

Original Article - Year 2024 - Volume 39 -
Surgical treatment of keloids: Total or partial resection?
Tratamento cirúrgico de queloides: Ressecção total ou parcial?
ABSTRACT
Introduction: Currently, the application of intralesional triamcinolone with surgical excision is considered the most satisfactory treatment for keloids, with a low recurrence rate.
Method: A case study was carried out covering reconstructive surgeries for patients with bilateral earlobe keloids, operated by the same plastic surgeon from July 2018 to January 2021 at the Hospital Regional de Sobradinho in Brasília-DF. The keloid scar (intralesional) was partially resected, leaving keloid margins in the surgical wound, and compared with the response after total resection (juxtalesional) of another scar in the same patient. Triamcinolone was applied preoperatively, with a total of 4 applications at intervals of 4 weeks between each session and in the immediate postoperative period, maintaining application every 30 days for 6 months. No patient had undergone previous treatments for keloids. Scars were evaluated postoperatively by the primary surgeon over a period of 12 months.
Results: Four of 11 patients had some type of recurrence, totaling 36% of recurrence in our study. Total excision of the keloid (left ear) had more recurrences than the contralateral side where a 1mm margin of keloid was left in the scar (right ear).
Conclusion: In the present study, we observed that when associated with treatment with triamcinolone pre-, intra-, and postoperatively, partial excision of the keloid presented lower rates of local recurrence when compared to total excision of the keloid.
Keywords: Keloid; Scar. Triamcinolone; Adrenal cortex hormones; Plastic Surgery Procedures.
RESUMO
Introdução: Atualmente, a aplicação de triancinolona intralesional com a excisão cirúrgica é considerada o tratamento mais satisfatório para queloides, com baixa taxa de recorrência.
Método: Realizado estudo de casos contemplando cirurgias reparadoras de pacientes com queloides em lóbulos de orelhas bilateralmente, operados pelo mesmo cirurgião plástico no período de julho de 2018 a janeiro de 2021 no Hospital Regional de Sobradinho em Brasília-DF. Ressecou-se parcialmente a cicatriz queloideana (intralesional), deixando margens de queloide na ferida operatória e comparou-se com a resposta após ressecção total (justalesional) de uma outra cicatriz em um mesmo paciente. Foi realizada aplicação de triancinolona no pré-operatório, com total de 4 aplicações a intervalos de 4 semanas entre cada sessão e no pós-operatório imediato, mantendo aplicação a cada 30 dias por 6 meses. Nenhum paciente havia realizado tratamentos prévios para queloides. As cicatrizes foram avaliadas no pós-operatório pelo cirurgião principal por um período de 12 meses.
Resultados: Quatro de 11 pacientes tiveram algum tipo de recidiva, totalizando 36% de recidiva em nosso trabalho. A excisão total do queloide (orelha esquerda) teve mais recidivas do que o lado contralateral em que foi deixada margem de 1mm de queloide na cicatriz (orelha direita).
Conclusão: No presente estudo observamos que, quando associada ao tratamento com triancinolona no pré, intra e pós-operatório, a excisão parcial do queloide apresentou menores taxas de recidiva local quando comparada à excisão total do queloide.
Palavras-chave: Queloide; Cicatriz Triancinolona; Corticosteroides; Procedimentos de cirurgia plástica
INTRODUCTION
The repair process after local trauma, whether physical or chemical, depends on the body’s inflammatory response. An exacerbated or diminished response has a significant impact on the aesthetic outcome of the postoperative wound, depending on factors such as age group, nutritional status, previous chronic diseases, drug therapies in use, cytogenetic abnormalities, and inadequate treatments1.
Little is known about the mechanisms that maintain the healing process in the inflammatory and proliferative phase, resulting in abnormal scars, including hypertrophic scars and keloids, but it is defined that the basis of keloid formation is the exaggerated and disproportionate deposition of collagen2.
Keloids are exaggerated skin scars, which go beyond the limits of the initial wound and invade normal tissue, formed in genetically predisposed people3,4. They normally appear 3 months after the trauma, do not regress spontaneously, can continue to expand, and cause great aesthetic damage2.
Currently, corticosteroid therapy is the most applied treatment for keloids, with intralesional triamcinolone being used since 19665. Its mechanism of action corresponds to inhibiting the proliferation of fibroblasts and collagen synthesis and increasing the production of collagenase, in addition to degenerating collagen nodules characteristic of keloids. keloid scar. Its application, together with surgical excision, is considered the most satisfactory treatment for keloids6. Griffith et al.5 reported in their studies the low recurrence rate of the association of surgical excision of keloids with triamcinolone injections, which guided our research.
OBJECTIVE
The objective is to evaluate the results of treating keloids in the ears after combining surgical resection with serial triamcinolone infiltration, comparing partial resection techniques with total resection of keloid tissue, in the same patient.
METHOD
This is a prospective pilot study covering reconstructive plastic surgeries for patients with bilateral earlobe keloids, operated by the same plastic surgeon from July 2018 to January 2021 at the Hospital Regional de Sobradinho, in Brasília-DF.
The protocol below was established, based on the work published by Ferreira et al.7, in which the authors partially resected the keloid scar (intralesional), leaving keloid margins in the surgical wound and compared it with the response after total resection (juxtalesional). of another scar in the same patient.
Then it was done:
Triamcinolone (20mg/ml) diluted in 2% lidocaine without vasoconstrictor (1:1), applied 0.5mg/cm of keloid in each ear preoperatively, with a total of 4 applications at intervals of 4 weeks between each session;
Right ear: intralesional/partial excision, maintaining 1mm of skin with keloid on each margin;
Left ear: juxtalesional/total excision of the keloid;
Simple suture with 6-0 nylon;
Triamcinolone (20mg/ml) diluted in 2% lidocaine without vasoconstrictor (1:1), applied 0.5ml to each ear in the immediate postoperative period and maintaining application every 30 days for 6 months;
Photographic record with follow-up for up to 12 months.
18 patients were selected and submitted to strict evaluation and postoperative follow-up criteria. Patients who did not have keloids in the ears bilaterally, who did not agree to participate in the study, or who did not carry out adequate follow-up were excluded, totaling 11 patients at the end of the study. The patients had not undergone previous treatments for keloids until now.
Initially, the following preoperative clinical treatment was carried out: intralesional application of corticosteroid (triamcinolone 20mg/ml – brand Triancil®) diluted in 2% lidocaine without vasoconstrictor (1:1), with 0.5mg/cm of keloid applied to each ear with a 1ml syringe, not exceeding 1 ampoule per session per patient. Four application sessions were carried out, with four-week intervals between each session.
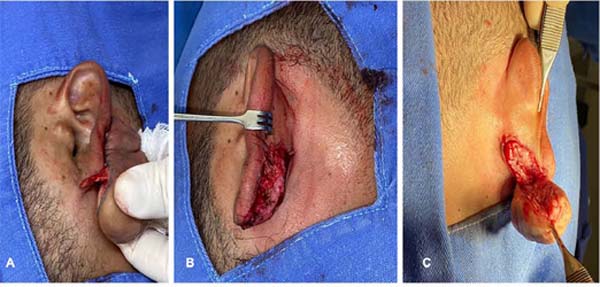
After the 4th month of clinical treatment, surgical treatment was performed according to protocol, with patients under local anesthesia and sedation in a hospital surgical center. In the right ear, intralesional corticosteroid and intralesional excision were performed, leaving a 1mm margin of keloid on each side of the surgical wound. In the left ear, intralesional corticosteroids and surgery with juxtalesional resection were performed, removing the entire keloid and presenting a macroscopically free margin. The wounds were sutured with simple stitches using Nylon 6.0 thread. The stitches were removed on the 14th postoperative day.
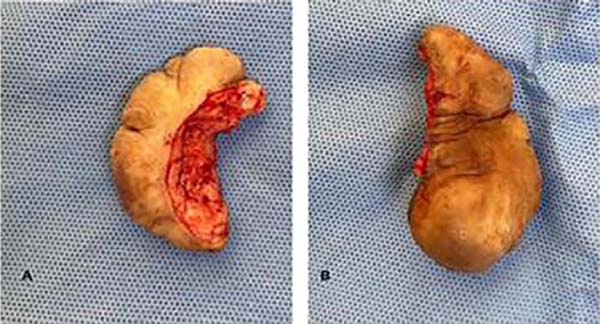
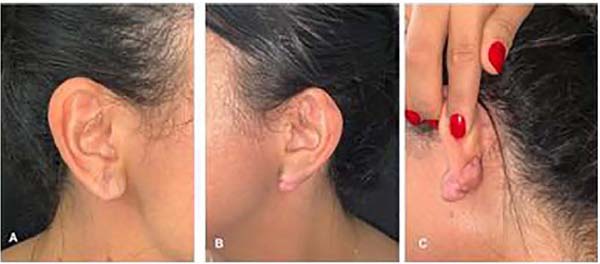
Figures 1, 2, and 3 show pre-, intra- and postoperative images according to the surgical protocol. Scars were evaluated postoperatively over 12 months by the primary surgeon and assistant surgeon. Their appearance was assessed and whether there was a recurrence of keloids in any lesion. In case of recurrence, the patient could be subjected to new treatment according to personal decision.
All excised lesions were sent for pathological study (Figure 4).
This research project followed the legal procedures determined by Resolution 466/12 of the National Health Council concerning research involving human beings and following the principles of the Declaration of Helsinki. Furthermore, it was approved by the Ethics and Research Committee of Hospital Daher Lago Sul and registered on Plataforma Brasil under number CAAE: 68255223.2.0000.0257 and report number 6.114.960(http://aplicacap.saude.gov.br/plataformabrasil).
Statistical analysis
The frequency of categorical data was compared using Fisher’s exact test or the Chi-square test (X2), as appropriate. Categorical variables were expressed as an absolute number, percentage, relative risk (RR), and 95% Confidence Interval (95CI). A value of p<0.05 was considered significant. Statistical analyses were performed using SPSS for Macintosh (Statistical Package for the Social Sciences, Chicago, IL, USA) version 20.0 (Table 1).
RESULTS
Eleven patients and 22 ears were evaluated, 5 male patients and 6 female patients. From the age profile, an average age of 23 years is observed, ranging from 19 to 28 years. All patients underwent ear keloid treatment according to protocol. All anatomopathological results showed that the lesions were keloids (100%), without any malignancy. Any papule or hardened nodule that appeared beyond the earlobe scar line, as seen in Figure 5, was considered a keloid recurrence, without any analysis regarding the dimensions or volume of the lesion. No patient in the study presented an anaphylactic reaction to the dose of triamcinolone applied.
From the evaluation of the scars, 2 patients had a bilateral recurrence of the keloid 6 months after the first surgical excision, corresponding to 18% of cases and 2 female patients had a unilateral recurrence in the left earlobe. The recurrence of the lesion was not related to the previous size of the keloid before treatment. Thus, 4 of 11 patients had some type of recurrence, totaling 36% of recurrence in our study.
It was possible to observe that total excision of the keloid (left ear) had more recurrences than the contralateral side in which a 1mm margin of keloid was left in the scar (right ear), with 36% of recurrences for the left ear versus 18% for the left ear. right (p=0.338), as can be seen in Table 1.
Regarding the level of satisfaction with the postoperative scar, 7 patients reported satisfaction with both scars, 2 patients reported being satisfied with the side on which there was no recurrence (right ear) and dissatisfied with the left ear due to recurrence, and 2 patients were dissatisfied with both sides due to the total recurrence of the keloid.
Regarding the examiner’s assessment, there was no damage to the scar on the right ear in which there was intralesional excision when compared to the left ear whose excision was juxtalesional, presenting flat and satisfactory scars in cases where there was no recurrence of the keloid.
Regarding the evaluation of the scars of patients who presented some type of recurrence (4 patients), it was observed that the keloid scar had reached similar sizes to the previous keloids of the same patients.
DISCUSSION
Changes related to the exacerbation of the scar response, due to factors that are not completely understood, can give rise to keloids, which, unlike hypertrophic scars, go beyond the limits of the wound. The main symptoms are pain, itching, and hyperpigmentation, occurring in 27% of patients3,5. As risk factors we can find: people with black skin or Asian origin, aged between 10 and 30 years, positive family history of keloid scar, blood type A, and presence of HLA B142. The most affected areas are the pre-sternal areas, neck, ear, deltoid, and beard area in men2. More recent studies show that fibroblasts derived from keloids present an exacerbated expression of the p535 gene, reducing apoptosis, and of TGF-BETA and fibroblasts, which produce a greater amount of collagen4.
Isolated surgical resection of the keloid results in therapeutic failure in 40 to 100% of cases, as it stimulates additional collagen synthesis, according to Al-Attar et al.6. Subtotal excision showed lower recurrence rates since the edge of the previous keloid scar immobilizes the lesion and generates less local tension, reducing the traumatic stimulus for collagen synthesis. Furthermore, monofilament threads generate less local inflammatory response6.
Berman & Flores8 observed that the recurrence rate after adequate treatment (surgical excision associated with intralesional corticosteroid injection) is around 20% and the recurrence rate with surgical excision alone fluctuates between 50-80%2.
Ferreira et al.7 carried out a study similar to ours and observed the recurrence of 20% of lesions submitted to intralesional resection versus 45% recurrence of juxtalesional resections. Cosman & Wolff9 concluded that completely removing the keloid does not reduce the chance of recurrence when compared to partial removal.
The literature recommends a minimum of 12 to 24 months of observation. Due to the difficulty of long-term outpatient follow-up, our study recommended evaluating these patients for 12 months. One of the patients who had a recurrence of the keloid underwent a new surgical procedure and is undergoing new monthly sessions of triamcinolone applications. The other patient who had a recurrence is still undergoing preoperative tests for a new approach.
It is important to mention the side effects of the application of corticosteroids, which are: skin atrophy, telangiectasias, depigmentation, infection, necrosis, and ulceration. Systemic effects such as Cushing’s syndrome are rare2,10. According to Ketchum et al.11, to avoid adverse effects, the drug should only be injected at the base of the keloid and not into adjacent normal tissues. No patient in our study presented local or systemic complications related to corticosteroid therapy.
According to Al-Attar et al.6 and Burusapat et al.12, the combined therapy of surgical excision with serial application of triamcinolone is considered one of the treatments with the most satisfactory results and with lower rates of recurrence and complications for keloids.
Finally, there is great difficulty in precisely analyzing the appropriate treatment of keloids, since there is no standardization of therapy in scientific articles, most of which present a small number of patients and a lack of homogenization in the description and evaluation of different scars13. Furthermore, we believe that due to the small sample size (N=11 patients/22 ears), we did not obtain statistical significance when comparing the two techniques. However, it is possible to say that we observed clinical relevance (18 vs. 36%).
CONCLUSION
In the present study, we observed that when associated with treatment with triamcinolone pre-, intra-, and postoperatively, partial excision of the keloid showed lower rates of local recurrence when compared to total excision of the keloid.
REFERENCES
1. Campos H. Cirurgia plástica para estudantes de medicina. 1a ed. Bahia: Sanar; 2020.
2. Urioste SS, Arndt KA, Dover JS. Keloids and hypertrophic scars: review and treatment strategies. Semin Cutan Med Surg. 1999;18(2):159-71.
3. De Felice B, Ciarmiello L F, Mondola P, Damiano S, Seru R, Argenziano C, et al. Differential p63 and p53 expression in human keloid fibroblasts and hypertrophic scar fibroblasts. DNA Cell Biol. 2007;26(8):541-7.
4. Bettinger DA, Yager DR, Diegelmann R F, Cohen IK. The effect of TGF-beta on keloid fibroblast proliferation and collagen synthesis. Plast Reconstr Surg. 1996;98(5):827-33.
5. Griffith BH, Monroe CW, McKinney P. A follow-up study on the treatment of keloids with triamicinolone acetonide. Plast Reconstr Surg. 1970;46(2):145-50.
6. Al-Attar A, Mess S, Thomassen JM, Kauffman CL, Davison S P. Keloid pathogenesis and treatment. Plast Reconstr Surg. 2006;117(1):286-300.
7. erreira FPM, Ferreira EM, Almeida PN, Diniz J V, Lima JCSA, Turrer CL, et al. A interferência do tipo de excisão na recidiva do quelóide: estudo com dois anos de acompanhamento. Rev Bras Cir Plást. 2009;24(3):281-5.
8. Berman B, Flores F. Recurrence rates of excised keloids treated with postoperative triamcinolone acetonide injections or interferon alfa-2b injections. J Am Acad Dermatol. 1997;37(5 Pt 1):755-7.
9. Cosman B, Wolff M. Correlation of keloid recurrence with completeness of local excision. A negative report. Plast Reconstr Surg. 1972;50(2):163-6.
10. Rosen DJ, Patel MK, Freeman K, Weiss PR. A primary protocol for the management of ear keloids: results of excision combined with intraoperative and postoperative steroid injections. Plast Reconstr Surg. 2007;120(5):1395-400.
11. Ketchum LD, Robinson DW, Masters F W. Follow-up on treatment of hypertrophic scars and keloids with triamcinolone. Plast Reconstr Surg. 1971;48(3):256-9.
12. Burusapat C, Wanichjaroen N, Wongprakob N, Sapruangthong R. The Effectiveness of Immediate Triamcinolone Acetonide Injection after Auricular Keloid Surgery: A Prospective Randomized Controlled Trial. Plast Reconstr Surg Glob Open. 2021;9(8):e3729.
13. Carvalhaes SM, Petroianu A, Ferreira MAT, Barros VM, Lopes R V. Assessment of the treatment of earlobe keloids with triamcinolone injections, surgical resection, and local pressure. Rev Col Bras Cir. 2015;42(1):9-13.
1. Hospital Daher Lago Sul, Plastic Surgery -
Brasília - Distrito Federal - Brazil
2. Hospital Universitário de Brasília, General
Surgery - Brasília - Distrito Federal - Brazil
3. Hospital de Base do Distrito Federal,
Anestesiology Department - Brasília - Distrito Federal - Brazil
Corresponding author: Marcela Santos Vilela SHIS QI 25 Conjunto 11 Casa 10, Lago Sul, Brasília, D F, Brazil. CEP: 71660-310 E-mail: marcelasvilela@gmail.com
Article received: September 09, 2023.
Article accepted: April 30, 2024.
Conflicts of interest: none.










 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter