

Articles - Year 2003 - Volume 18 -
Total Reconstruction of the Lower Lip with Face Flaps
Reconstrução Total do Lábio Inferior com Retalhos de Face
ABSTRACT
The use of flaps from the face is indicated for total reconstruction of the lower lip, even when the primary lesion goes beyond its anatomical boundaries. The authors present three patients with spinocellular carcinoma of the lower lip, whose lesions were greater than 4.0 cm in their larger diameter; and who underwent total reconstruction ofthe lower lip.
Keywords: Lip-tumors; lower lip-surgery; face flaps
RESUMO
A utilização de retalhos localizados na face é indicada na reconstrução total do lábio inferior, mesmo quando a lesão primária vai além do seu limite anatômico.
Apresentamos três pacientes portadores de carcinoma espinocelular do lábio inferior, com lesões acima de 4,0 cm no seu maior diâmetro, nos quais a reconstrução total foi realizada.
Palavras-chave: Lábio - tumores; lábio inferior - cirurgia; retalhos de face
In lower lip deformities resulting from tumor resections, face flaps are the first choice for reconstruction. The proximity of the donor and receptor sites favors positive aesthetic and functional outcomes.
It is necessary to know the anatomy of the lower lip in order to indicate the appropriate technique for its reconstruction. The sphincter component (closing) of the lip is performed by the circular or semicircular fibers of the orbicularis oris muscle of the mouth helped by the mentalis muscle. The dilating component (opening) is performed by the radial fibers of several facial muscles: levator labii superioris alaeque nasi, levator labii superioris, zygomaticus major, buccinator, depressor anguli oris, depressor labii inferioris, levantor anguli oris (Fig. 1). Irrigation is performed by the facial artery, whose upper and lower labial arteries anastomose (Fig. 2). Lymph is drained to the submandibular and submental lymph nodes. Sensitive innervation of the upper lip is provided by the infraorbital nerve and in the lower lip, by the mentalis nerve. Motor innervation is provided by the facial nerve.

Fig. 1 - Upper and lower lip muscles.
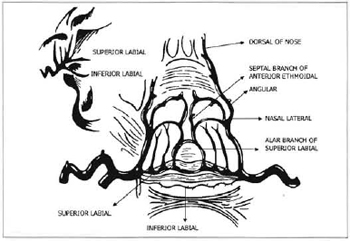
Fig. 2 - Arterial vascularization of the upper and lower lips.
Even though there are techniques like Barron's & Saad's(l), who, in 1990, described the use of platysma musculocutaneous flaps for the total reconstruction of the lower lip, with good results, and others like Tobin's(2) (1990), who used the depressor labii inferioris muscle, the techniques that use facial arterial cutaneous flaps with innervated muscles are still performed today. Osteomusculocutaneous flaps with a microsurgical approach are used when the area to be reconstructed extends to the region of the mandible and chin. Today's challenge is the recovery of the movements of the lower lip, as the motor function of the orbicular muscle is difficult to recover.
The objective of this paper is to show that the use of facial flaps is indicated for total reconstruction of the lower lip, even when the primary lesion goes beyond its anatomical limits.
BACKGROUND
Dieffenbach(3), in 1834, described a technique for lower lip reconstruction using large full-thickness rectangular cheek flaps, which advanced to each of the sides of the face.
Bürow(4), in 1838, suggested the resection of skin and subcutaneous triangles, laterally to the nasolabial fold, to facilitate the advancement of cheek flaps for lower lip reconstruction.
Camile Bernard(5), in 1853, described a technique which extended the principle of advancement of lateral flaps.
Scymanowski(6), in 1858, changed Dieffenbach's(3) technique, suggesting the use of cheek flaps, laterally to the nasolabial fold, for total reconstruction of the lower lip.
Webster(7), in 1960, made an addition to Camile Bernard's(5) technique of longitudinal incisions that originated in the labial conunissures and other parallel structures starting at the level of the chin. This provided the correction of the excess tissue in the central region of the chin.
Karapandzic(8), in 1974, proposed the use of a rotation flap, starting at the nasolabial fold opposite to the defect, encompassing full thickness of the cheek. This technique offered good aesthetical and functional results for losses of up to ¾ of the lip.
Scymanowski's(6) technique was changed by Fujimore(9) in 1980, in a technique called "Gate Flap", due to the manner in which nasolabial flaps adjusted to reconstruct the lower lip (Figs. 3 and 4).

Fig. 3 - Fujimore technigue(9) Marked flaps. The distance OB=O'B' ranges from 0.5 cm to 1.0 cm or to 2 cm in elderly patients. The distance BC=B'C' is 3 cm. AB, A'B', AC, A'C' incisions are in full thickness and CE, C'E', ED, E'D', only on the skin and subcutaneous. The dotted lines correspond to excess mucosa used in the reconstruction of the lip-alveolar fold and lip vermillion.

Fig. 4 - Fujimore technigue. Flaps after transposition.
Barron & Saad(l), in 1990, described the use of the platysma musculocutaneous flap for total lower lip reconstruction.
Tellioglu(10), in 1997, published a paper in which he suggested combining the depressor labii inferioris muscle with a free microsurgical flap from the forearm (radial flap), for total reconstruction of the lower lip. He said that the depressor labii inferioris muscle replaced the sphincter of the orbicularis muscle. He also said that the sensitivity of the radial flap was provided by the neurorhaphy of the sensitive nerve of the flap with the mentalis nerve.
In 2000, Miguel Sabino Neto(1) at al. published a paper suggesting the use of a flap formed by the depressor labii inferioris muscle combined with a cutaneous island for lower lip reconstruction, a technique already described by Tobin(l4), in 1990. They provided excellent aesthetic and functional results for 18 patients.
CASES AND METHODS
3 patients with lower lip spinocellular carcinoma were selected for this study, all of them with tumors greater than 4 cm in the larger diameter.
CASE #1
92-year-old white female patient, from the state of Bahia, with a vegetative lesion in the lower lip whose larger diameters measured 5.0 x 2.0 x 1.5 cm, without palpable cervical lymph nodes (Figs. 5,6 and 7).
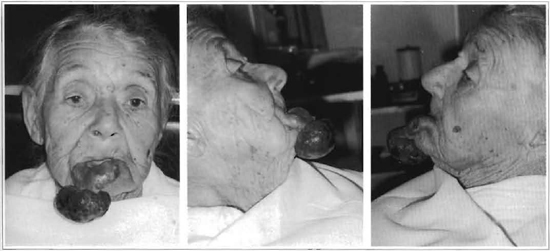
Figs. 5, 6 and 7 - Patient preoperative (case # 1).
The lesion was resected under local anesthesia with, a safety margin of approximately 1.0 cm. Reconstruction was performed according to Camile Bernard's(5) technique, using flaps from the cheeks, through longitudinal incisions in the skin and muscles starting on the labial commissures, associated to other parallel structures in the mucosa, superiorly located at approximately 0.8 cm, thus leaving enough mucosa for the reconstruction of the vermillion. The central region of the lip and chin was also closed without tension, thanks to the resection of skin and subcutaneous triangles a , laterally to the nasolabial fold.
CASE #2
58-year-old white male patient, from the state of A1agoas, with an ulcerated lesion in the lower lip measuring 4.0 x 1.5 x 0.9 cm in its larger diameters, with palpable bilateral submandibular lymph nodes. A thin needle was used to puncture a left submandibular node, and aspiration confirmed the existence of spinocellular carcinoma metastases (Figs. 8,9 and 10).
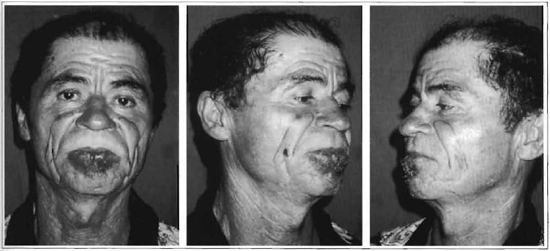
Figs. 8, 9 and 10 - Patient preoperative (case # 2).
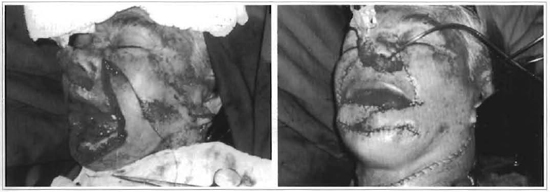
Bilateral supra-omohyoid cervical emptying was performed. Next, the lesion was resected with a safety margin of 1.0 cm, encompassing the entire lower lip. Reconstruction was performed according to Fujimore's(9) technique (Figs. 11 and 12).

Figs. 11 and 12 -Transoperative and recent postoperative of the patient (case # 2).
CASE #3
A 75-year-old white female patient, from the state of Bahia, with an ulcerated and vegetative lesion in the lower lip measuring 8.0 x 2.5 x 1.0 cm in its largest diameters, with bilateral submandibular lymph nodes (Figs. 13, 14 and 15). Bilateral supra-omohyoid cervical emptying was performed. Next, the lesion was resected, with a safety margin of 1.0 cm, encompassing the entire lower lip; marginal resection of the mandible at the level of the chin was also performed. Reconstruction followed Fujimore's technique(9), associated with the advancement of cervical cutaneous flap to help the reconstruction of the chin, and a tongue flap to reconstruct the vermillion. (Figs. 16 and 17).
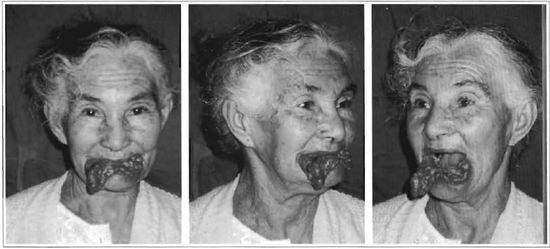
Figs. 13,14 and 15 -Patient preoperative (case # 3).
Figs. 16 and 17 - Patient transoperative (case # 3).
RESULTS
In case # 1, which was performed with local anesthesia, the patient was discharged on the 3rd postoperative day. Six months after the surgery, she was asymptomatic, with satisfactory aesthetic and functional results (Figs. 18 a 21).

Figs. 18 and 21 - Patient postoperative (case # 1).
In the other two cases, the nasogastric tube was removed on the 6th, day and patients were discharged on the 7th postoperative day. The histological examination of the lesion diagnosed spinocellular carcinoma and resection margins were free from neoplasia in all the cases. In case # 2, the histological examination of the material from cervical emptying identified metastases of spinocellular carcinoma in five out of nine lymph nodes, and in case # 3, in one lymph node out of eighteen. In case # 3, the histological examination of mandible fragments identified invasive spinocellular carcinoma. The pedicle of the tongue flap used in case # 3 was sectioned on the 15th day after hospital discharge. Six months (case # 3) and 1 year (case # 2) after surgery, patients were asymptomatic, presenting good aesthetic and functional results (Figs. 22 to 29).

Figs. 22 to 25 - Postoperative of patient (case # 2).

Figs. 26 to 29 - Postoperative of parient (case # 3).
DISCUSSION
The first techniques described for the correction of lower lip defects resulting from tumor resections were performed with face flaps.
The techniques of Bernard(5) (1852), Estlander(12) (1852), Abbe(13) (1898), Gillies(14) (1920), Webster(7) (1960), and Karapancizic(8) (1974), which recommended the use of face flaps, are still performed today along with other techniques. Fujimore's technique(9), described in 1980, used flaps from the nasolabial fold similar to those described by Scymanowski(6), in 1858. The suggested changes provided: a) an increase in the width of the flaps and in their distance to the labial commissure, thus allowing more tissue for the new lip; b) axial flaps, with preservation of blood vessels starting on the labial commissure; c) reconstruction of the lip vermillion and lip-alveolar fold using cheek mucosa.
The author highlighted the following advantages:
1. The flap can be 3 cm wider than rotation nasolabial flaps.
2. Rotating the flap is possible without forming excess skin at its base.
3. The flap contains innervated muscle.
4. The procedure can be performed in a single stage.
Today, in spite ofthe evolution of reconstructions with microsurgical flaps, there is a preference for the use of face flaps due to: a) proximity to tissues; b) their similarity; c) easier surgical technique. When tumors relapse, depending on their extension, or when tissues do not offer safe conditions for reconstruction, there is an indication for flaps from outside the anatomical limits of the face . Distant flaps would thus always be a second choice.
CONCLUSION
We therefore conclude that:
a) Total reconstruction of the lower lip can be performed using only flaps from the face;
b) When the area to be reconstructed goes beyond the anatomical borders of the lower lip, reconstruction can be performed with face flaps combined with flaps from adjacent regions;
c) Tongue and neck flaps combined with face flaps favor good aesthetic and functional outcome.
REFERENCES
1. Barron JN & Saad MN. Platysma musculocutaneous flap to the lower lip. In: B. Strauch LO. Vasconez, and EJ. Hail-FindJay (Eds.), Grabb's Encyclopedia of Flaps, Vol. 1. Boston: Little, Brown & CO; 1990. p. 989-93.
2. Tobin GR. Funtional lower lip and oral sphinter reconstruction with innervated depresor anguli oris flap hair-bearing skin flap. In: Grabb's Encyclopedia of Flaps, 1. ed. Boston: Little, Brown & CO; 1990. p. 665-9.
3. Dieffenbach JF. Chirurgische Erfahrungen, besonders ueber die Wiederherstellung Zerstoerter Theile des menschlichen Koerpers nach neuen methoden. Berlim: T.C.F Enslin; 1829. p. 34-8.
4. Burow A. Zur Blepharoplastik. Monatsschr. Med Augenheilkd Chir. 1838; 1:57-61.
5. Bernard C. Cancer de la levre inferieur opere par un proce-de nouveau. Bull Soc Chir Paris. 1853; 3:357-60.
6. Scymanowski J von. Zur plastichen Chirurgie. Vrtljschr Prakt Heilk. 1858; 60:152-7.
7. Webster RC, Coffey RJ, Kelleber RE. Total and partial reconstruction of the lower lip with innervated muscle bearing flaps . Plast Reconstr Surg. 1960; 25:360-71.
8. Karapandzik M. Reconstruction of the lip defects by local arterial flaps . Br JPlast Surg. 1974; 27:937.
9. Fujimore R. "Gate flap" for the total reconstruction of the lower lip. Br J Plast Surg. 1980; 33:340-7.
10. Tellioglu AT, Akyüz M. Functional reconstruction of total lower lip defects with a radial forearm free flap combined with a depressor anguli muscle transfer. Ann Plast Surg. 1998; 40(3) :310-1.
11. Sabino Neto M, Garcia EB, Castilho HT, Ferreira LM, Hochberg J, Toledo SR. Utilization of Depressor Anguli Oris Musculocutaneous Flap for Lip Reconstruction. Ann Plast Surg. 2000; 44(1):23-8.
12. Estlander JA. Eeine Method, aus der einen Lippe Substanzverluste der anderen zu ersetzen. Arch Klin Chir. 1872; 14:622-6.
13. Abbe R. A new plastic operation for relief of deformity due to double harelip. Med Rec New York. 1898; 53:477-51.
14. Gillies HD, Millard R. Principles and art of plastic surgery. Boston: Little, Brown & Co; 1957. p. 507-8.
I - Master in Plastic Surgery, Universidade Federal de Sao Paulo - Escola Paulista de Medicina (UNIFESP-EPM), plastic surgeon of the Hospital Municipal Infantil Menino Jesus, São Paulo.
II - Doctor of Medicine, UNIFESP-EPM.
III - Head Professor of Plastic Surgery at UNIFESP-EPM Surgery Department.
IV - Professor of Otorhinolaryngology at UNIFESP-EPM.
Escola Paulista de Medicina da Universidade Federal de São Paulo. Surgery Department - Discipline of Plastic Surgery and Otorhinolaryngology Department - Head and Neck Surgery Sector.
Address for correspondence:
R. Manoel da Nobrega, 277
04614-000 -São Paulo -SP Brazil
Fone: (55 11) 5543-9451 -Fax: (55 11) 5532-1677
e-mail: bca2000@llol.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter