

Articles - Year 2001 - Volume 16 -
Plastic Surgical vs. Prosthetic Reconstruction after Total Loss of the Orbital Contents and the Auricle
Cirurgia Plástica ou Reconstrução Protética na Perda Total do Conteúdo Orbitário e do Pavilhão Auricular
ABSTRACT
In the reconstruction of facial defects, there are two competing approaches: transplantation of body tissue and the use of foreign material. Most clinics prefer either the one or the other technique, which makes comparison difficult. At the Frankfurt University Medical School since 1992, cases of plastic surgical and prosthetic reconstruction of particularly difficult regions after orbital exenteration (n = 13) and total auricular loss (n=5) were examined in relation to the medical literature, in order to enable a critical evaluation. Today, facial prostheses still are esthetically superior to plastic surgical reconstructions and need much less time and interventions. Age and general condition of a patient are important for the decision. In the case ofthe auricle, autologous reconstruction is preferred whenever possible. While facial prostheses are seen today in many cases as a practical means of rehabilitation which can help the heavily disfigured patient at short notice, the future, however, lies with autologous replacement despite the larger amount of work required.
Keywords: Auricle reconstruction; orbital reconstruction; facial prosthesis
RESUMO
Na reconstrução de defeitos faciais, duas opiniões rivalizam entre si: o auto-enxerto e o uso de material aloplástico. A maioria das clínicas opta entre uma ou outra técnica, o que torna difícil a comparação entre elas. A fim de chegar a uma avaliação crítica, apresentamos os prós e os contras da cirurgia plástica e da reconstrução protética de regiões particularmente difíceis, depois de exenteração orbitária (n=13) e perda total do pavilhão auricular (n=5), entre a população de pacientes da Faculdade de Medicina da Universidade de Frankfurt a partir de 1992, com base em exemplos típicos e na literatura. Atualmente, as próteses faciais ainda são esteticamente superiores às reconstruções cirúrgicas e requerem muito menos tempo e intervenções. A idade do paciente e seu estado geral são levados em consideração para decisão. No caso do pavilhão auricular, sempre que possível, deve-se optar pela reconstrução autóloga. Embora atualmente as próteses faciais possam ser vistas, em muitos casos, como uma forma possível de reabilitação imediata que pode auxiliar o paciente excessivamente desfigurado, o futuro, entretanto, pode estar na reconstrução autóloga, apesar de ser uma solução muito mais trabalhosa.
Palavras-chave: Reconstrução do pavilhão auricular; reconstrução orbitária; prótese facial
In the reconstruction of facial defects, there are two the competing approaches: transplantation of body tissue and the use of foreign material(1). Most clinics use one of the two techniques and, therefore, prefer that one nearly exclusively. This makes comparison of the tech niques difficult. The goal always is to obtain a result as similar to narure as possible. Concerning this goal, not only the esthetics have to be considered, but rather also the function of the tissue or the replacement and compatibility of the repair vis-à-vis the surrounding host tissue. Particularly sensitive regions are the orbit and the auricle. If they are affected by malformation, traumas and by ablative interventions and the orbit is emptyor the whole auricle is lost, both patient and physician are confron difficult after an orbital exenteration with partial or complete removal of the eyelids. The surgical creation of an eye socket that can receive an eye prosthesis should mask the loss of the eye. Here a facial prosthesis may offer an esthetically superior alternative but remains problematic for the patient because of the possible spontaneous loosening. An exterior ear is not valued as critically in esthetic terms. The reconstruction with body material can be particularly difficult, however. In the present article, a comparison of the techniques is presented based on examples. Their pros and cons are discussed. Because it concerns an infrequent problem, a critical evaluation is presented. Partial losses of the auricle make their own demands; their discussion is omitted in this paper.
PATIENTS AND METHODS
In the time from 1992 to 1999, 13 patients have been treated after an orbital exenteration either prosthetically (n = 11) or by plastic reconstructive surgery (n=2). The histologic diagnoses comprised 5 cases of squamous cell carcinomas of the maxillary sinus, 2 adenoidcystic carcinomas and basal cell carcinomas of the periorbital region, respectively, and one rhabdomyosarcoma of the orbit, an osteosarcoma of the maxilla, a sebaceous gland carcinoma of the upper eyelid and an aspergillosis of the maxillary sinus, respectively. Treatment concerned three women and 10 men between 28 and 79 years.
Patients treated by autogenous reconstruction were two men with the diagnoses basal cell carcinoma and osteosarcoma. The orbit was filled with a temporal muscle flap(2), the temporal region with a Palacos implant (approximately 10 days of stay on the ward) to build a new conjunctival sulcus, oral mucosa and split thickness skin grafts from the upper arm were transplanted (approximately 1 week stay on the ward). After creation of a stable sulcus for the upper and lower lid, eye prostheses were inserted.
For the fixation of the orbital prostheses, between two and four endosseous implants were inserted in the orbital rim during a 2 day stay on the ward; in 9 cases dental Bone-Lock implants (Howmedica Leibinger, Freiburg, Germany) with subsequent out-patient bar and/or telescope retention of the prostheses(3), in two cases craniofacial Branemark implants (Noble Phanna, Goteborg, Sweden) with subsequent out-patient magnet retention(4), after a 3 month healing phase, respectively. In 9 cases, orbital prostheses have been completed and carried with an average observation time of 3 years. Two patients died before completion.
Since 1996, complete losses of an auricle have been treated in two cases prosthetically and in three cases by reconstruction with rib cartilage. Hernifacial microsomias with subtotal or complete deficiency of an ear were treated in three cases (two plastic reconstructive cases), once a malignant melanoma (prosthe thesis) and once a traffic accident in an open car (rean construction) led to the loss of an auricle. Treatment concerned a woman and four men aged between 17 and 75 years.
The method of total ear reconstruction out of rib carrtilage in a first step and dorsal lining with a temporal fascia flap and a spit skin graft in the second step was based upon a proposal of Nagata(5) (approximately 10 days stays on the ward each time). The ear lobules were preserved and were included respectively. In one patient with hemifacial microsomia and preexisting psychical over reaction, there were patient acceptance problems despite a good auricle relief whereon the second phase (loosening of the dorsal part of the auricle) was not performed and further mterventlons were refused. In the trauma patient, the transplant was lost due to a bad vascularization of the receiving bed. The probable cause was scars in the temporal reo-ion from wounds suffered in the accident. The patient wishes to undergo a second attempt following a rotation plasty with healthy skin from the neck.
For the fixation of the ear prostheses two or three craniofacial Branemark implants were used exclusively, with magnetic retention(4). For the implant insertion the patients were hospitalized for 2 days.
CASES
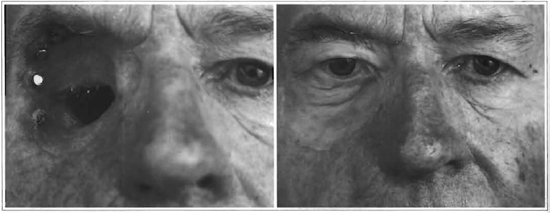
RA, 20 years old, male; with the diagnosis osteosarcoma of the maxilla on the right side, a hemimaxillectomy had to be undertaken including an exenteration of the right orbit by which means a continuous defect from the orbit to the oral cavity emerged (Fig. 1a). Subsequently, a polychemotherapy lasting several weeks took place following the COSS-scheme. After two years free from recurrence, the orbit was filled with a temporal muscle flap. A microsurgical solution comprising a scapula flap for reconstruction of the orbital floor was refused. Two months later the conjunctival sack of the upper and lower eyelid was reconstructed with a split skin graft of the right upper arm. Recurrent symblephara and shrinkage could be detached two and four months later. The lid fissure was kept open with Illig plastic shells of increasing sizes. Finally, after further 5 months, the upper conjunctival fold was reconstructed with oral mucosa and three months after that the final eye prosthesis was inserted. The hard palate was closed with a Millard island-flap. On this occasion a tightening of the right upper eyelid could take place combined with an elevation of the hanging eyelashes. Because of the lack of caudal support of the muscle transplant, there is an impression ofa slight enophthalmos on the right side (Fig. 1b).

Figs. 1a & 1b. 1a -Preoperative view of empty right orbit (patient RA). Nore the inverted eyelashes. 1b -Postoperarive view showing good result. Slight enophthalmos resulting from lacking caudal support of the temporal muscle graft.
ST, 66-year old, male, presented with a recurrence of a solid basal cell carcinoma in the left medial canthal area. The primary tumor had been operated on several times and had been irradiated three years before with 50 Gy. After resection under sacrifice of the medial two-thirds of the upper lid and canthal area, the defect was closed with a glabella flap. Two and a half years later it recurred and this led to the exenteration of the right orbit (Fig. 2a). Based on the strong psychical concerns of the patient, the orbit was filled up with a temporal muscle transplant three months later. The caudal conjunctival sack was reconstructed with oral mucosa two months later. The main problems were recurrent symplephara, that required detachment 3 times and the creation of an upper lid sulcus and a medial part ofthe upper lid. A transposition flap from above the brow and a nasal transposition flap brought no success until finally, 18 months after the filling of the orbit, a stable condition was achieved with a transposition flap harvested out of the medial forehead skin together with a lateral upper lid sliding plasty. Some days later, after few months carrying of an Illig plastic shell, the final eye prosthesis could be inserted (Fig.2b).

Fig. 2a & 2b. 2a -Preoperative view of empty left orbit (patient ST). Note multiple scars at the medial canthus and the defect of the upper lid. 2b -Postoperative view showing acceprable result.
KL, 75-year old, male. Exenteration of the right orbit was caused by a squamous cell carcinoma of the maxillary sinus, followed by chemotherapy with cisplatin and 5-fluorouracil (Fig. 3a). 13 months later, insertion of 5 craniofacial Branemark implants in the lateral orbital rim was performed; after 5 months exposure of the implants with explantation of one implant due to insufficient osseointegration; a further month later the tissue was trinuned to restrict movement around the implants; three months later finally the integration of a prosthesis with magnet retention (Fig. 3b).
Figs. 3a & 3b. 3a -Empty right orbit with magnetic abutments of the craniofacial endosseous implants (patient KL). 3b -Orbital prosthesis in site. Excellent result.
TÜ, 17-year old, male. Microtia due to a right-sided hemifacial microsomia (Fig. 4a); a total ear reconstruction one year later with cartilage of the 6th to 9th rib to the right according to the Nagata procedure with inclusion of the redesigned remnant of the lobule. Facial asymmetry caused slightly caudal placement of the auricle. A half year later the ear was folded outward and the dorsum covered with a temporal fascia flap and full skin from the right inguinal region. The patient accepted the new auricle without problems and is socially completely rehabilitated for 3 years and practices sports enthusiastically (Fig. 4b and C).
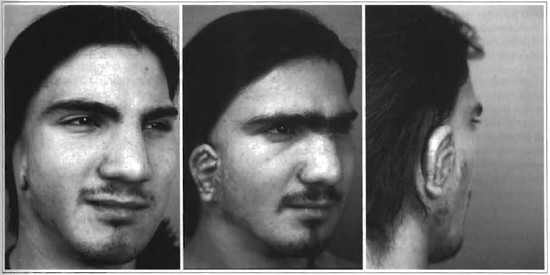
Figs. 4a -4c. 4a -Preoperative view (patient TU) with hemifacial microsomia and microtia on the right side. 4b -Postoperative view after reconstruction. Placement of new amicie is determined by the lobule and facial asymmetry. 4c -Postoperative view from behind to show good projection of the auricle.
KR, 44-year old, female. The complete ablation of the left auricle was carried out together with an ipsilateral neck-dissection because of a melanoma of the skin of the auricle. After 10 months two craniofacial Branemark implants were inserted into the mastoid, 6 months later the fixtures were exposed and the periimplant skin thinned. The prosthesis with magnet retention could be mounted two months later (Fig. 5a and B).
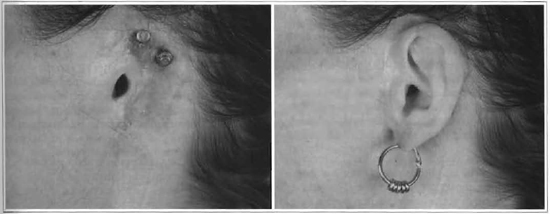
Figs. 5a & 5b. 5a -Complete loss of left auricle, scar resulting neck dissection (patient KR). Magnetic abutments of the craniofacial endosseous can be seen. 5b -Ear prosthesis in site. Excellent result.
RESULTS
1. Both groups of patients were content with the respective reconstruction and were socially well integrated. The esthetics of the facial prostheses were better.
2. The duration of the stays on the ward was about 10 fold longer with the plastic surgical reconstructions. Also the total period of the reconstructive treatment was about 2 to 3 fold longer.
3. The age and the general condition of a patient are extremely important for the decision: an active young patient would not accept a removable prosthesis, if informed about all possibilities.
4. The auricle requires a different approach than the orbit. Since there are no mobile parts and facial expression is not involved, a decision in favor of a plastic reconstruction can be made more easily, if no contraindications are present.
DISCUSSION
The action after orbital resections depends on the defect(6). The procedures for the orbit involving total eye socket reconstruction, also may be carried out with free, microsurgically anastomized transplants (e.g. radial forearm flap, groin flap). This technique is thought not to be prone to shrinkage(7).The temporal blood vessels are used for anastomosis. Even if the number of interventions can be ideally reduced to two, if optimal eyelid and conjunctival conditions exist, reconstructive intervention remains difficult and is therefore in the majority of cases reserved for younger patients(1). The temporal muscle flap is not obsolete, especially as there is essentially no donor-site morbidity(8). From the view point of follow up care of tumor patients, the resection should be done with healthy margins because a local inspection is hindered by a plastic surgical reconstruction which can conceal a recurrence. The esthetic effect of reconstructions with body tissue is probably never optimal, but that should be interpreted as a surgical challenge, especially when looking at new techniques. Without any doubt a reconstruction with autologous material is a more natural approach that improves the patient's own body image, and that even with an older patient is more highly appreciated than a prosthesis, as shown in the above example. The facial prosthesis has psychologically a poor image because the defect is only covered by a removable tool, even if it offers an outstanding esthetic result. There is a new generation of orbital prostheses, which have movable eyelids to enhance vivid expression(9) but this doesn' t change the situation decisively. Further disadvantages of the prosthetic reconstruction are the possibility of losing the prosthesis in spite of improved retention (endosseous implants and magnetic devices) and the fact that it does not change color with seasons as does the surrounding skin and must be renewed at regular intervals. In addition, these check-ups remind the patient of the defect, which he must see during the daily cleaning of the prosthesis. Incontestable advantages of the prosthetic care are its fast, secure and simple integration that does not present a major surgical challenge. The skill of the creator of these prostheses should also be mentioned(10). The ability to perform local inspection is medically important in cases with a highly probable recurrence. Here, the prosthesis is suited to achieve social rehabilitation of the patient in the remaining observation time. With defects caused by an accident this argument for a facial prosthesis is not relevant.
The situation in the region of the ear must be judged differently. For one, it is not so esthetically sensitive as the eye. The feeling of a defect is not as strongly pronounced in the patients. Again and again patients reject reconstruction or replacement of partial or total losses because they have accepted the condition. Often hair, especially in women, covers the defect. In addition, the ear possesses no mobile and fine elements as the eye and the eyelids and can therefore be fonned basically in toto out of cartilage parts put together. It is surely left to the skill and the experience of the operating surgeon, how exact and natural the reconstructed ear turns out to be, and the esthetic argument for a prosthesis in this case is clearly weakened. Often the problem of the necessary inclusion of hairy skin for the covering of the transplant develops, which can be solved by laser epilation. So if surgical experience for a good reconstruction is not sufficient, the transfer into a center with experience should not be postponed(11, 12). An additional argument for an auricular prosthesis can be the hidden attachment of hearing assistance, which concerns another group of patients(13) .
In conclusion the reconstruction with autologous material should remain the ideal goal. Attempts to bring cartilage and other tissue into the desired form has promise for success of auricle reconstruction in the near future(14). That would lead to a clear decline of the donor-site-morbidity with a reduction of the stress of the patient. Facial prostheses are to be seen today in many cases as a practical means of fast rehabilitation, with the ability to help heavily disfigured patients immediately. However, the future should not be seen in this type of prosthetic replacement.
REFERENCES
1. SCHWENZER N. Grenzen der Rekonstruktion der Lider und einer prothesenfähigen Augenhöhle. In: Schwipper, V., and Tilkorn, H. (eds). Fortschritte in der kraniofazialen chirurgischen Prothetik und Epithetik. Reinbek: Einhorn-Presse Verlag, p. 94-8,1997.
2. TESSIER P, KRASTINOVA D. Transposition of the temporalis muscle into an anophthalmic orbit. Ann. Chir. Plast. 1982;27:212-20.
3. KOVÁCS AF. A follow-up study of orbital prostheses supported by dental implants. J. Oral Maxillofac. Surg. 2000;58:19-23.
4. NESTLE B, CORNELIUS CP, SCHWENZER N. Enossale Implantate nach -Tumorresektion im Gesichtsbereich. Mund Kiefer GesichtsChir. 1999; 3 (Suppl 1):130-2.
5. NAGATA S. A New Method of Total Reconstruction of the Auricle for Microtia. Plast. Reconstr. Surg. 1993;92:187-201.
6. LEVIN PS, ELLIS DS, STEWART WB, TOTH BA. Orbital exenteration. The reconstructive ladder. Ophthal. Plast. Surg. 1991;7:84-92.
7. GUBISCH W, GREULICH M. Zum Problem der Orbitarekonstruktion. Klin. Mbl. Augenheilk. 1990;197:522-6.
8. SCHICK B, SCHAUSS F, DRAF W, CONSTANTINIDIS J. Possible indications for temporalis muscle flaps in plastic-reconstructive surgery of the head and neck. Laryngorhinootologie 1997;76:235-40.
9. KLEIN M, MENNEKING H, SCHMITZ H, LOCKE HG, BIER J. A new generation of facial prostheses with myoelectrically driven moveable upper lid. Lancet. 1999;353:1493.
10. SCHILLING N. Der große Orbitadefekt - Möglichkeiten und Grenzen der epithetischen Versorgung. In: Schwipper V, and Tilkorn H. (eds). Fortschritte in der kraniofazialen chirurgischen Prothetik und Epithetik. Reinbek: Einhorn-Presse Verlag. p. 103-6,1997
11. Brent B. Auricular repair with autogenous rib cartilage grafts. Two decades of experience with 600 cases. Plast. Reconstr. Surg. 1997;90:353-74.
12. Firmin F. Value of tissue expansion in total reconstruction of the external ear. Ann. Chir. Plast. Esthet. 1996;41:495-502.
13. Federspil P, Kurt P, and Koch A. Bone-anchored epitheses and audioprostheses: 4 years' experience with the Branemark system in Germany. Rev. Laryngol. Otol. Rhinol. (Bord). 1992;113:431-7.
14. Yotsuyanagi T, Urushidate S, Watanabe M, and Sawada Y. Reconstruction of a Three-Dimensional Structure Using Cartilage Regenerated from the Perichondrium of Rabbits. Plast. Reconstr. Surg. 1999;103:1120-3.
I - Frankfurt University Medical School, Department of Maxillofacial Plastic Surgery, Frankfurt am Main, Germany.
Address for correspondence:
Adorján Ferenc Kovács MD, DMD
Klinik fur Kiefer- und Plastische Gesichtschirurgie Universitätsklinik Haus 21
Theodor-Stern-Kai 7
D-60590 Frankfurt am Main- Germany


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter