INTRODUCTION
This article aims to report the case of a patient affected by Mondor syndrome in
the postoperative period of breast augmentation. Mondor syndrome is a rare,
benign, and self-limited condition in which thrombophlebitis occurs in the
peripheral venous vessels of the breast, which can even affect the lymphatic
system in the region, presenting clinically as a subcutaneous fibrous cord on
the anterolateral wall of the chest1.
Thus, the importance of the study is urgent amid the exponential increase in
aesthetic surgical interventions in the world, which, in 2019, reached
11,363,569 procedures, a number 7.4% higher than in 2018, according to the
International Society of Aesthetic Plastic Surgery ( ISAPS)2. Still according to
ISAPS, Brazil, in 2019, was responsible for 13.1% of procedures, totaling almost
1,500,000 interventions2.
Added to this, the relevant association of Mondor syndrome with breast carcinoma
requires concern for the disease3.
Furthermore, it is essential to properly guide patients affected by this
clinical condition, to calm them down, and to treat them appropriately.
CASE REPORT
MCGM, female patient, 22 years old, mixed race, medical student, born in Sousa-PB
and from Natal-RN, underwent breast augmentation on 12/05/2020, having
progressed uneventfully in the immediate postoperative period.
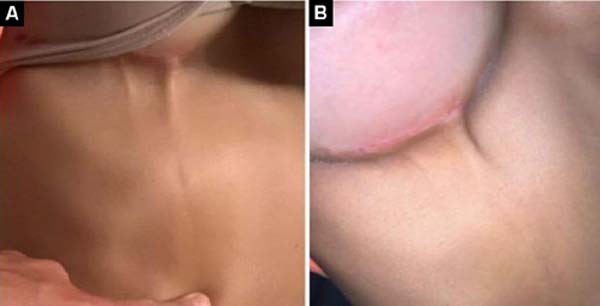
On the 23rd post-operative day, she began to complain of progressive pain
(intensity 5/10) without irradiation in the lower region of the right breast,
with the appearance of a thin subcutaneous cord of hardened consistency and high
temperature, without factor triggering and improving, which was directed to the
upper right quadrant of the abdomen, retracting the skin (Figure 1).
Figure 1 - A-B: Photographs taken by the patient herself at the beginning of
the reported clinical picture that show the fibrous cord typical of
the condition discussed.
Figure 1 - A-B: Photographs taken by the patient herself at the beginning of
the reported clinical picture that show the fibrous cord typical of
the condition discussed.
Physical examination confirmed the presence of a fibrous cord that began in the
inframammary region and extended to the right upper abdominal quadrant. The
plastic surgeon responsible for the aesthetic procedure the patient underwent,
through physical examination alone, confirmed the diagnosis of Mondor
syndrome.
Afterward, the professional instructed the patient to use Prednisone® 20mg orally
once a day, for 7 days, and to apply a warm compress to the area three times a
day. Furthermore, he advised the patient about Mondor syndrome, which therefore
recognized the self-limited nature of the condition, a situation that reduced
the patient’s nervousness and concerns about the syndrome.
There was progressive remission of the fibrous cord projected under the skin,
which completely disappeared after 10 weeks, without leaving any scars.
The patient was taking contraceptive therapy without medical advice. In the
period of 8 months before the surgery, she was using Iumi®, a combined oral
contraceptive.
DISCUSSION
Mondor syndrome is almost ten times more common in women than in men and
primarily affects the average age group of 43 years. Presenting greater
unilateral involvement, with few reports of bilateral appearance, Mondor
syndrome is evident without systemic signs4.
This condition is associated, in up to 12% of cases, with the emergence of breast
carcinoma, a situation that explains the concern surrounding its diagnosis3 and makes the need to investigate the
disease causing the pathology under discussion imminent.
The etiology related to the development of Mondor syndrome has not yet been
completely clarified, with 50 to 60% of cases considered idiopathic5. However, its pathophysiology is similar
to deep vein thrombosis (DVT)6 and its genesis is also related to Virchow’s
triad (stasis, hypercoagulability, and endothelial damage)7. It is believed that the deficient action of venous
valves, by enabling retrograde blood flow, generates stasis that favors the
formation of thrombi, which can progress with aggression to the vascular wall
and the formation of venous fibrosis typical of the syndrome under
discussion8.
The use of oral contraceptives increases the risk of DVT as the dosage of
estrogen increases. Estrogen tends to increase levels of clotting factors,
reduce levels of antithrombin III, and decrease plasminogen activator9. Some risk factors are associated with the
development of the disease, such as surgical procedures, breast cancer, trauma,
injectable drug abuse, pendulous breasts, excessive physical activity,
pregnancy, blood dyscrasia, infections, and rheumatoid arthritis9.
The characteristic lesion of Mondor syndrome begins with the appearance of a
rounded, painful, reddish cord, which progresses to a thick, painless fibrous
line10, whose structure becomes more
evident with the abduction movement of the arm. The appearance of the fibrous
cord is limited, preferably, to the inframammary region, with its appearance
until the fourth week after surgery and total remission until the eighth
week4.
A priori, the clinical condition of patients with Mondor syndrome is
characterized by pain, increased breast volume, and retraction of the skin at
the level of the lesion, which can be identified as a fibrous cord or palpable
mass on physical examination. Furthermore, the patient may be asymptomatic or
even have less common symptoms, such as fever, bruising, and skin
inflammation5.
A mammogram is an exam that can be requested, observing a tubular, dilated, long,
and superficial density, giving a “rosary bead” appearance, thus suggesting
thrombosis of the affected vein4. The
importance of this examination is mainly due to the possibility of diagnosing
non-palpable breast neoplasia.
Treatment for Mondor syndrome is symptomatic only. Generally, a warm compress is
used at the site of thrombophlebitis and rest and the use of analgesics and
non-steroidal anti-inflammatory drugs are recommended. For the doctor and
examiner, it is essential to inform the patient about the benign and
self-limited nature of the condition, accepting their concerns.
CONCLUSION
In light of these considerations, it is concluded that Mondor syndrome is a rare
condition and its main characteristic is the presence of a fibrous cord caused
by the formation of a thrombus, with the breast being the most affected region
of the human body - emerging as a complication breast surgery, but it can also
affect males to a lesser extent, preferably affecting regions of the penis and
scrotum.
Finally, it is worth highlighting that it is a benign and self-limited condition
(with a beginning, middle, and end), but that, due to its relationship with
breast carcinoma, it requires attention for its diagnosis.
REFERENCES
1. Faucz RA, Hidalgo RT, Faucz RS. Doença de Mondor: achados
mamográficos e ultra-sonográficos. Radiol Bras.
2005;38(2):153-5.
2. International Society of Aesthetic Plastic Surgery (ISAPS).
International Survey of Aesthetic/Cosmetic Procedures 2019. Mount Royal: ISAPS;
2019.
3. Catania S, Zurrida S, Veronesi P Galimberti V, Bono A, Pluchinotta
A. Mondor’s disease and breast cancer. Cancer.
1992;69(9):2267-70.
4. Becker L, McCurdy LI, Taves DH. Superficial thrombophlebitis of the
breast (Mondor’s disease). Can Assoc Radiol J.
2001;52(3):193-5.
5. Pasta V D’Orazi V Sottile D, Del Vecchio L, Panunzi A, Urciuoli P.
Breast Mondor’s disease: Diagnosis and management of six new cases of this
underestimated pathology. Phlebology. 2015;30(8):564-8.
6. Sobreira ML, Yoshida WB, Lastória S. Tromboflebite superficial:
epidemiologia, fisiopatologia, diagnóstico e tratamento. J Vasc Bras.
2008;7(2):131-43.
7. Alvarez-Garrido H, Garrido-Ríos AA, Sanz-Muñoz C, Miranda-Romero A.
Mondor’s disease. Clin Exp Dermatol. 2009;34(7):753-6.
8. Khan UD. Incidence of mondor disease in breast augmentation: a
retrospective study of 2052 breasts using inframammary incision. Plast Reconstr
Surg. 2008;122(2):88e-89e.
9. Favarin GJ, Favarin E, Rocha LPS, Horner C. Mondor’s disease, case
report and literature review. Arq Catarin Med.
2016;45(2):102-6.
10. Piccinato CE. Trombose venosa pós-operatória. Medicina (Ribeirão
Preto). 2008;41(4):477-86.
1. Universidade Federal do Rio Grande do Norte, Natal, RN, Brazil
2. Universidade de Brasília, Brasília, DF, Brazil
3. Secretaria de Estado da Saúde Pública, Centro Estadual de Reabilitação e Atenção Ambulatorial Especializada, Natal, RN, Brazil
Corresponding author: Rafael Rodolfo Tomaz de
Lima Av. Alexandrino de Alencar, 1900, Tirol, Natal, RN, Brazil. Zip Code: 59030-660, E-mail: limarrt@gmail.com
Article received: September 18, 2023.
Article accepted: April 30, 2024.
Conflicts of interest: none.
Institution: Universidade Federal do Rio Grande do Norte, Natal, RN, Brazil.