

Original Article - Year 2024 - Volume 39 -
Flankplasty systematization based on surgical anatomy
Sistematização de flancoplastia baseada na anatomia cirúrgica
ABSTRACT
Introduction: The study explores body contouring surgery in patients undergoing bariatric surgery. In recent years, this type of surgical intervention has gained prominence due to the increase in the search for reparative procedures after significant weight loss. The text emphasizes the importance of flankplasty, a technique that aims to improve body contour.
Methods: A literature review was carried out to elucidate the anatomy of the deep fat of the thoracolumbar fascia, and a parallel was made with the flankplasty technique used in our service in post-bariatric patients undergoing 360° or 270° abdominoplasty at Daher Lago Sul Hospital, in Brasília-DF.
Results: Deep liposuction of the flanks, often necessary in body contouring surgeries, may not be sufficient to remove fat deep into the thoracolumbar fascia and during this procedure, there is an increased risk of retroperitoneal injuries. However, flankplasty, which involves resection of fat deep into the thoracolumbar fascia, has been shown to provide satisfactory results and minimize these risks.
Conclusion: The study focuses on the importance of precise anatomical knowledge, highlighting the relevance of flankplasty as a valuable technique to improve aesthetic results and reduce complications in post-bariatric patients, complementing bariatric surgery and improving the patient's quality of life.
Keywords: Plastic surgery procedures; Body contouring; Body image; Subcutaneous fat, abdominal; Adipose tissue; Anatomy; Lipectomy
RESUMO
Introdução: O estudo explora a cirurgia de contorno corporal em pacientes submetidos a cirurgias bariátricas. Nos últimos anos, esse tipo de intervenção cirúrgica ganhou destaque devido ao aumento na busca por procedimentos reparadores após significativa perda de peso. O texto enfatiza a importância da flancoplastia, técnica que visa melhorar o contorno corporal.
Métodos: Foi realizada revisão da literatura para elucidação da anatomia da gordura profunda da fáscia toracolombar, e feito um paralelo com a técnica de flancoplastia utilizada em nosso serviço em pacientes pós-bariátricos submetidos a abdominoplastia 360° ou 270° no Hospital Daher Lago Sul, em Brasília- DF.
Resultados: A lipoaspiração profunda dos flancos, muitas vezes necessária em cirurgias de contorno corporal, pode não ser suficiente para retirar a gordura profunda à fáscia toracolombar e durante esse procedimento observa-se risco aumentado de lesões retroperitoneais. No entanto, a flancoplastia, que envolve a ressecção da gordura profunda à fáscia toracolombar, demonstrou proporcionar resultados satisfatórios e minimizar esses riscos.
Conclusão: O estudo enfoca a importância do conhecimento anatômico preciso, destacando a relevância da flancoplastia como uma técnica valiosa para melhorar os resultados estéticos e reduzir complicações em pacientes pós-bariátricos, complementando a cirurgia bariátrica e melhorando a qualidade de vida do paciente.
Palavras-chave: Procedimentos de cirurgia plástica; Contorno corporal; Imagem corporal; Gordura subcutânea abdominal; Tecido adiposo; Anatomia; Lipectomia
INTRODUCTION
Body contouring surgery has gained a lot of attention in recent years due to the increase in the number of patients undergoing bariatric surgery, who develop significant weight loss and body dysmorphism and subsequently seek out the plastic surgery team to perform reconstructive surgery1.In 1940, Somalo pioneered the term “Belt Lipectomy”, but with little detachment of the abdominal wall2. In 1961, Gonzalez-Ulloa described, in detail, circumferential abdominoplasty, which involves the anterior and posterior approach to the abdomen, flank, waist, culottes, and buttocks regions1.
It is observed that post-bariatric patients have significant skin flaccidity, associated, despite great weight loss, with fat accumulation in deep regions3. Furthermore, such patients tend to have poorer skin contractility, due to stretching of the skin and damage to elastic fibers, either due to excessive weight loss or skin aging. Therefore, we use a combination of surgical techniques in search of improving body contour4.
Lockwood contributed to major developments in circumferential abdominoplasty techniques when he described high lateral tension abdominoplasty in 1995, highlighting that soft tissue laxity was a direct component in the results of this surgery and should be treated with increased lateral skin resection, repair of the superficial fascial and significant liposuction of the back and flank whenever necessary. Recognizing, therefore, that the entire trunk should be treated as an aesthetic unit5.
When analyzing the anatomy of the flank region, Lockwood mentions the superficial fascia that separates superficial fat from deep fat, generating areas of adhesion in the trunk and being an important anatomical reference for the body surface. The author states that it is possible to observe anatomical variations of this fascia between male and female patients and between lean and obese patients6.
OBJECTIVE
The objective of the study is to detail the anatomy of the thoracolumbar fascia and describe the flankplasty technique performed in our plastic surgery service, to improve body contour in patients undergoing circumferential abdominoplasty.
METHOD
A review of the literature was carried out to better elucidate the anatomical region that involves the fat deep into the thoracolumbar fascia. A parallel was then made with the flankplasty technique routinely performed in our plastic surgery service at Hospital Daher Lago Sul, in Brasília-DF, for post-bariatric patients undergoing 360º or 270º abdominoplasty. Tomographic exams were correlated with what was found intraoperatively in these patients.
This project was approved by the Ethics and Research Committee of Hospital Daher Lago Sul and registered on Plataforma Brasil under number CAAE: 68265323.9.0000.0257(http://aplicacap.saude.gov.br/plataformabrasil).
RESULTS
Much is known about the anatomy of the abdominal muscles, but little is mentioned about the thoracolumbar fascia in the literature. The thoracolumbar fascia is a deep-lining connective tissue membrane that extends from the subdermal plane to the underlying muscular fascia, covering the deep muscles of the posterior part of the trunk, involving superficial and deep fat in well-defined compartments. It is present from the thoracic region, where it is strongly adhered to the musculoskeletal surface, providing areas of adherence7.
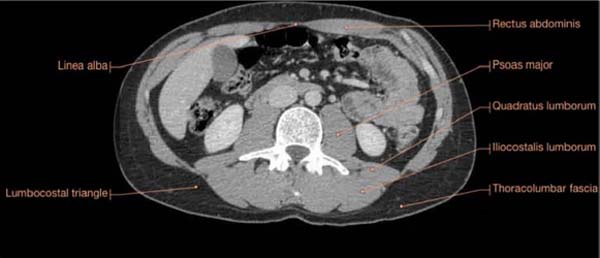
The lumbocostal triangle is delimited by the thoracolumbar fascia and is located above the lumbar muscles. This region is easily visualized on abdominal computed tomography or magnetic resonance imaging, with tomography being a routine exam requested preoperatively for patients who will undergo circumferential abdominoplasty in our service (Figure 1).
Anatomically, the lower back has denser and more abundant adipose tissue, which makes liposuction of the region difficult and increases the risk of perforation of organs such as the kidneys. The kidneys are retroperitoneal and protected only by perirenal and pararenal fat, perirenal fascia, and the abdominal wall on its posterior surface, composed of the psoas major and minor muscles, quadratus lumborum muscle, latissimus dorsi muscle, thoracolumbar aponeurosis and a considerable amount of interposed posterior adipose tissue located in the superficial fascia7.
Petit’s triangle is located in the lower and lateral part of the lumbar region and limited inferiorly by the iliac crest, laterally by the inferior border of the external oblique muscle of the abdomen, and medially by the anterior border of the latissimus dorsi muscle. Therefore, it is a region of greater exposure and danger during flank liposuction7.
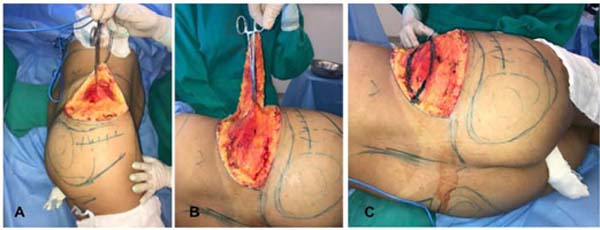
Such anatomical factors make deep flank liposuction more complex, as there is a greater chance of retroperitoneal perforations when compared to flankplasty. Furthermore, it is fat with a more adherent and dense appearance, less fluid than the fat observed in the anterior abdominal region, located in a deep topography, and with difficult angulation for the liposuction cannulas (Figure 2).
In the pre-operative period of the patient who will undergo 360º or 270º abdominoplasty, it is possible to observe, during palpation, whether there will be a need to associate flankplasty to improve body contour. Surgical markings are routinely performed with the patient in an upright position and completed after anesthetic induction, following the usual markings for an extended abdominoplasty. All patients are operated on under general anesthesia.
Intraoperatively, as a routine in our service, we begin the surgery with liposculpture. After this step, the 360º or 270º abdominoplasty begins with the patient in the prone or lateral decubitus position, respectively. The incision and dissection of the surgical planes are performed, making it possible to identify the thoracolumbar fascia and the projection of deep fat that will be excised (Figures 3A and 3B). The area to be excised is then marked with methylene blue and resected (Figure 3C). Afterward, the remaining stages of body contouring surgery are performed, with the traction of the dermal-fat flap and suturing in layers: fatty flap with Nylon 3.0 thread and simple inverted stitches, subdermal with Nylon 4.0 thread with simple inverted stitches, and intradermal with Nylon 3.0 thread with continuous points (Figure 4).
All patients receive a fat injection in the buttocks, with a variable volume depending on each case, but always in a subcutaneous plane and with fat retroinjection. A vacuum drain is placed bilaterally with incisions in the inguinal fold and directed to the posterior region, fixed with Nylon 4.0 and ballerina stitches. All patients undergo prophylaxis for deep vein thrombosis and pulmonary embolism intraoperatively with a pneumatic compressor and postoperatively with subcutaneous enoxaparin 40 mg, once a day, for seven days, starting on the first day after surgery, in addition to early ambulation. Figure 5 shows the pre- and 6th month post-operative results of a patient undergoing this technique.
DISCUSSION
The increased incidence of obesity in contemporary times, combined with the effectiveness of surgical treatment through bariatric surgery, results in rapid weight loss with aesthetic and functional consequences that require surgical correction to ensure improvements in the patient’s quality of life8. Abdominoplasty associated with flankplasty is performed to restore body contour and improve individual deformities in post-bariatric patients who present flaccidity, tissue redundancy and lipodystrophy of the flank region. Therefore, reconstructive plastic surgery increases and complements the results of bariatric surgery, generating improvements in the patient’s physical and psychological impacts9.
Circumferential abdominoplasty is characterized by extended incisions completing 360º to circumferentially remodel all sagging tissue present in the abdominal region, flank, side of the thigh, back, and buttocks at the same surgical time, as well as achieving simultaneous remodeling of the skin4.
Flank liposuction and flankplasty are complementary surgeries to abdominoplasty. Flank lipoabdominoplasty is indicated when there is no excess skin on the abdominal sides and in most surgeries, it already shows good results. However, patients who have severe skin laxity require additional procedures to obtain a better result, as observed by Cintra et al.10 in their 10-year case study. The fact that the upper skin flap is more adherent than the lower flap allows this procedure to generate an elevation of the gluteal region.
Sergio Levy Silva11, in his work on anatomical variations of subcutaneous cellular tissue after weight loss, observed that bariatric patients presented macroscopic and histological variations of the areolar and lamellar layers, in addition to a structural discontinuity of the superficial fascia, which led to an increased risk of perforation during deep liposuction.
Therefore, knowing the anatomy of this region allows for better therapeutic decisions and minimizes the risk of intraoperative complications, such as injuries to retroperitoneal organs or vascular injuries.
Little is mentioned in the literature about the excision of deep fat from the thoracolumbar fascia as a surgical procedure for flankplasty, in addition to its more adherent characteristic and less susceptibility to liposuction. In our service, it was observed that this association brings improvements in the results of patients undergoing abdominoplasty with extended incisions (Figure 5).
CONCLUSION
In-depth knowledge of the anatomy of the abdominal region and flanks allows for a better surgical strategy when planning body contouring surgery, especially for patients who have suffered major weight loss. Resecting part of the fat deep to the thoracolumbar fascia located on the flanks, when properly indicated, generates more satisfactory results and minimizes the risks associated with deep liposuction in this region.
REFERENCES
1. Aly A, Mueller M. Circumferential truncal contouring: the belt lipectomy. Clin Plast Surg. 2014;41(4):765-74. DOI: 10.1016/j. cps.2014.06.008
2. Somalo M. Dermolipectomia circular del tronco. Sem Med. 1940;47:1435.
3. Gemperli R, Munhoz AM, Marques Neto AA. Fundamentos da Cirurgia Plástica. Rio de Janeiro: Thieme Brasil; 2016.
4. Richter D F, Stoff A. Circumferential body contouring: the lower body lift. Clin Plast Surg. 2014;41(4):775-88. DOI: 10.1016/j. cps.2014.07.004
5. Lockwood T. High-lateral-tension abdominoplasty with superficial fascial system suspension. Plast Reconstr Surg. 1995;96(3):603-15. DOI: 10.1097/00006534- 199509000-00012
6. Lockwood TE. Superficial fascial system (SFS) of the trunk and extremities: a new concept. Plast Reconstr Surg. 1991;87(6):1009-18. DOI: 10.1097/00006534-199106000-00001
7. Sabiston DC, Townsend CM Jr, Beuchamp RD, Everds BM, Mattox KL. Sabiston tratado de cirurgia: A Base Biológica da Prática Cirúrgica Moderna. 20ª ed. Rio de Janeiro: Guanabara Koogan; 2019. p. 1085-6.
8. Cintra Junior W, Modolin MLA, Colferai DR, Rocha RI, Gemperli R. Post-bariatric body contouring surgery: analysis of complications in 180 consecutive patients. Rev Col Bras Cir. 2021;48:e20202638. DOI: 10.1590/0100-6991e-20202638
9. Andrade M V, Barbosa EC, Lauck AJM, Noleto DC, Freitas TVM, Hartmann AA. Abdominoplastia pós-bariátrica: os impactos na saúde, na qualidade de vida e no bem estar social do paciente. Rev Educ Saúde. 2021;9(Supl 1):8.
10. Cintra W, Modolin M, Rocha RI, Gemperli R. Abdominoplastia circunferencial simples e composta: evolução técnica, experiência de 10 anos e análise das complicações. Rev Bras Cir Plást. 2021;36(1):21-7.
11. Silva SL. Variações anatômicas do tecido celular subcutâneo pós-perda ponderal. Rev Bras Cir Plást. 2010;25(4):675-8. DOI: 10.1590/S1983-51752010000400020
1. Hospital Daher Lago Sul, Plastic Surgery -
Brasilia - Distrito Federal - Brazil
Corresponding author: Marcela Santos Vilela SHIS QI 25 Conjunto 11 Casa 10, Lago Sul, Brasília, D F, Brasil. CEP: 71660-310 E-mail: marcelasvilela@gmail.com
Article received: September 15, 2023.
Article accepted: April 30, 2024.
Conflicts of interest: none.











 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter