

Original Article - Year 2024 - Volume 39 -
From Surface to Depth: Learning Curve in Extended Deep Facelift - My First 100 Cases.
Da superfície para a profundidade: Curva de aprendizado em lifting facial profundo estendido - meus primeiros 100 casos.
ABSTRACT
Introduction: Facial aging is a gradual, complex, and multifactorial process. It is the result of changes in the quality, volume, and positioning of tissues. Plastic surgeons have modified their approach to facial rejuvenation surgery, opting for the subaponeurotic plane (SMAS). The objective of this study is to analyze 100 cases of patients operated on using the deep SMAS technique, evaluating its applicability and effectiveness.
Method: 100 patients were evaluated, undergoing facial plastic surgery using the deep SMAS technique - "Deep Smas", and followed up for 6 months. Patient satisfaction, number of complications, number of reoperations, risks, and advantages of the technique were observed.
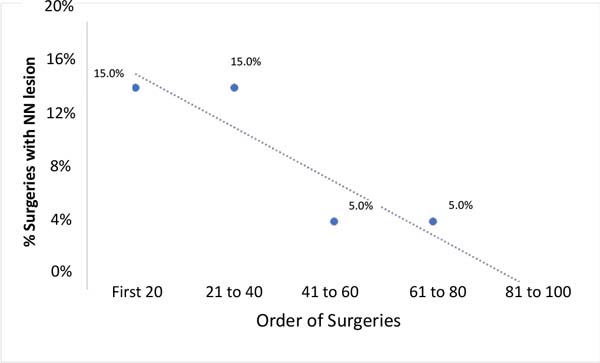
Results: 100 patients were operated on over 3 years. Age ranged from 41 to 79 years, with 95% being female. The complications were 8 cases (8%) of injuries to branches of the facial nerve, of which 4 cases of zygomatic injury, 3 cases of mandibular injury, and 1 case of buccal injury; there was 1 case (1%) of post-auricular keloid; 1 case (1%) of hematoma. Regarding surgical revisions, there were 8 cases (8%) of surgical completion due to patient dissatisfaction. There were 15% of nerve injuries between the 1st and 40th surgery, 5% between the 41st and 80th, and no injuries between the 81st and 100th patient.
Conclusion: Deep facial lifting or subSMAS has proven to be effective, providing good aesthetic results. It has a low recurrence rate and low morbidity rate; however, it requires a long learning curve.
Keywords: Face; Plastic surgery procedures; Esthetics; Cosmetic techniques; Facial nerve; Learning curve
RESUMO
Introdução: O envelhecimento facial é um processo gradual, complexo e multifatorial. É o resultado de mudanças na qualidade, volume e posicionamento dos tecidos. Cirurgiões plásticos têm modificado sua abordagem na cirurgia do rejuvenescimento facial optando pelo plano subaponeurótico (SMAS). O objetivo deste estudo é analisar 100 casos de pacientes operados pela técnica de SMAS profundo, avaliando sua aplicabilidade e eficácia.
Método: Foram avaliados 100 pacientes, submetidos a cirurgia plástica facial pela técnica de SMAS profundo - "Deep Smas", e acompanhados por 6 meses. Observou-se a satisfação dos pacientes, número de complicações, número de reoperações, riscos e vantagens da técnica.
Resultados: Foram operados 100 pacientes, num período de 3 anos. A idade variou de 41 a 79 anos, sendo 95% sexo feminino. As complicações foram 8 casos (8%) de lesões de ramos do nervo facial, sendo: 4 casos lesão do zigomático, 3 casos de lesão do mandibular e 1 caso de lesão do bucal; houve 1 caso (1%) de queloide retroauricular; 1 caso (1%) de hematoma. Em relação às revisões cirúrgicas, houve 8 casos (8%) de complementação cirúrgica por insatisfação das pacientes. Houve 15% de lesões nervosas entre a 1ª e a 40ª cirurgia, 5% entre a 41ª e a 80ª, e nenhuma lesão entre o 81º e o 100º paciente.
Conclusão: O lifting facial profundo ou subSMAS mostrou ser efetivo, proporcionando bons resultados estéticos. Apresenta baixa taxa de recidiva e baixa taxa de morbidade, porém, necessita de uma longa curva de aprendizagem.
Palavras-chave: Face; Procedimentos de cirurgia plástica; Estética; Técnicas cosméticas; Nervo facial; Curva de aprendizado.
INTRODUCTION
Facial aging is a gradual, complex, and multifactorial process. It is the result of changes in the quality, volume, and positioning of tissues1-3.
Plastic surgeons have modified their technical approach to patients who wish to undergo facial rejuvenation, including video endoscopy, cosmetic treatments such as laser, botulinum toxin, and facial fillers, and extensive knowledge of anatomy, highlighting the retaining ligaments of the face4-7. Retaining ligaments connect the loose tissues of the face to deep bony structures.
Modern facial surgery was pioneered by Skoog8, who described the elevation of the deep facial cervical flap to the platysma and superficial fascia of the face. When talking about a deep approach, Hamra9,10 and Barton11,12 added personal modifications, but maintained the concept of the flap composed of skin with the superficial muscular aponeurotic system (SMAS)13.
After a better understanding and knowledge of the system of fat compartments, both superficial and deep, described by Rohrich & Pessa6,7, added to publications by Aston13 on FAME (finger assisted malar elevation), Mendelson et al.14,15 described the importance of the facial ligaments and also the subSMAS spaces, the ligaments forming a complex fibrous support system, and the spaces that are areas delimited by the ligaments on the sides where no anatomical structures are crossing inside, that is, they are safe spaces with all nerve branches being outside these compartments.
More recently, the studies by Jacono1 stood out, which in great detail showed the advantages of releasing the retaining ligaments from the ptotic tissue of the midfacial third followed by en bloc traction, fixation, and repositioning at the level of the malar prominence and the fixed SMAS. The section of the cutaneous zygomatic ligament, the strongest ligament on the face (according to biomechanical studies)15, allows the elevation and mobilization of the malar fat pad. Tissue mobilization allows great volumization of the middle third, which is believed not to be possible with traditional SMAS flap or plication techniques, as they would not mobilize the loose tissue structures1,16-22 as studies by Gassner et al.23 demonstrated histologically, there is no SMAS tissue medial to the zygomatic muscles.
Characteristics of Mendelson Studies
The ligaments of the face resemble a tree where the trunk are the ligaments that unite the soft tissues to the facial skeleton, the larger branches cross the SMAS, and their branches (small branches) connect the SMAS to the sub-dermis (retinacular cutis fibers), forming a complex fibrous support system14,15.
The subSMAS spaces are areas delimited by retaining ligaments on the sides where no anatomical structures are crossing inside; that is, they are safe spaces with all nerve branches being outside these compartments. As they allow the movement of loose tissues, there may be sagging in these spaces and not in their limits where the ligaments are located14,15. Dissection in these areas presents less bleeding, edema, and risk of nerve injury.
Prezygomatic space: covers the zygomatic bone, the zygomatic muscles originate below the floor, the roof or lining is by the orbicularis oculi muscle and the SOOF (sub orbicular oculi fat), the upper edge by the orbicularis retaining ligament (which does not is so resistant) and the lower edge by the zygomatic ligament (this one is stronger).
Pre-masseteric space: covers the lower ½ of the masseter muscle, the platysma forms the roof, the posterior edge by the platysma auricular fascia (PAF), the anterior edge by the masseteric ligaments, and the weakness of the fixation of the floor formed by the platysma in the inferior masseteric ligament allows the formation of the jowl.
Limits of the premasseteric space:
a) Base: masseter/additional and anterior triangle;
b) Ceiling: platysma;
c) Later: transition to the PAF;
d) Superior: cutaneous masseteric ligaments;
e) Lower: membrane formed between the PAF and the mandibular ligament;
f) Anterior: membrane formed between the platysma and the masseter.
C) Chewing Space: also called the buccal space, this space contains the buccal fat and the laxity in this area allows the formation of the nasolabial fold (NLF).
When the term “deep Smas facelift” was introduced, it referred to subSMAS dissection, but it was not clear whether it involved the face laterally (here in the subcutaneous plane) until the transition of the orbicularis muscle and zygomaticus major muscle on the anterior face24,25. Hamra9,10,24,26 described access to the anterior face through the lower eyelid and zygomatic orbicularis dissection. Currently, the term compound lifting involves the dissection of the face anteriorly, always in the subSMAS plane, but with lateral access coming over the middle 1/3 of the face (mid cheek) used in our study and also recommended by Jacono1,18-20.
Different facelifting techniques offer good results. However, a deeper analysis allows us to observe that the balance between skin tension and volume or shape will determine the harmony of the face.
There are 3 areas or layers where tension can be applied to treat sagging: skin, SMAS, and periosteum. Advantages of subSMAS: spaces are naturally pre-dissected, fast, bleed little and atraumatic.
Features of Hamra Studies
Initially, Hamra9,26 described his “Deep Plane” deep dissection technique that aimed to treat sagging cheek fat that made the NLF more evident and deeper. Traction superiorly would promote attenuation of the NLF. One characteristic that stood out was that the fatty tissue was over the zygomatic muscles, was easy to dissect, and remained connected to the SMAS (“cheek fat” + platysma).
Evolving over time, he described the Composite Face Lift, which formed a flap composed of the orbicularis oculi muscle (MOO) + “cheek fat” + platysma. The incision in the arcus marginalis (junction of the septum with the orbital rhyme)10.
Finally, he described the Zygomatic Orbicularis Flap and Septal Reset, incising the orbital septum inferiorly and “redraping” the tissue superiorly, treating the nasal jugal groove, leaving it more youthful27.
Jowl
The “jowl” is a protrusion of soft tissues in the lower and anterior third of the face14,15,28-30, being the main stigma of facial aging30. Its anterior limit is the mandibular ligament and the labrum mandibular groove; it is located in the supraplatysmal plane as a redundancy of the subcutaneous tissue (fat) covered by facial skin28. The subplatysmal anatomical structures are not related to the formation of the jowl, but the adjacent structures are Bichat fat (buccal fat pad) and the submandibular gland when very prominent30. The Auersvald brothers28 believe that the main factors involved in the formation of the “jowl” are subcutaneous fat, excess skin, descending SMAS sliding and infiltrating the fat, and Bichat fat.
OBJECTIVE
The objective of this study is to analyze 100 patients operated on using the deep SMAS (Extended Deep Plane Face Lifting) technique, evaluating its applicability, effectiveness, morbidity and surgical results.
METHOD
One hundred patients were analyzed between January 2020 and November 2022 who underwent facial plastic surgery using the deep SMAS technique - “Deep Smas”, and were followed up for 6 months postoperatively (PO). The study was carried out in a private clinic in Curitiba-PR, observing the number of complications, number of reoperations, risks, and advantages of the technique. The study was previously approved by the Research Ethics Committee of Faculdade Evangélica Mackenzie do Paraná, with number 5,281,745.
Operative technique
Previous marking with methylene blue on the skin, starting at the contour of the rib of the hair, going around the entire ear, positioning post-tragal in the anterior region, in the posterior region at the transition between the turbinate cartilage and the mastoid, extending to the foot of the hair in the posterior region.
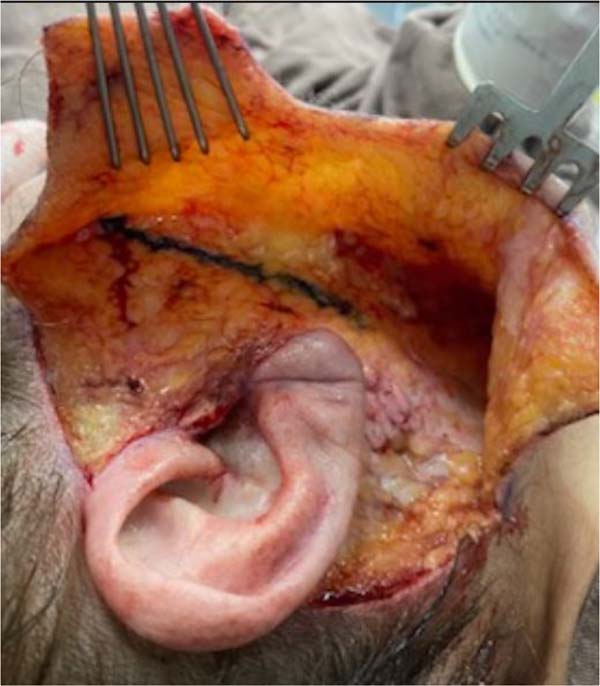
Skin incision followed by subcutaneous dissection approximately 3 cm anteriorly to where the transition line for the deep plane is located. This line runs from the lateral corner of the orbit to the angle of the mandible (gonion) (Figure 1).
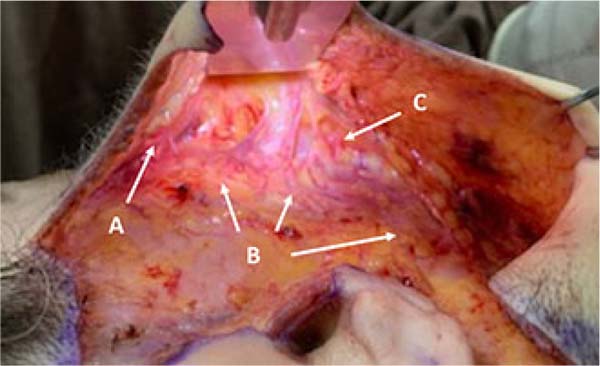
Access to the subSMAS plane is achieved through a scalpel incision. Next, using electrocautery, dissection is made in the loose areolar tissue with the branches of the facial nerve (zygomatic, buccal and marginal of the mandible) being below this plane protected by the masseteric fascia. It is followed anteriorly with blunt dissection and release of the masseteric ligaments in the superior, middle, and inferior pre-masseteric spaces. More superiorly, with the section of the cutaneous zygomatic ligament, access to the prezygomatic space is gained, and this allows communication with the premasseteric space. The zygomaticus major muscle is located in this region, below which the zygomatic branch of the facial nerve passes. The malar region is suspended after performing FAME13 using the index finger (Figure 2).
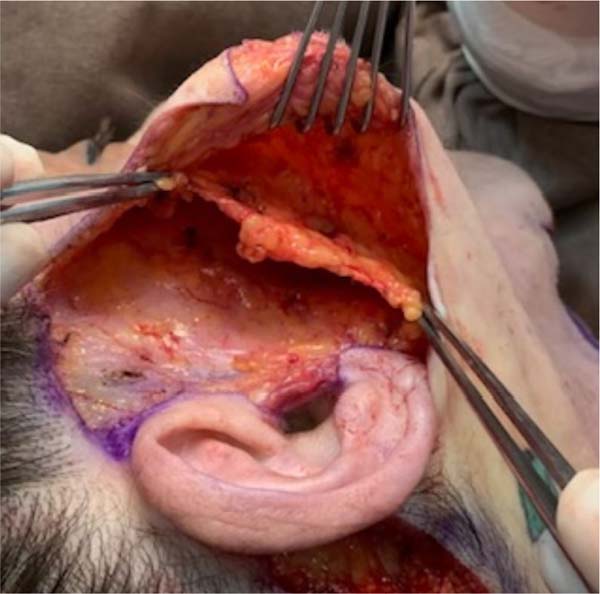
Blunt dissection continues anteriorly to the level of the NLF and inferiorly to the transition of the premasseteric space with the subplatysmal space (Figures 3 and 4). With the entire subSMAS plane dissected, the “cuff” is created, which is, on average, 2cm, a SMAS flap that will serve as anchorage supporting the traction of the fasciocutaneous flap (Figure 5). There are approximately 5 to 6 traction points made with Vycril® plastic 4.0, starting more inferiorly in a posterosuperior direction until the fixed SMAS (Figures 6 and 7).
The last step is to suture the lateral platysma, as described by Jacono1, using the hammock technique, to the mastoid periosteum (Figures 8, 9, 10, and 11). Finally, the excess skin is resected, hemostasis is reviewed, and drainage with a suction drain, accommodating the tissues without tension, with simple 4.0 Monocryl sutures in the subdermis and continuous 5.0 nylon in the skin.
Statistical analysis
Quantitative variables were described using the statistics of mean, median, minimum value, maximum value, and standard deviation. Qualitative variables were summarized using frequencies and percentages. To evaluate the association between sex and the presence of injury, the Fisher’s Exact test was considered. The association between age and presence of injury was assessed using Student’s t-test for independent samples. The association between surgery order and the presence of injury was assessed using the Cochran-Armitage test. P values lower than 0.05 indicated statistical significance.
RESULTS
One hundred patients were operated on over 3 years. Age ranged from 41 to 79 years, mean age of 58.7 years, with 95% female and 5% male (Tables 1 and 2).
| N | Average | Median | Minimum | Maximum | Standard deviation |
|---|---|---|---|---|---|
| 100 | 58.7 | 59 | 41 | 79 | 8,1 |
| Sex | N | % |
|---|---|---|
| Feminine | 95 | 95.0% |
| Masculine | 5 | 5.0% |
| Total | 100 | 100.0% |
The complications were 8 cases (8%) of injuries to branches of the facial nerve, of which 4 cases of zygomatic injury, 3 cases of mandibular injury, and 1 case of buccal injury; there was 1 case (1%) of post-auricular keloid; 1 case (1%) of hematoma (Figure 12). All nerve injuries were transient, treated with oral peripheral nerve neuroregenerators and lasting 45 to 60 days.
Regarding surgical revisions, there were 8 cases (8%) of surgical completion due to patient dissatisfaction due to sagging skin or little projection in the middle third of the face, which were carried out between 6 and 8 months postoperatively. The vast majority of patients undergoing surgical revision were over 60 years old (75%) (Table 3).
| Age | Patients | Reviews (%) |
|---|---|---|
| < 49 | 2 | 1 |
| 50-59 | 17 | 1 |
| 60-69 | 57 | 4 |
| 70-79 | 24 | 2 |
| Total | 100 | 8 |
Assessment of the association of sex with the presence of injury
The null hypothesis that the probability of the presence of a lesion in female patients is equal to the probability of the presence of a lesion in male patients was tested versus the alternative hypothesis of different probabilities. The table below presents the results obtained in the study, as well as the p-value of the statistical test (Table 4).
| NN injury | Sex | |||
|---|---|---|---|---|
| Feminine | Masculine | |||
| N | % | N | % | |
| No | 87 | 91.6% | 5 | 100.0% |
| Yes | 8 | 8.4% | 0 | 0.0% |
| Total | 95 | 100.0% | 5 | 100.0% |
p-value=1
Assessment of the association of age with the presence of injury
The null hypothesis of the mean age in cases without injury equal to the mean age in cases with injury was tested versus the alternative hypothesis of different means. The table below presents the descriptive statistics of age in each injury classification, as well as the p-value of the statistical test (Table 5).
| NN injury | N | Average | Median | Minimum | Maximum | Standard deviation | p-value* |
|---|---|---|---|---|---|---|---|
| No | 92 | 58.9 | 59 | 41 | 79 | 8.3 | 0.504 |
| Yes | 8 | 56.9 | 57.5 | 45 | 64 | 6.1 |
(*) Student’s t-test for independent samples; p<0.05.
Evaluation of the association between the order of surgery and the presence of injury
The null hypothesis of an association between the order in which surgeries are performed and the probability of presence of injury was tested versus the alternative hypothesis of no association between the order in which surgeries are performed and the probability of presence of injury. To apply the test, the surgeries were grouped into classes with 20 surgeries considering the order in which they were performed. This way, the first 20 were carried out before the next 20 and so on.
The results obtained in the study are presented in the table below (Table 6).
| Surgeries | Surgeries | % with injury | ||
|---|---|---|---|---|
| With NN injury | No NN injury | Total | ||
| 1 to 20 | 3 | 17 | 20 | 15.0% |
| 21 to 40 | 3 | 17 | 20 | 15.0% |
| 41 to 60 | 1 | 19 | 20 | 5.0% |
| 61 to 80 | 1 | 19 | 20 | 5.0% |
| 81 to 100 | 0 | 20 | 20 | 0.0% |
| Total | 8 | 92 | 100 | 8.0% |
p-value=0.037
The result of the statistical test indicated the rejection of the null hypothesis (p=0.037), providing evidence for the finding that there is a tendency for the probability of the presence of an injury to decrease as experience with performing surgery increases.
The results obtained in the study can be seen in the graph below (Figure 13).
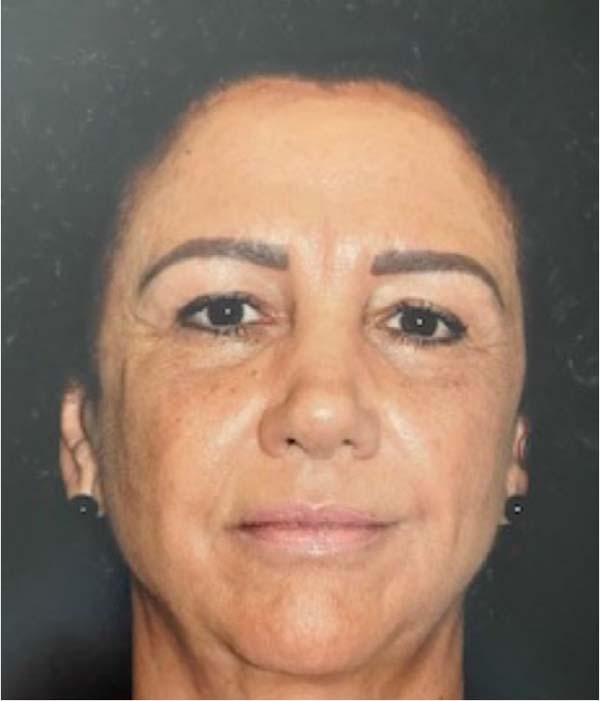
Below, some preand postoperative cases are presented (Figures 14, 15, 16, 17, 18, 19, 20 and 21).
DISCUSSION
The learning curve was described in 1936 by Wright31 and can be defined as the graphic expression representing the period of incorporation of new knowledge. In practice, it has been confused with the number of procedures necessary to reach the point of proficiency, with the point of proficiency being understood as the moment at which the optimization of this procedure is achieved or, better said, it is the moment at which the surgeon can perform the procedure without supervision32.
The Sociedade Brasileira de Vídeo Cirurgia (Brazilian Society of Video Surgery) establishes the minimum number of procedures performed at 25 for the surgeon to be considered qualified33. In plastic surgery, data are sparse, but Tapking et al.34 reviewed 29 articles that indicate that the learning curve reaches a plateau between 45-100 cases operated in breast reconstruction. This translates into a higher success rate, shorter surgical time, and lower complication rate.
The deep approach in facial surgery, also called deep lifting, subSMAS, or deep plane, began with the publications by Hamra9,10 and Barton11,12, but it was only after the studies by Mendelson et al.14,15 that it was understood that more clearly and in detail the anatomy of this region. The diffusion and “popularization” of the technique, so to speak, among plastic surgeons around the world and even among lay people occurred mainly through the studies of Jacono1,18,19,20.
Both Jacono1 and Mendelson et al.14 propose the dissection and approach of the prezygomatic space, all premasseteric spaces, and the masticatory space. From here onwards, Jacono1 proposes the realization of FAME, but in a different way from Aston13. This approaches with the index finger sliding below the orbicularis muscle to the malar fat pad, while Jacono1 advises the use of the index finger over the orbicularis muscle, as a way of protecting the zygomatic branch of the facial nerve.
Another distinct characteristic occurs in the treatment of the platysma muscle. Jacono1 proposes blunt dissection anteriorly to the level of the NLF and inferiorly to the transition of the premasseteric space with the subplatysmal space. With the subplatysmal dissection performed both via the middle third of the face and through the lateral platysma, there is a platysma flap called a hammock platysma (swing hammock) that will be anchored in the periosteum of the mastoid process with suture threads.
Jacono1 recommends the use of nonabsorbable monofilament threads to fix the composite flap, with an average number of 6 sutures. It justifies the use of nylon so that, if in the future there is a new reintervention of the face, the surgeon can find the threads and that they serve as a guide or parameter for a new sub-SMAS plane dissection. In this study, absorbable multifilament 4.0 Vycril® plastic threads were used, which, due to technical characteristics, would cause a greater inflammatory reaction and consequently greater adhesion and fixation of the flap than monofilament thread (nylon). Disadvantages include the risk of visualizing the black nylon threads in the subdermis and the palpation of knots in the event of a foreign body reaction (nonabsorbable threads).
The biggest concern for the patient and the facial surgeon is the risk of nerve injury, which is the reason to avoid some techniques that involve wider dissections such as subSMAS or deep plane. Despite speculation, most individual case series consider rates of temporary nerve injury to be between 1% and 2%, regardless of the technique used. Permanent injuries vary from 0.04% to 0.08%35. Jacono18,22, in 584 patients, reported 1% of temporary injuries and 0% of definitive injuries, mainly attributing to the connections between the buccal and zygomatic branches, the possibility of direct vision of the branches, and the protection of the parotid masseteric fascia.
In this study, it was observed, after completing the learning curve - that in plastic surgery, between 45-100 cases34 can be considered, values equal to those of other techniques and also to those of Jacono18,22, with a regressive character tending to 0% in the last 20 operated cases. Furthermore, there were also no cases of definitive nerve damage, which is also similar to the literature18,22,35 (p=0.037).
Regarding surgical revision rates, Jacono1,18,22 cites values between 3% and 5% in more than 2000 cases operated in around 11 years. Moreover, it corroborates its results with the publication by Kamer & Frankel36, who cite values of 3.3% of surgical revisions in other studies in which the techniques were SMASectomy, SMAS imbrication, and SMAS plication. Surgical revisions within 1 year were between 11.4% and 21.7%36. Jones & Lo37, in turn, showed a 69% recurrence of flaccidity in the angle of the mandible and cervical region in a 5.5-year follow-up period. In this study, values of 1% were found in patients under 60 years old, 4% between 60 and 70 years old, and 2% between 70 and 79 years old. This is similar to literature data, as Jacono1 mentions that revisions increase in older patients, reaching 100% in patients over 80 years old and 50% in patients between 70 and 79 years old.
Different facelifting techniques can offer good results, leaving both the patient and the surgeon satisfied, and each surgeon needs to develop their own approach that provides desired and long-lasting results. However, a deeper analysis allows us to observe that the balance between skin tension and volume or shape will determine the harmony of the face. The deep approach to facial surgery, also called deep lifting, subSMAS, or deep plane, provides more effective and long-lasting results with a low rate of surgical revisions1,36,37.
CONCLUSION
The deep facial lifting technique or subSMAS (Extended Deep Plane Face Lifting) has proven to be effective, providing good aesthetic results, and has a low recurrence rate and low morbidity rate; however, it requires a long learning curve.
REFERENCES
1. Jacono AA. A Novel Volumizing Extended Deep-Plane Facelift: Using Composite Flap Shifts to Volumize the Midface and Jawline. Facial Plast Surg Clin North Am. 2020;28(3):331-68.
2. Warren R, Gartstein V, Kligman AM, Montagna W, Allendorf RA, Ridder GM. Age, sunlight, and facial skin: a histologic and quantitative study. J Am Acad Dermatol. 1991;25(5 Pt 1):751-60.
3. Coleman SR, Grover R. The anatomy of the aging face: volume loss and changes in 3-dimensional topography. Aesthet Surg J. 2006;26(1S):S4-9.
4. Ferreira LM, Horibe EK. Understanding the finger-assisted malar elevation technique in face lift. Plast Reconstr Surg. 2006;118(3):731-40.
5. Furnas DW. The retaining ligments of the cheek. Plast Reconstr Surg 1989;83(1):11-6.
6. Rohrich RJ, Pessa JE. The fat compartments of the face: anatomy and clinical implications for cosmetic surgery. Plast Reconstr Surg. 2007;119(7):2219-27.
7. Rohrich RJ, Pessa JE. The retaining system of the face: histologic evaluation of the septal boundaries of the subcutaneous fat compartments. Plast Reconstr Surg. 2008;121(5):1804-9.
8. Skoog T. Plastic Surgery: New Methods and Refinements. Philadelphia: Saunders; 1974. p. 300-30.
9. Hamra ST. The deep-plane rhytidectomy. Plast Reconstr Surg. 1990;86(1):53-61.
10. Hamra ST. Composite rhytidectomy. Plast Reconstr Surg. 1992;90(1):1-3.
11. Barton FE Jr. The SMAS and the nasolabial fold. Plast Reconstr Surg. 1992;89(6):1054-7.
12. Barton FE Jr. The “high SMAS” face lift technique. Aesthet Surg J. 2002;22(5):481-6.
13. Aston SJ. The FAME technique, presented at the Aging Face Symposium. Waldorf Astoria Hotel, New York; 1993.
14. Mendelson BC, Muzaffar AR, Adams WP Jr. Surgical anatomy of the midcheek and malar mounds. Plast Reconstr Surg. 2002;110(3):885-96; discussion 897-91.
15. Mendelson BC, Freeman ME, Wu W, Huggins RJ. Surgical anatomy of the lower face: the premasseter space, the jowl, and the labiomandibular fold. Aesthetic Plast Surg. 2008;32(2):185-95.
16. Hashem AM, Couto RA, Duraes EFR, Çakmakoğlu Ç, Swanson M, Surek C, et al. Facelift Part I: History, Anatomy, and Clinical Assessment. Aesthet Surg J. 2020;40(1):1-8.
17. Brandt MG, Hassa A, Roth K, Wehrli B, Moore CC. Biomechanical properties of the facial retaining ligaments. Arch Facial Plast Surg. 2012;14(4):289-94.
18. Jacono AA, Parikh SS. The minimal access deep plane extended vertical facelift. Aesthet Surg J. 2011;31(8):874-90.
19. Jacono AA, Malone MH. Characterization of the Cervical Retaining Ligaments During Subplatysmal Facelift Dissection and its Implications. Aesthet Surg J. 2017;37(5):495-501.
20. Jacono AA, Bryant LM, Ahmedli NN. A Novel Extended Deep Plane Facelift Technique for Jawline Rejuvenation and Volumization. Aesthet Surg J. 2019;39(12):1265-81.
21. Graf R, Groth AK, Pace D, Graça Neto L. Facial rejuvenation with SMASectomy and FAME using vertical vectors. Aesthetic Plast Surg. 2008;32(4):585-92.
22. Graf R, Graça Neto L, Araújo LR, Bernardes A, Rippel R, Auersvald A. Vertical vectors in SMASectomy to reshape the aging face. Aesthet Surg J. 2003;23(3):198-201.
23. Gassner HG, Rafii A, Young A, Murakami C, Moe KS, Larrabee WF Jr. Surgical anatomy of the face: implications for modern face-lift techniques. Arch Facial Plast Surg. 2008;10(1):9-19.
24. Hamra ST. The zygorbicular dissection in composite rhytidectomy: an ideal midface plane. Plast Reconstr Surg. 1998;102(5):1646-57.
25. Stuzin JM, Baker TJ, Gordon HL, Baker TM. Extended SMAS dissection as an approach to midface rejuvenation. Clin Plast Surg. 1995;22(2):295-311.
26. Hamra ST. Deep plane facelift. In: American Society of Aesthetic Plastic Surgery Midwinter Symposium of Facial Rejuvenation; 1989 Jan 12-13; Santa Barbara; CA, USA.
27. Hamra ST. Building the Composite Face Lift: A Personal Odyssey. Plast Reconstr Surg. 2016;138(1):85-96.
28. Auersvald A, Auersvald LA. Anatomia Cirúrgica da Face e do Pescoço. In: Full Face & Neck Surgical Anatomy; 2020 Mar 6-8; São Paulo, SP, Brasil.
29. Auersvald LA, Auersvald A. The Short Neck: Challenges and Techniques. Facial Plast Surg. 2022;38(6):650-67.
30. Minelli L, Yang HM, van der Lei B, Mendelson B. The Surgical Anatomy of the Jowl and the Mandibular Ligament Reassessed. Aesthetic Plast Surg. 2023;47(1):170-80.
31. Hopper AN, Jamison MH, Lewis WG. Learning curves in surgical practice. Postgrad Med J. 2007;83(986):777-9.
32. Santos EG, Bravo Neto GP. Curva de aprendizado e lesões iatrogênicas em colecistectomias videolaparoscópicas. Rev Col Bras Cir. 2010;37(3):184-9.
34. Tapking C, Kowalewski KF, Hundeshagen G, Kneser U, Hirche C. A Systematic Review of Learning Curves in Plastic and Reconstructive Surgery Procedures. Ann Plast Surg. 2020;85(3):324-31.
35. Jacono AA, Alemi AS, Russell JL. A Meta-Analysis of Complication Rates Among Different SMAS Facelift Techniques. Aesthet Surg J. 2019;39(9):927-42.
36. Kamer FM, Frankel AS. SMAS rhytidectomy versus deep plane rhytidectomy: an objective comparison. Plast Reconstr Surg. 1998;102(3):878-81.
37. Jones BM, Lo SJ. How long does a face lift last? Objective and subjective measurements over a 5-year period. Plast Reconstr Surg. 2012;130(6):1317-27.
1. Clínica Privada, Curitiba, PR,
Brazil
2. PUC Pr, Curso de Medicina, Curitiba, PR,
Brazil
3. Faculdade Evangélica Mackenzie de Medicina,
Curitiba, PR, Brazil
Corresponding author: Lincoln Graça NetoRua Alferes Ângelo Sampaio, 2029, Batel, Batel, PR, Brazil, Zip Code: 80420-160, E-mail:lgracaneto@hotmail.com lgracaneto@hotmail.com
Article received: June 5, 2023.
Article accepted: August 20, 2023.
Conflicts of interest: none.









































 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter