

Review Article - Year 2024 - Volume 39 -
Impact of upper blepharoplasty on quality of life and its insertion in the context of Brazilian public health: scoping review
Impacto da blefaroplastia superior na qualidade de vida e sua inserção no contexto da saúde pública brasileira: revisão de escopo
ABSTRACT
Introduction: The aim was to conduct a comprehensive scoping review of available researches on the impact of blepharoplasty on quality of life and its scope within the Unified Health System.
Methods: A literature search was performed in the Virtual Health Library, Capes Journals, SciELO, LILACS, Medline, and Cochrane Library databases for studies published within the past five years.
Results: Out of the 323 studies initially selected, nineteen studies were included in the final sample. Seven studies (36.8%) examined the impact of blepharoplasty on quality of life, while others assessed functional criteria (31.5%) or subjective factors related to quality of life (26.3%). The majority of the studies demonstrated positive effects of blepharoplasty on quality of life, self-esteem, personal satisfaction, well-being, and visual improvement. However, limited data were found regarding the coverage of blepharoplasty in the public healthcare system, with no specific studies on this topic.
Conclusion: Blepharoplasty has been shown to positively impact quality of life, highlighting the need to ensure the access to this procedure within the public healthcare when appropriate. The lack of data on blepharoplasty within the Unified Health System indicates a research gap and emphasizes the importance of further studies to explore its impact on quality of life, as well as its coverage and expansion.
Keywords: Blepharoplasty; Quality of life; Unified Health System; Personal satisfaction; Aging
RESUMO
Introdução: O objetivo foi desenvolver uma revisão de escopo que mapeie pesquisas disponíveis que respondam à questão: "O que se sabe sobre o impacto da blefaroplastia na qualidade de vida? Qual sua abrangência no Sistema Único de Saúde?".
Método: Levantamento bibliográfico nas bases de dados: Biblioteca Virtual em Saúde, Periódicos Capes, SciELO, LILACS, Medline e Cochrane Library, com estudos publicados nos últimos cinco anos.
Resultados: Foram selecionados 323 estudos para pré-análise e a amostra final contou com 19 estudos. A qualidade de vida foi analisada em sete dos estudos incluídos (36,8%) e os demais analisaram critérios funcionais (31,5%) ou outras questões subjetivas que podem estar ligadas à qualidade de vida (26,3%). A maioria dos estudos demonstrou que a blefaroplastia traz melhora na qualidade de vida e em critérios indiretos como autoestima, satisfação pessoal e bem-estar, além de melhora da visão. Os dados sobre a cobertura da cirurgia no contexto público são escassos e não foi encontrado nenhum estudo que tratasse desse tema.
Conclusão: A blefaroplastia impacta positivamente na qualidade de vida, reforçando a necessidade de se fazer cumprir o direito de realização do procedimento na saúde pública, quando comprovada sua indicação. A ausência de dados sobre a blefaroplastia no Sistema Único de Saúde demonstra alguma negligência deste tópico no âmbito da saúde pública. Portanto, a presente pesquisa tem importância em evidenciar tal lacuna, incentivando a realização de estudos que aprofundem a análise do impacto da blefaroplastia na qualidade de vida, bem como, busquem entender melhor sua cobertura e formas de ampliá-la.
Palavras-chave: Blefaroplastia; Qualidade de vida; Sistema Único de Saúde; Satisfação pessoal; Envelhecimento
INTRODUCTION
Aging is a biological process that results in several anatomical and functional changes in the human body. In this context, the eye region is essential to guarantee facial harmony, in addition to being an important means of social communication, constituting the most important aesthetic-functional component of the face, and any changes in this region can lead to compromised such functions1.
In this sense, one of the most frequent clinical manifestations derived from the natural aging process is eyelid ptosis2, which mainly affects the upper eyelid and may have other etiologies in addition to aging, such as neurogenic, myogenic, traumatic, or even congenital factors3. As a consequence, eyelid ptosis brings to the patient a reduction in campimetry and visual quality, an increase in the incidence of entropion (a condition that facilitates contact between the eyelashes and the ocular conjunctiva, predisposing to infections), and a decline in self-esteem, contributing significantly to the reduction of the quality of life1.
In this context, blepharoplasty arises, a surgical procedure that aims to correct any functional or aesthetic abnormality existing in the eyelids, mostly performed by plastic surgeons and ophthalmologists1. Due to its notorious importance, the Unified Health System (Sistema Único de Salud SUS) guarantees citizens the right to undergo reconstructive plastic surgery, especially when there is partial or total functional impairment and there are no treatment alternatives other than surgery. In this way, patients are guaranteed blepharoplasty surgery through the SUS when the functional declines described above are proven4.
From this perspective, this scoping review was carried out, to elucidate and substantiate what the coverage of care for patients in need of blepharoplasty in the SUS really is, as well as the scope of its impact on patients’ quality of life.
OBJECTIVE
Therefore, the main objective of this scoping review was to systematically map the available research on the proposed topic, in addition to delimiting the remaining gaps in the study of the area. To this end, the following research questions were formulated: What is known about the impact of upper blepharoplasty on quality of life? What is its scope in the single health system?
METHOD
This study is a scoping review guided by the references and principles proposed by the Joanna Briggs Institute (JBI) and Preferred Reporting Items for Systematic Review and MetaAnalyses extension for Scoping Review (PRISMA- ScR)5,6, aiming to search for information available, as well as the identification of remaining gaps in the subject covered by following the steps: formulation of objectives and research questions (“What is known in the literature about the impact of blepharoplasty on quality of life and its scope in the SUS? ”; structuring the research question using the acronym PCC - Population: individuals undergoing blepharoplasty / Concept: quality of life / Context: blepharoplasty surgery, SUS); elaboration of exclusion and inclusion criteria; development of the search strategy; search and selection of studies; data mapping and synthesis of results.
Eligibility Criteria
To select the studies, the following criteria were used: studies published from 2017 to 2022, that addressed quality of life, functionality, and patient satisfaction after upper blepharoplasty, performed as the first intervention, in English, Portuguese, and Spanish, with the application of the filter “in the last 5 years”. Quantitative, qualitative, and mixed studies were included, aiming for a broad understanding of the topic.
Information sources
The bibliographic survey took place from March to June 2022, based on searches in the electronic databases Medline, VHL, Periódicos Capes, SciELO, and LILACS. In addition to searching journals, data were collected from the official websites of the Ministry of Health and the Sociedade Brasileira de Cirurgia Plástica.
The results obtained were exported to EndNote to exclude repeated articles. The search strategy used was through the descriptors present in MeSH (Medical Subject Headings) and DeCS (Health Sciences Descriptors): “Blepharoplasty”, “Quality of Life”, “Visual Field Tests”, “Patient Satisfaction” and “ Health Unic System”.
These descriptors were combined using the Boolean operators OR and AND, which were used in the databases as expressed in Chart 1.
| Databases/ Libraries/ Search Engines/ Grey Literature | Search Strategies |
|---|---|
| PubMed, VHL, Journals Capes, LILACS, SciELO, Cochrane. | ((“Blepharoplasty” OR “Eyelid surgery”)) AND ((Quality of
life)) ((“Blepharoplasty” OR “Eyelid surgery”)) AND ((Visual field test)) ((“Blepharoplasty” OR “Eyelid surgery”)) AND ((Patient satisfaction OR satisfaction)) ((“Blepharoplasty” OR “Eyelid surgery”)) AND ((Patient satisfaction)) AND ((Quality of life)) AND ((Visual field test)) |
To increase the consistency of the research, all articles found in the databases described were selected together by the researchers, following the order of title, abstracts, and, finally, full text, so that, in the end, through discussion between the evaluators, only those studies that contributed to answering the research questions were classified by consensus.
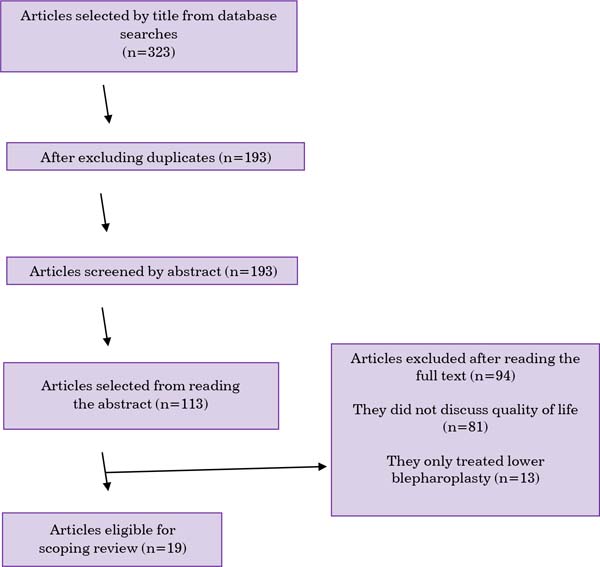
The first search, selecting articles based on the title, totaled 323 articles chosen. After duplicates were removed (130), 193 citations remained. After this stage, the summary of the articles in question was read, leaving 113 studies. Finally, after reading the full text, and taking into account the eligibility criteria, we had 19 articles eligible for this scoping review. Of the 94 excluded studies, 81 did not discuss or speak very superficially about the impact of blepharoplasty on patients’ quality of life and 13 dealt only with lower blepharoplasty. Data is expressed in Figure 1.
RESULTS
The title, author, year, journal, objectives, study design, methods, and results of the studies concerning the research questions are presented in Chart 2.
| Title | Authors, Year, and Journal | Objectives | Design | Number of participants and age | Methods | Result |
|---|---|---|---|---|---|---|
| The Effect of Blepharoplasty on Our Patient’s Quality of Life, Emotional Stability, and Self-Esteem7 | Papadoulos et
al., 2019 The Journal of Craniofacial Surgery |
Determine whether blepharoplasty affects the quality of life, satisfaction, emotional stability, and self-esteem | Retrospective study with patients who underwent transdermal blepharoplasty between 1995 and 2008 | 46 patients (age 38-75 years) | Application of a self-developed questionnaire for blepharoplasty, in addition to the Statistically significant increased values in quality of life (FLZM), Freiburg Personality Inventory (FPI-RL), and Rosenberg Self-Esteem (RSES). | Improved quality of life in the aspects: of work, mobility, and independence. Increased self-esteem |
| Association on of Upper Eyelid Ptosis Repair and
Blepharoplasty With Headache-Related Quality of Life8 |
Bahceci Simsek, 2017 JAMA Facial Plast Surgery |
To evaluate changes in headache-related quality of life in patients undergoing upper blepharoplasty | Prospective cohort study | 108 patients undergoing blepharoplasty and 44 patients undergoing ptosis correction (age 45-49 years) | Application of the Headache Impact Test-6 (HIT) questionnaire preand postoperatively for patients with tension headache. | Increase in Headache Impact Test-6 (HIT) score in the two groups studied (ptosis repair and upper blepharoplasty) |
| Upper eyelid blepharoplasty using Plasma exeresis: Evaluation of outcomes, satisfaction and symptoms after procedure9 | Ferreira et
al., 2021 Journal of Cosmetic Dermatology |
To evaluate patient satisfaction and symptoms after upper blepharoplasty using plasma technology | Observational study of patients who underwent upper blepharoplasty using plasma to treat dermatitis | 16 patients (average age 50.5 years) | Assessment of quality of life, symptoms, and satisfaction using two questionnaires on day 7 and 30 after the procedure | High level of satisfaction, but low impact on daily quality of life |
| Functional benefits and patient satisfaction with upper blepharoplasty - evaluated by objective and subjective outcome measures10 | Jacobsen et al., 2017 Acta Ophthalmology |
Investigate functional outcomes and patient satisfaction in upper blepharoplasty | Observational cohort study | 45 patients (mean age 56.9 years) | Preand postoperative analysis of the patient's visual capacity, together with a questionnaire to assess the functional and psychosocial impact of the eyelid | Increase in the superior visual field by 31.3% on the right side and 28.3% on the left side. All patients were satisfied with the postoperative result and would undergo surgery again. |
| Title | Authors, Year, and Journal | Objectives | Design | Number of participants and age | Methods | Result |
| Measuring satisfaction with appearance: Validation of the FACE-Q scales (ferramenta de resultados relatados pelo paciente (PRO) composta por várias escalas e listas de verificação com funcionamento independente, projetadas para medir os resultados) for double-eyelid blepharoplasty with minor incision in young Asiansretrospective study of 200 cases11 | Chen et al.,
2017 Journal of Plastic, Reconstructive & Aestethic Surgery |
Use a validated FACE-Q questionnaire (a patient-reported outcomes (PRO) tool comprised of multiple independently functioning scales and checklists designed to measure outcomes) to assess patient-reported satisfaction after small-incision double blepharoplasty | Retrospective study with patients who underwent double blepharoplasty between 2012 and 2014 | 200 patients (age 21-30 years) | Administration of the FACE-Q questionnaire (a patient-reported outcomes (PRO) tool comprised of several independently functioning scales and checklists designed to measure outcomes) anonymously via email | High level of satisfaction with overall eye appearance and increased quality of life, including confidence and well-being |
| Functional outcomes of upper eyelid blepharoplasty: A systematic review12 | Hollander et al., 2019 Journal of Plastic, Reconstructive & Aestethic Surgery |
Review the literature to evaluate the objective and subjective functional benefits of upper blepharoplasty | Revisão sistemática | 3525 estudos | Busca sistemática em 4 bases de dados (Pubmed, Embase, Cinahl e Cochrane) | 28 estudos foram incluídos e mostraram aumento do campo de visão, aumento da qualidade de vida por diminuição da cefaleia e melhora da visão e diminuição da sensibilidade das pálpebras. Resultados para altura da sobrancelha, astigmatismo, sensibilidade ao contraste e cinemática da pálpebra não foram consistentes. |
| Title | Authors, Year, and Journal | Objectives | Design | Number of participants and age | Methods | Result |
| Investigation of Goldmann perimetry in evaluation of patients for upper eyelid blepharoplasty13 | Pemberton et
al., 2018 Orbit |
To determine whether the preoperative Goldman Visual Test (GVT) tested in patients with functional dermatochalasis describes the postoperative superior visual field outcome | Prospective cohort study | 23 patients (mean age 67 years) | Obtaining the Goldman Visual Test (GVT) pre-operatively with the eyelids in the natural position and post-operatively and subsequent analysis to determine whether the pre-operative test accurately predicts visual field improvement | Preoperative testing underestimated postoperative outcome by an average of 35%, therefore, postoperative improvement in the visual field is typically greater after blepharoplasty than the Goldman Visual Test (GVT) predicts. |
| Objective quantification of the impact of blepharoplasty on the superior visual field14 | Kim et al., 2022 Archives of Plastic Surgery |
To analyze the visual field before and after surgery and investigate whether visual field measurements can be applied as an adequate predictor of surgical results | Prospective study | 9 patients (mean age 59.66 years) | Nine patients with pseudoptosis who underwent
blepharoplasty participated. Visual fields were analyzed
preoperatively and 3 months postoperatively with the
Goldmann kinetic perimetry test |
Blepharoplasty had an average beneficial effect of 4.99 times on the superior field of vision. There was a strong correlation between the preoperative superior visual field and the surgical outcome. |
| Assessment of Patient Satisfaction With Appearance, Psychological Well-being, and Aging Appraisal After Upper Blepharoplasty: A Multicenter Prospective Cohort Study15 | Domela
Nieuwenhuis et al., 2022 Aesthetic Surgery Journal |
To evaluate patient-reported satisfaction with facial appearance, psychological well-being, and assessment of aging after upper blepharoplasty with validated questionnaires | Prospective cohort study | 2134 elderly patients | Upper blepharoplasty patients from 8 outpatient clinics were included. Patient-reported satisfaction was assessed with the FACE-Q at admission and 6 and 12 months postoperatively. | Large improvements in FACE-Q scores between admission and 6 months postoperatively were observed for satisfaction with appearance, psychological well-being, and assessment of aging. Satisfaction with treatment results was strongly correlated with satisfaction with appearance, but not with assessment of aging. |
| Title | Authors, Year, and Journal | Objectives | Design | Number of participants and age | Methods | Result |
| Patient-reported outcome measurement in upper blepharoplasty: How to measure what the patient sees 16 | Herruer et al., 2018 Journal of Plastic, Reconstructive & Aestethic Surgery |
Research the outcome of blepharoplasty in terms of satisfaction and quality of life, as well as determine a recommendation on which assessment tools should be used | Prospective study | 56 patients (36 completed all questionnaires, (mean age 55 years) | Patients undergoing blepharoplasty completed Blepharoplasty outcome evaluation (BOE) and Derriford appearance scale 59 (DAS59) questionnaires preoperatively and 3-6 months postoperatively. Visual analog scales (VAS) were also used preand postoperatively and the Glasgow Benefits Inventory (GBI) was used postoperatively. | Both satisfaction with the eyes and self-esteem improved significantly. Patients reported significant benefits after the procedure. |
| Effects of Upper Eyelid Blepharoplasty on Contrast Sensitivity in Dermatochalasis Patients1 7 | Nalci et al., 2020 Turkish Journal of Ophthalmology |
To evaluate the impact of upper eyelid blepharoplasty on contrast sensitivity in patients with dermatochalasis | Prospective study | 34 patients (mean age 59.66 years) | Preoperatively and postoperatively, best-corrected visual acuity, ophthalmological examination, eyelid examination, eyelash ptosis, contrast sensitivity, keratometric parameters, and corneal aberrations were evaluated in 34 eyes of patients undergoing upper blepharoplasty for dermatochalasis among the years 2014 and 2018 | Contrast sensitivity increases significantly after upper blepharoplasty, especially at higher spatial frequencies. Blepharoplasty may have additional functional indications for elderly patients with dermatochalasis in terms of improving functions such as performing daily tasks and reading. |
| Title | Authors, Year, and Journal | Objectives | Design | Number of participants and age | Methods | Result |
| A practical technique combining orbicularis oculi muscle resection-based epicanthoplasty and orbicularis-tarsus fixation double-eyelid plasty for cosmetic blepharoplasty18 | Sun et al., 2019 Journal of Plastic, Reconstructive & Aestethic Surgery |
To describe a technique that combines epicanthoplasty based on resection of the orbicularis oculi muscle and double eyelid plasty with orbicularis tarsus fixation for cosmetic blepharoplasty and report the surgical results in a large number of Chinese patients. | Prospective study | 475 patients with an average age of 26 years | From January 2015 to February 2019, 475 patients underwent double eyelid blepharoplasty associated with epicanthoplasty using this technique. The follow-up period ranged from 2 to 38 months, with an average of 16 months | 97% of patients were satisfied with the surgical results, presenting well-defined eyelid folds and a naturally improved contour of the inner corner, with no evident scar. Photographic analysis showed a significant improvement in the proportion of the palpebral fissure postoperatively. |
| Surgical outcome and patient satisfaction after Z-epicanthoplasty and blepharoplasty19 | Zhao et al.,
2019 International Journal of Ophthalmology |
To evaluate the surgical outcomes of the modified Z-epicanthoplasty with blepharoplasty that we previously reported from the patient's perspective using patient-reported outcome measures (PROMs) and patient satisfaction scores. | Retrospective study | 180 patients (average age 24 years) | 180 patients who underwent surgery between January 2013 and June 2016 were randomly selected. Standardized patient satisfaction forms and questionnaires using validated patient-reported outcome measures (PROMs) were sent to patients for completion. | Most patients reported good or excellent results on analysis of patient-reported outcome measures (PROMs). In questions relating to function and appearance, 80.3% reported satisfaction with both domains. Most patients reported a high or very high satisfaction rate producing an average score of 104 out of 120 for the patient satisfaction assessment |
| Title | Authors, Year, and Journal | Objectives | Design | Number of participants and age | Methods | Result |
| Factors Influencing Patient Satisfaction with Upper Blepharoplasty in Elderly Patients20 | Kim et al., 2021 Plastic and Reconstructive Surgery-Global Open |
Research which factors influence elderly patient satisfaction in upper blepharoplasty | Prospective study | 57 patients (over 65 years of age) | Patients undergoing upper blepharoplasty between April 2018 and March 2019 responded to a pre-operative questionnaire and after 6 months, a satisfaction survey was carried out. | Significant verification of regression coefficients showed that functional improvement and cognitive degree of postoperative precautions had a significant effect on patient satisfaction, while aesthetic results and surgical outcome expectations were not correlated with patient satisfaction. |
| Qualidade de vida e autoestima em idosas submetidas e não submetidas à cirurgia estética21 | Spadoni-Pacheco e Carvalho, 2018 Revista Brasileira de Cirurgia Plástica |
To evaluate the importance of aesthetic surgery (CE) for the elderly, and whether there is a difference in quality of life and self-esteem between elderly women who have and have not undergone cosmetic surgery. | Case-control study | 25 elderly women who underwent cosmetic surgery (EC) and 25 elderly women who did not undergo CE (average age of 67.26 years). | Case group formed by 25 elderly women who underwent aesthetic surgery (CE) and the control group of 25 elderly women who did not undergo aesthetic surgery (CE). The instruments applied were: Minimental, quality of life questionnaire (WHOQOL-BREF), Rosenberg self-esteem scale, and a questionnaire designed to research sociodemographic data, motivation, and satisfaction with aesthetic surgery (CE). | The most chosen reasons for surgery were physical discomfort, the desire to improve quality of life (QoL), and dissatisfaction with self-image. No elderly women were found with low self-esteem and the level of satisfaction was high when related to their own life or social life. There was no difference in quality of life (QOL) and self-esteem between the two groups analyzed. |
| Title | Authors, Year, and Journal | Objectives | Design | Number of participants and age | Methods | Result |
| Assessment of self-esteem and psychological aspects in patients undergoing upper blepharoplasty22 | Gracitelli et al., 2017 Revista Brasileira de Oftalmologia |
To evaluate the results of self-esteem and quality of life in patients undergoing upper blepharoplasty. | Cross-sectional study | 49 individuals diagnosed with dermatochalasis. | The self-esteem and quality of life of patients undergoing upper blepharoplasty were compared with volunteers of the same age. Preoperative assessment included ophthalmological examinations and two questionnaires: the Rosenberg Self-esteem Scale (RSES) and the World Health Organization quality of life assessment (WHOQOL-BREF). | Individuals undergoing upper blepharoplasty had
worse self-esteem based on the Rosenberg Self-Esteem Scale
(RSES). Regarding the quality of life, assessed by the World Health Organization the quality of life assessment (WHOQOL-BREF), significant differences were evident between the groups in the psychological aspects subscale. |
| The Bleph and the Brain: The Effect of Upper Eyelid Surgery on Chronic Headaches2 3 | Mokhtarzadeh
et al., 2017 Ophthalmic Plastic & Reconstructive Surgery |
Determine the effect of upper eyelid surgery on headache symptoms | Case-control study | 47 patients (age 58.7 to 60.7 years) | Case and
control groups completed a preand post-operative Headache Impact
Test-6 quality of life questionnaire. The study was carried out
over a period of 2 years. Neither patients nor study investigators were masked. |
Postoperative scores were better in the case group compared to the control group. All questions on the Headache Impact Test-6 improved significantly in the case arm compared to the control. Subjectively, 25 of 28 study patients and 4 of 19 control patients noted some improvement in symptoms after surgery. |
| Title | Authors, Year, and Journal | Objectives | Design | Number of participants and age | Methods | Result |
| Resultados funcionales de la blefaroplastia superior2 | Hernández Sánchez et al., 2021 Revista Cubana de Oftalmologia |
Describe the functional results of upper blepharoplasty | Prospective longitudinal study | 99 patients (age 50-62 years) | A prospective longitudinal descriptive study was carried out on patients diagnosed with upper eyelid dermatochalasis, some associated with eyelid and eyebrow ptosis from February 2019 to January 2020. | In 98% of the intervention cases, total
correction of dermatochalasis of the upper eyelid was achieved,
ptosis correction in 86%, and eyebrow correction in
88%. There were no complications in 94% of the operated eyelids. The most frequent complication was bleeding, with 2.5%. |
| Influence of upper blepharoplasty on intraocular lens calculation2 4 | Vola et al., 2021 Arquivo Brasileiro de Oftalmologia |
Determine the effect of upper blepharoplasty on corneal topography and intraocular lens power calculation using Galilei and IOLMaster (Holladay formula). | Case series study | 30 patients (age 47.7 - 74.4 years). | Patients undergoing upper blepharoplasty underwent imaging sessions with Galilei and IOLMaster (Holladay's formula) preoperatively and at 1 and 6 months postoperatively. Axial length determination and lens power calculation were performed using only IOLMaster (Holladay formula). Paired t-tests and vector analysis were used for statistical analysis. | Vector analysis showed that 6 months after surgery, blepharoplasty induced on average 0.39D and 0.31D of corneal astigmatism, measured with Galilei and IOLMaster (Holladay's formula). IOLMaster measurements (Holladay's formula) showed that mean corneal curvature, steepest corneal curvature, and corneal astigmatism were greatest 6 months after surgery. They also showed that intraocular lens power was significantly lower 6 months after surgery. |
Of the selected studies, only seven of them7-10,12,21,22 cited or directly evaluated the criterion of improvement in quality of life; of these, five7,8,11,12,22 found a statistically significant increase in quality of life after blepharoplasty, one found no significant differences21 and another found a low impact on quality of life on the seventh day after surgery9. The age of individuals participating in these studies varied, with one article without specification12, four (57%) with patients at least 50 years old9,10,21,22, one between 45 and 49 years old8 and another covering patients from 38 to 75 years old.
Six studies analyzed the functional results of upper blepharoplasty2,10,13,14,17,24, a criterion that was considered by the present review as a possible contributing factor to the improvement in quality of life. Of these studies, three found a significant increase in the superior field of vision10,13,14, one showed a significant increase in contrast sensitivity17 after surgery and, together with another study24, demonstrated excellent levels of correction of dermatochalasis. Furthermore, induction of corneal astigmatism and decreased power of the intraocular lens were also found after blepharoplasty25. Most research was carried out on patients over 55 years old10,13,14,17,25 and only one had an age ranging between 47.7 and 74.4 years24. In all studies, the majority of patients were female.
Finally, six studies11,15,16,18,20,23 evaluated subjective issues that may be linked to improved quality of life, such as patient satisfaction15,16,18,20, headache improvement23, psychological well-being15 and self-esteem16. They all found significant improvements in the respective criteria analyzed, through the application of questionnaires to participating patients.
From the results demonstrated here, it was clear that, with a few exceptions9,21,24, blepharoplasty has a positive and significant impact on the lives of patients undergoing surgery, whether due to functional or well-being criteria. Benefits include high satisfaction, improved self-esteem, increased field of vision, safety, and well-being.
Considering all the benefits, blepharoplasty surgery is provided by the SUS and is included in the Table of Procedures, Medications, Orthoses and Prostheses, and Special Materials of the Unified Health System (SIGTAP)25. The amount spent by the SUS to carry out this procedure was changed by ordinance no. 3,03726, of November 14, 2017, to 449.44 reais. Blepharoplasty may be recommended by a general practitioner or ophthalmologist in the following conditions: (1) dermatochalasis (excess skin and sagging in the upper eyelid fold) with obstruction of the visual axis, (2) lagophthalmos (palpebral malocclusion), (3) alteration the position of the eyelids, (4) post-trauma eyelid deformities or burn sequelae4.
However, the procedure is only covered by the SUS in hospitals where there is a Plastic Surgery residency27. According to data from the Sociedade Brasileira de Cirurgia Plástica (SBCP), in Brazil, there are 88 accredited medical residency services, several of which are located in the same city and 13 (50%) of the 26 Brazilian states are not covered by any accredited service. , demonstrating the scarcity and difficulty in accessing this resource for the population.
No data was found on the SUS waiting list, as well as the number of blepharoplasties performed per year, making it impossible to conclude the reality of the expected coverage. The only data found on the coverage of plastic surgeries by the SUS was provided by the SBCP Census of 201628, which demonstrated that, of the total number of plastic surgeries performed that year, 16.30% were performed by the SUS, however, there is no specification of how much this percentage represents the blepharoplasty itself.
On the other hand, some actions, mainly by the SBCP, sought to make up for the deficit in the care of these patients on the waiting list, in the form of blepharoplasty joint efforts carried out in some Brazilian cities29. These actions, for the most part, take place in partnership with SUS hospitals and bring together medical teams that mobilize in a short period to serve as many patients as possible. Despite the lack of data on the number of surgeries performed by the SUS, the need to organize actions like these already denotes the existence of a gap in necessary care in the area.
Furthermore, in the databases searched, no study was found on the inclusion of blepharoplasty in the SUS, only on other reconstructive plastic surgeries, such as skin and breast tumors.
This scoping review has some limitations. The main one was the lack of publications dealing with the topic, in addition to extremely scarce and limited data regarding the coverage of blepharoplasty by the SUS, mainly in the scientific literature, with no scientific study on this being found. Therefore, it was not possible to have clarity on the Brazilian scenario in terms of the real demand of the population, the waiting list, and the surgery itself. Another limitation of this review is that no randomized clinical trial was found regarding the effects of blepharoplasty on any of the outcomes mentioned. All primary studies included in this review were observational, being cohorts, case-control, and case series. Therefore, there is a great need to develop well-conducted randomized clinical trials that evaluate the effectiveness of upper blepharoplasty on relevant patient outcomes.
CONCLUSION
In the selected studies that sought to understand the influence of blepharoplasty on patients’ quality of life, different ways of clarifying this relationship were found. The first was direct, with a specific focus on analyzing improvements in quality of life, through pre-defined criteria. The second was indirectly, researching criteria that, by inference, increase quality of life, such as personal satisfaction, self-esteem, improvement in headaches, and other functional criteria.
In both research focuses, the vast majority of them demonstrated an effective increase in the quality of life factor in patients undergoing surgery. In addition to the improvement in quality of life, there were reports of functional improvements and subjective criteria linked to quality of life, such as self-esteem and satisfaction. Thus, 73% of studies found some type of positive influence from blepharoplasty. However, the number of studies that have analyzed this relationship in depth is still scarce.
Regarding the inclusion of blepharoplasty in the SUS, the data found was insufficient to have a good overview, and no study was found on the subject, demonstrating a gap in scientific knowledge aimed at this purpose.
In this sense, there seems to be a neglect of this topic in public health, with the practical consequence of having a negative effect on the quality of life of many patients who have criteria and the right to undergo blepharoplasty, but who, unfortunately, are not met. Furthermore, the lack of research makes it difficult to truly understand the importance and impact of this surgery.
It is therefore encouraged to carry out studies, focused on deepening the relationship between blepharoplasty and quality of life, but mainly evaluating the impact of coverage of this procedure within the Unified Health System.
REFERENCES
1. Bhattacharjee K, Misra DK, Deori N. Updates on upper eyelid blepharoplasty. Indian J Ophthalmol. 2017;65(7):551-8.
2. Hernández Sánchez Y, Noa Hernández Y, Estrada Amador B, Rojas Rondón I, Ruiz Contrera E. Resultados funcionales de la blefaroplastia superior. Rev Cuba Oftalmol. 2021;34(1):e950.
3. Kobe GL, Labrea VN, Carvalho LRDAT. Indicações estéticas e funcionais na blefaroplastia. Congresso Internacional em Saúde. 2021 [Internet]. Disponível em: https://www.publicacoeseventos.unijui.edu.br/index.php/conintsau/article/view/18983/17716
4. Brasil. Ministério da Saúde. Regula SUS. Protocolos de encaminhamento para Cirurgia Plástica [Internet]. Brasília: Ministério da Saúde; 2019 Disponível em: https://www.ufrgs.br/telessauders/documentos/protocolos_resumos/ptrs_CirurgiaPlastica.pdf
5. Peters MDJ, Godfrey C, McInerney P, Baldini Soares C, Khalil H, Parker D. Chapter 11: Scoping Reviews. In: Aromataris E, Munn Z, eds. Joanna Briggs Institute Reviewer’s Manual. Adelaide: Joanna Briggs Institute; 2017.
6. Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467-73.
7. Papadopulos NA, Hodbod M, Henrich G, Kovacs L, Papadopoulos O, Herschbach P, et al. The Effect of Blepharoplasty on Our Patient’s Quality of Life, Emotional Stability, and Self-Esteem. J Craniofac Surg. 2019;30(2):377-83.
8. Bahceci Simsek I. Association of Upper Eyelid Ptosis Repair and Blepharoplasty With Headache-Related Quality of Life. JAMA Facial Plast Surg. 2017;19(4):293-7.
9. Ferreira FC, Sathler CSCO, Hida IY, Leite SC, Kusabara AA, de Castro ACV, et al. Upper eyelid blepharoplasty using plasma exeresis: Evaluation of outcomes, satisfaction, and symptoms after procedure. J Cosmet Dermatol. 2021;20(9):2758-64.
10. Jacobsen AG, Brost B, Vorum H, Hargitai J. Functional benefits and patient satisfaction with upper blepharoplasty - evaluated by objective and subjective outcome measures. Acta Ophthalmol. 2017;95(8):820-5.
11. Chen B, Song H, Gao Q, Xu M, Wang J, Wang F, et al. Measuring satisfaction with appearance: Validation of the FACE-Q scales for double-eyelid blepharoplasty with minor incision in young Asiansretrospective study of 200 cases. J Plast Reconstr Aesthet Surg. 2017;70(8):1129-35.
12. Hollander MHJ, Contini M, Pott JW, Vissink A, Schepers RH, Jansma J. Functional outcomes of upper eyelid blepharoplasty: A systematic review. J Plast Reconstr Aesthet Surg. 2019;72(2):294-309.
13. Pemberton JD, Salter M, Fay A, Thuro B, Spencer H, Dajani O. Investigation of Goldmann perimetry in evaluation of patients for upper eyelid blepharoplasty. Orbit. 2018;37(1):48-52.
14. Kim H, Lee S, Son D, Yeo H. Objective quantification of the impact of blepharoplasty on the superior visual field. Arch Plast Surg. 2022;49(1):19-24.
15. Domela Nieuwenhuis I, Luong KP, Vissers LCM, Hummelink S, Slijper HP, Ulrich DJO. Assessment of Patient Satisfaction With Appearance, Psychological Well-being, and Aging Appraisal After Upper Blepharoplasty: A Multicenter Prospective Cohort Study. Aesthet Surg J. 2022;42(4):340-8.
16. Herruer JM, Prins JB, van Heerbeek N, Verhage-Damen G, Ingels K. Patient-reported outcome measurement in upper blepharoplasty: How to measure what the patient sees. J Plast Reconstr Aesthet Surg. 2018;71(9):1346-51.
17. Nalcı H, Hoşal MB, Gündüz ÖU. Effects of Upper Eyelid Blepharoplasty on Contrast Sensitivity in Dermatochalasis Patients. Turk J Ophthalmol. 2020;50(3):151-5.
18. Sun W, Yin N, Song T, Wu D, Li H, Wang Y. A practical technique combining orbicularis oculi muscle resection-based epicanthoplasty and orbicularis-tarsus fixation double-eyelid plasty for cosmetic blepharoplasty. J Plast Reconstr Aesthet Surg. 2019;72(12):2009-16.
19. Zhao JY, Guo XS, Song GD, Zong XL, Yang XN, Du L, et al. Surgical outcome and patient satisfaction after Z-epicanthoplasty and blepharoplasty. Int J Ophthalmol. 2018;11(12):1922-5.
20. Kim YS, Kim BS, Kim HS, In SK, Yi HS, Kim HI, et al. Factors Influencing Patient Satisfaction with Upper Blepharoplasty in Elderly Patients. Plast Reconstr Surg Glob Open. 2021;9(8):e3727.
21. Spadoni-Pacheco LM, Carvalho GA. Qualidade de vida e autoestima em idosas submetidas e não submetidas à cirurgia estética. Rev Bras Cir Plást. 2018;33(4):528-35.
22. Gracitelli CPB, Osaki TH, Hirai FE, Yabumoto C, Viana GAP, Osaki MH. Assessment of self-esteem and psychological aspects in patients undergoing Upper blepharoplasty. Rev Bras Ofatlmol. 2017;76(6):280-4.
23. Mokhtarzadeh A, McClelland C, Lee MS, Smith S, Harrison AR. The Bleph and the Brain: The Effect of Upper Eyelid Surgery on Chronic Headaches. Ophthalmic Plast Reconstr Surg. 2017;33(3):178-1.
24. Vola ME, Lisboa R, Diniz ER, Pereira NC, Kanecadan RT, Forseto AS. Influence of upper blepharoplasty on intraocular lens calculation. Arq Bras Oftalmol. 2021;84(1):11-6.
25. Brasil. Ministério da Saúde. Datasus. Sistema de Gerenciamento da Tabela de Procedimentos, Medicamentos e OPM do SUS. 2023 [Internet]. Disponível em: http://sigtap.datasus.gov.br/tabela-unificada/app/sec/inicio.jsp
26. Brasil. Ministério da Saúde. Portaria Nº 3.037. Altera valores de procedimentos oftalmológicos na Tabela de Procedimentos, Medicamentos, Órteses, Próteses e Materiais Especiais do Sistema Único de Saúde (SUS) e estabelece o remanejamento de recursos do Fundo de Ações Estratégicas e Compensação-FAEC para Componente Limite Financeiro de Média e Alta Complexidade Ambulatorial e Hospitalar do Bloco da Atenção de Média e Alta Complexidade Ambulatorial e Hospitalar a serem incorporados aos Estados e Distrito Federal. Brasília: Ministério da Saúde; 2017.
27. Brasil. Ministério da Saúde. Cartão SUS. Cirurgia de pálpebras: Como conseguir una Blefaroplastia pelo SUS [Internet]. Brasília: Ministério da Saúde; 2022. Disponível em: https://cartaodosus.info/blefaroplastia-pelo-sus/
28. Sociedade Brasileira de Cirurgia Plástica. Censo 2016. Situação da Cirurgia Plástica no Brasil: análise comparativa entre 2014 e 2016 [Internet]. São Paulo: Sociedade Brasileira de Cirurgia Plástica; 2017. Disponível em: http://www2.cirurgiaplastica.org.br/wp-content/uploads/2017/12/CENSO-2017.pdf
29. Prefeitura de Poços de Caldas. Mutirão de cirurgias plásticas será realizado simultaneamente em 5 unidade de saúde de Poços [Internet]. Prefeitura de Poços de Caldas; 2019. Disponível em: https://pocosdecaldas.mg.gov.br/noticias/mutirao-de-cirurgias-plasticas-sera-realizado-simultaneamente-em-5-unidades-de-saude-de-pocos/
1. Pontifícia Universidade Católica de Minas
Gerais, Poços de Caldas, MG, Brazil
Corresponding author: Lucas Freire Guerra Boldrin Rua Assis Figueiredo 515, apto 107, Centro, Poços de Caldas, MG, Brazil, Zip Code: 37701-000, E-mail: guerralucas1807@gmail.com
Article received: August 13, 2023.
Article accepted: February 04, 2024.
Conflicts of interest: none.






 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter