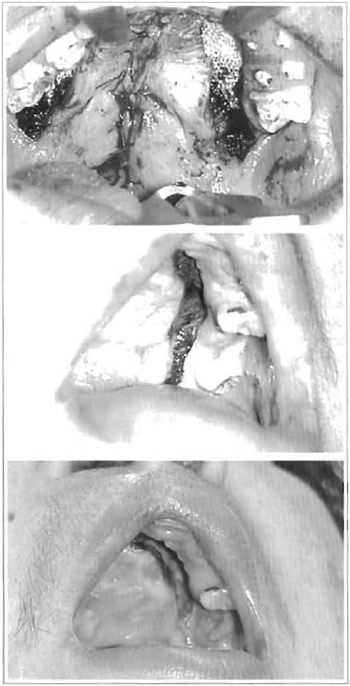
Fig. 6 - A: Packaging with surgicel at the end of surgery. B: Aspect after 24 hours. C: Aspect after 7 postoperative days.
We usually add a compressive dressing of folded gauze, in contact with the palate, fixed with 2-0 silk in X, crossing the palate for palatoplasties performed in adult patients, (Fig. 7). The dressing is removed on the day following surgery.

Fig. 7 - We use packaging with gauze during the first 24 postoperative hours in adult patients.
POSTOPERATIVE CARE
The patient should be kept in a lateral position to drain any existing bloody secretion during the immediate postoperative period.
Venous hydration is maintained until the patient is able to eat. Diet is given according to patient acceptance and request, as of 2 hours after the procedure, for children, and 4 to 6 hours, for adults.
The diet should be liquid-pureed on the first postoperative day. For lip clefts, a soft diet can be given after the second postoperative day. For palatoplasties, a pureed diet is maintained until the seventh postoperative day, evolving, gradually to a free diet as of the 21st postoperative day. After each meal, oral hygiene should be performed with clean water in smaller children and oral antiseptic mouthwash for older ones. Brushing of the teeth should be continued and performed gently.
DISCUSSION
The multidisciplinary approach to cleft patients is considered the ideal treatment. It is increasingly necessary to be aware of concepts and procedures related to the different specialties that work toward improving conditions for lip and/or palate cleft patients (4,5) .
The increase in the number of patients seen and specialists involved in this type of care at HUCFF has made it possible to improve the quality of the results obtained. In addition, technical details not formerly used, have simplified tissue handling and decreased aggressiveness of intra and postoperative care.
The plastic surgeon is usually considered responsible for the general treatment by family members and patients with clefts(S): the person that actually deals with the deformity. This is true to a certain extent, although we should take into account the opinion and participation of other specialists so as not to go astray by losing the necessary interdisciplinarity for adequate follow-up.
During the intraoperative period, we should pay attention to the facts that may interfere in performing a satisfactory surgery.
Orotracheal tube fixation should not deviate commissures, interfering in lip flap marking. In palatoplasties, the ulbe should fo llow the median line of the tongue up to the vallecula, otherwise, it can deviate and fall on to the surgical field while positioning the mouth gag. Putting rubber between the tongue depressor and teeth reduces the pressure on the tongue and avoids the tube being pressured, especially if we are not using an armored tube.
The Rose position and pharyngeal packing avoid blood and secretion descending the trachea(6).
We must not forget that the anesthetic handling of children is much more prone to variations than that of adults. The possibility of complications is greater and real, as the patient is more unstable and the anesthetist does not have direct access to airways. All of this helps increase the stress and attention necessary to the procedure. Thus, respecting this condition is vital to the understanding of the team and control of the patient.
Anesthetic infiltration for cheiloplasties should not be excessive, leading to the risk of deforming the lip and ending the procedure with asymmetries.
Some do not infiltrate solution at all during cheiloplasty and obtain very satisfactory results evident in the immediate postoperative period. In these cases, despite the absence of vasoconstrictors, an exaggerated increase in bleeding is not observed.
Millard's technique for unilateral cheiloplasty has proved to be a good option. We obtain adequate tissue mobility and final symmetry even for wide clefts.
In order to attain satisfactory symmetry, it is essential that initial flap marking be well performed. It is better to spend a little more time checking markings, than have trouble in obtaining balance after the flaps are incised. A practical way for measuring flaps is using Halstead forceps. We use a small segment of the same suture that will be used for the McComb sutures (vicryl rapide® 4-0). We measure the normal filtral crest and transfer the marking. It is interesting that the adequate movement of the forceps makes the suture present a curvature that imitates flap markings. Moreover, we carefully follow the extension of the filtral crest that will be reconstructed comparing it to the normal crest.
Whenever we foresee difficulties for obtaining the right height for the lip in reconstruction, we may choose Millard II technique and/or add a small triangular flap near the vermillion that inserts itself in the rotating flap, lengthening it.
Flaps are incised, released and mobilized in a conventional fashion, emphasizing subperiosteal detachment at the base of the cleft nostril, allowing large mobilization of the nostril base, easing balance. Detachment of the nasal dorsum follows the subcutaneous plane, as recommended by McComb.
Sutures with small delicate, resistant and sharp needles have eased repositioning and suture of structures. Needle standards fit exactly into the existing needs of surgeries for clefts, bearing out the fact that, the greater the accuracy and less aggressiveness imposed upon tissues, the better is their recovery.
The utilization of absorbable synthesis material has made postoperative care much easier. Everyone that works with children knows the difficulties of removing sutures and cleaning wounds, particularly in babies.
Sutures used on skin are absorbed fast and begin to loosen in a week, avoiding external marks. On the other hand, mucosa sutures, performed with monocryl®, are absorbed slower, have a considerable tensile force (30%) at 14 days, and loosen after 3 weeks.
In a significant number of cases, in which there is no considerable tension for skin synthesis, we use skin adhesives (dermabond®). It proved to be a good option. It is easy and fast to use and is generally a positive surprise for patients' family members. The film over the wound still keeps it clean and protected. We have not observed dehiscence even in more active children. The tape should not be wet excessively, but daily routine does not call for changes.
The nasal support sutures described by McComb are a major detail. As the surure hook invaginates and runs externally, we do not use any type of skin cushion. Some authors use padded sutures, although a segment of gauze, frequently hardened by blood, may compress the skin and lead to ulcerations. We thus avoid the possibility of skin injury. We do not use padded sutures on the inner surface of the nostril either. The knot is in direct contact with the skin. It is important that there is no tension on the suture, because it can affect surrounding skin. The objective of the supporting surures is to keep strucrures in the position reached after skin detachment, and not to traction nostrils. As the suture used is absorbed fast, after 10 to 14 days it begins to loosen. Again, there is no need to submit the child to suture removal.
Special attention should be given to approximating skin borders, mainly at the cutaneous-mucosa junction. Anesthetic infiltration, edema and the tiny size of structures may lead to asymmetric sutures, not perceived immediately, although embarrassing in the late postoperative period. A magnifying glass should be used for better visualization, if necessary.
In palatoplasties, we infiltrate a slightly larger volume of anesthetic to expand tissues and malce their approximation easier. We prefer to infiltrate the segment that will be handled instead of infiltrating the whole palate at once. In this fashion we infiltrate the nasal mucosa and detach it; we follow with infiltration of the area of muscular detachment and perform it; and, last, we infiltrate the whole oral flap and release it. On the infiltration area on the hard palate, we prefer to use a Carpule syringe which provides ease and a steady flow of the volume infiltrated. With this routine, we take advantage of the mechanical expansion of the anesthetic to make detaching flaps easier. We have not observed increased bleeding because we do not wait long enough for the adrenalin vasoconstrictor effect to occur.
We prefer to surure the nasal mucosa before total palate detachment, particularly if ample mucoperiosteal flap detachment is necessary. After complete palate detachment, structures present more bleeding and overlay easily, malcing synthesis more difficult. By suturing the nasal mucosa right after detachment we avoid these drawbacks and give tension to the soft palate, which eases muscle release.
Detachments should be performed firmly, but also delicately. The strucrures may be firmly adhered to deep planes and, at the same time, present little resistance. Detachers of various shapes are used according to the area to be mobilized and should be sharp enough to make detachment easy without however risking accidental cutting of structures.
Utilization of absorbable monofilament suture, with a small sharp needle has made palatal sutures easier. The size of the needle proved to be adequate for use in such a tiny space. The availability of a compound curvature needle is especially significant, above all for complete palatal clefts in ogival-shaped palates, where access and a synthesis of the anterior portion always is a major technical difficulty. This difficulty is more easily overcome with that needle.
Palatal hemostatic absorbable packing (surgicel®) has greatly improved hemostasia and oral postoperative hygiene. Surgicel® is easy to handle, offers adeguate hemostasia, avoids foul odor during the postoperative period and does not need to be removed, as it is absorbed in a few days. Current conditions are quite different from a non distant past in which we used packaging with ointment dressings that left a characteristically offensive breath and needed to be removed after a few days. In older patients in whom palate bleeding is more abundant and can become a problem, we add a compressive dressing to the palate. In these cases, we should care not to use a very large volume of gauze compressing the palate, because it can stimulate vomiting. Compression should not be excessive so as not to lead to ischemia of palate flaps.
These technical details incorporated into our routine have led to better patient control in the intraoperative period and have made handling tissues and postoperative care easier, particularly for family members. Children would certainly be thankful if they knew what they were being spared.
Technological advances that were not formerly available have made things easier. The guality of results has improved. This is probably due mainly to the increased number of patients seen and the professionals responsible for this kind of care. We cannot deny, however that adeguate material enhances our working skills.
Last, it is important that those beginning in the specialty assess the information obtained and use it in the best possible way. It would be ideal to work with evidence-based medicine, that is to say, do what has been scientifically proven to be best. The problem with treating clefts is that there are various indications of good results, some of which are conflicting. Our own observations and the ability to use them should be added to evidence.
REFERENCES
1. Millard DR Jr. The primary camouflage of the unilateral harelip. In: Skoog T and Ivy RH, eds. Transactions of the International Society of Plastic Surgeons, 1st Congress, Stockholm, 1955. Baltimore: Williams & Wilkins. 1957; 160-6.
2. McComb HK, Coghlan BA. Primary repair of the unilateral cleft lip nose: completion of a longitudinal study. Cleft Palate Craniofac J. 1996 Jan; 33(1):23-30.
3. Rocha, DL. Fissuras bilaterais: tratamento cirurgico pela tecnica de Spina. In: Carreirao S, Lessa S, Zanini SA. Tratamento das fissuras labiopalatinas. 2. ed. Rio de Janeiro: Revinter; 1996.
4. Franco T, Franco D, Cintra H. Malformacões congênitas. In: Franco T, Franco D, Gonc;alves LFF. Princápios de cirurgia phástica. Rio de Janeiro: Editora Atheneu; 2002. p. 301-54.
5. Oliveira DFV Fendas labiopalatais: tratamento multidisciplinar [Dissertação Mestrado J. Rio de Janeiro: UFRJ; 2000.
6. Garambone MA, Sardenberg KM, Ferreira EC, Kreimer G. Anestesia para Operacções de Lábio e Palato. In: Tratamento das fissuras labiopalatinas. 2. ed. Rio de Janeiro: Editora Revinter; 1996.
I - Member of the Plastic Surgery Service of Hospital Universitário Clementino Fraga Filho, Universidade Federal do Rio de Janeiro (UFRJ). Master in Plastic Surgery by UFRJ. Senior Member of SBCP; TCBC; FICS. II - Resident physician of the service.
Work perfonned at the Plastic Surgery Service of Hospital Universitário Clementino Fraga Filho, Universidade Federal do Rio de Janeiro.
Address for correspondence:
Praia de Botafogo, 528 apto. 1304-A
22250-040 -Rio de Janeiro -RJ Brazil
e-mail: diogo@openlink.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter