

Case Report - Year 2023 - Volume 38 -
Dermatofibrosarcoma in glabella: An uncommon location
Dermatofibrossarcoma na glabela: Uma localização incomum
ABSTRACT
Dermatofibrosarcoma is a rare cancer with a slow growth pattern and aggressive
tissue invasion. The treatment for this condition involves surgical intervention
to achieve clear margins. In this particular case, we have a 60-year-old man who
had a mass in the glabella area that was excised twice under local anesthesia at a
different facility. The results of both biopsies indicated dermatofibroma. However,
the patient experienced a new recurrence, and during the immunohistochemistry
analysis of the initial excision, it was revealed to be dermatofibrosarcoma. As a result,
a broad excision was performed until negative margins were obtained based on
frozen sections. Additionally, a frontal flap was employed to reconstruct the surgical
defect. The outcome of the treatment was deemed successful, without complications.
Keywords: Dermatofibrosarcoma; Skin neoplasms; Mohs surgery; Head and neck neoplasms; Reconstructive surgical procedures.
RESUMO
O dermatofibrossarcoma é um câncer raro que apresenta padrão de crescimento lento
e invasão tecidual agressiva. O tratamento para esta condição envolve intervenção
cirúrgica com o objetivo de obter margens livres. Neste caso particular, temos um
homem de 60 anos que apresentava uma massa na região da glabela que foi extirpada
duas vezes sob anestesia local em outro serviço. Os resultados de ambas as biópsias
indicaram dermatofibroma. No entanto, o paciente apresentou nova recidiva,
que durante a análise imuno-histoquímica da excisão inicial revelou tratar-se de
dermatofibrossarcoma. Como resultado, uma ampla excisão foi realizada até que
margens negativas fossem obtidas ao exame de congelação. Além disso, um retalho
frontal foi empregado no procedimento para reconstrução do defeito cirúrgico.
O resultado do tratamento foi considerado bem-sucedido, sem complicações.
Palavras-chave: Dermatofibrossarcoma; Neoplasias cutâneas; Cirurgia de Mohs; Neoplasias de cabeça e pescoço; Procedimentos cirúrgicos reconstrutivos
INTRODUCTION
Dermatofibrosarcoma is a rare cancer, representing 1% of all skin sarcomas and less than 0.1% of all tumors1. This disease was initially reported by Darier and Fernand in 1924 as an unfamiliar condition and only later identified by Hoffman as dermatofibrosarcoma2.
It is considered an uncommon soft tissue tumor, affecting approximately 0.8 to 5 people per million3. The proportion of affected individuals is similar between men and women. Although it can occur at any age, it is most commonly observed from the second to the fifth decade of life2.
The tumor exhibits characteristics such as slow growth, aggressive tissue invasion, and a high risk of recurrence. However, metastasis is rarely observed3. Initially, it was believed to originate from fibroblasts, but immunohistochemistry analysis suggested its origin from dendritic cells of the skin4.
Dermatofibrosarcoma is most frequently found on the chest and extremities of the body, with approximately 10% to 15% of cases occurring on the head and neck. It initially presents as a painless, flat lesion with the same color as healthy skin or rose-colored. As a result, it can be mistaken for some benign conditions, leading to delayed diagnosis, sometimes even up to a few years3.
The recommended treatment for dermatofibrosarcoma is surgical excision of the lesion with wide margins and primary reconstruction. An excisional biopsy alone is insufficient, as at least 2 cm of free margins or Mohs micrographic surgery is necessary5,6. Currently, Mohs micrographic surgery is considered the gold standard for treatment, regardless of the tumor’s location. Case series analyses and retrospective studies have demonstrated that this technique has lower recurrence rates and preserves more healthy tissue compared to the traditional technique with wide margins3.
This study was accepted by the ethics committee - #24859519.0.0000.5509.
A sixty-year-old man, social drinker, and smoker for 27 years (from 18 to 45) complained of a forehead skin lesion next to the right orbit in the glabella for 6 years. He underwent surgical resection under local anesthesia in 2013 and 2017, with a pathological diagnosis of dermatofibroma spreading to muscle with the recommendation for immunohistochemistry evaluation; however, it had not been performed. A mobile subcutaneous nodular lesion measuring 2.5 cm located on the right glabella was detected (Figure 1). There were no palpable lymph nodes. The ultrasonography showed a highly vascularized nodule measuring 19 x 17 x 16 mm with a hypoechoic halo. The immunohistochemical analysis of both previous biopsies indicated dermatofibrosarcoma protuberans with a proliferation index (Ki67) of 10%. MRI scan revealed an expansive lesion with 25 x 18 x 21 mm in contiguity with the bone, however, without erosion. Surgical resection with intraoperative frozen sections was performed to determine free margins (Figure 2). After two margin augmentations next to the nasogenian groove, they were tumor-free. The reconstruction was performed with a midfrontal flap based on the left trochlear artery (Figures 3 and 4).
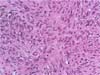
Histopathological examination showed low graded cell spindle tumor with discreet nuclear atypia, low mitotic index, and no necrosis, measuring up to 32 mm in diameter, spreading into dermis, hypodermis, and striated muscle tissue with free margins (Figure 5). Thus, the final diagnosis was dermatofibrosarcoma protuberans. The patient evolved uneventfully.
DISCUSSION
Seldom does dermatofibrosarcoma affect the glabella, resulting in few reported cases in this location. It typically exhibits a slow growth pattern, local aggressive behavior, and negligible metastatic potential, with high rates of local recurrence1.
It commonly presents as a violaceous red-blue plaque with gradual growth over the years, eventually developing multiple nodules within the plaque1. The tumor demonstrates aggressive local invasion and a high recurrence rate after excision, although metastasis is rare2. The diagnosis of dermatofibrosarcoma is often delayed due to its insidious onset and appearance that is relatively nonspecific7, and these lesions can be clinically misdiagnosed as benign entities, as was the case in our patient3.
Dermatofibrosarcoma has been reported to occur on various body surfaces, primarily the trunk, followed by the extremities, and less commonly on the head and neck4. Initially, it superficially adheres to the overlying skin, leading to mobility upon palpation. However, it may infiltrate adipose tissue in later stages and become fixed to deeper structures such as fascia and muscle. Delayed diagnosis and misdiagnosis are common, often due to the absence of symptoms or confusion with benign dermal fibrohistocytic lesions4. The initial lesion was misdiagnosed as dermatofibroma in our case due to the lack of further immunohistochemical evaluation before the patient was referred to our facility. Other possible differential diagnoses in the early stages include lipomas, epidermal cysts, nodular fasciitis, and even keloids. As the lesion becomes more protuberant in the late stages, other soft tissue sarcomas should be considered in the differential diagnosis4.
MRI scan findings are not specific, typically showing a well-delineated tumor that appears isointense or mildly hyperintense on T1-weighted images and hyperintense on T2-weighted images1.
Dermatofibrosarcoma protuberans occupies a central position within a spectrum of tumors known as fibrous histiocytomas. These tumors can exhibit relatively benign behavior, similar to fibrous histiocytomas, or demonstrate more aggressive features akin to malignant histiocytomas. Histologically, dermatofibrosarcoma protuberans is highly cellular and composed of monomorphic, fusiform cells with elongated nuclei that show little or no pleomorphism or hyperchromasia. Mitotic activity is usually moderate. Immunohistochemical evaluation is necessary for accurate diagnosis5. The diagnosis is confirmed by demonstrating strong immunoreactivity for CD 344. This patient underwent two surgeries at another facility, and, most likely, due to the omission of immunohistochemistry evaluation, they were misdiagnosed as dermatofibroma.
Due to its histological characteristics of poor circumscription and frequent extension into the dermis, subcutis, and muscles, resection should include wider and deeper margins than those appreciated clinically or on MRI studies1. The tumor often extends beyond the clinically determined margins during surgical resection3.
Successful treatment requires deep and wide excision and extensive reconstruction involving flaps or grafts5. Micrographic Mohs surgery is considered the optimal treatment for this disease in all anatomical locations3,6. Recommended excision margins are 2 cm or even 3 cm for block excision4,5. The recurrence rate depends on the adequacy of the excision margins4. In our case, intraoperative frozen sections confirmed disease-free margins, subsequently confirmed by the final histopathologic examination using paraffin-embedded tissue.
Dermatofibrosarcoma protuberans is uncommon in the glabella region. Given its proximity to the orbits, its occurrence in this location presents a significant challenge due to the requirement for radical excision and the potential impact on both functional and cosmetic outcomes.
REFERENCES
1. Kiratli H, Koç İ, Özkayar Ö, Kösemehmetog Lu K. Sequential development of dermatofibrosarcoma protuberans in the forehead and eyelid. Can J Ophthalmol. 2017;52(6):e228-30.
2. Simman R, DeFranzo A, Sanger C, Thompson J. Dermatofibrosarcoma protuberans of the face: surgical management. J Craniofac Surg. 2005;16(3):439-43.
3. Benoit A, Aycock J, Milam D, Brown M. Dermatofibrosarcoma Protruberans of the Forehead With Extensive Subclinical Spread. Dermatol Surg. 2016;42(2):261-4.
4. Eguzo K, Camazine B, Milner D. Giant dermatofibrosarcoma protuberans of the face and scalp: a case report. Int J Dermatol. 2014;53(6):767-72.
5. Brazzo BG, Saffra N. Dermatofibrosarcoma protuberans of the brow and eyelid. Ophthalmic Plast Reconstr Surg. 2004;20(4):332-4.
6. St Clair B, Clark A, Rollins B, Jennings TA. Mohs Micrographic Surgery for Dermatofibrosarcoma Protuberans in 15 Patients: The University of Arkansas for Medical Sciences Experience. Cureus. 2022;14(4):e24147.
7. Haas AF, Sykes JM. Multispecialty approach to complex dermatofibrosarcoma protuberans of the forehead. Arch Otolaryngol Head Neck Surg. 1998;124(3):324-7.
1. Universidade Metropolitana de Santos, Santos,
SP, Brazil
2. Universidade de São Paulo, São Paulo, SP,
Brazil
Corresponding author: Mario Augusto Ferrari de Castro Rua Dr. Luis de Faria, 109/94, Santos, SP, Brazil, Zip Code: 11060-481, E-mail: mafc@uol.com.br
Article received: November 27, 2022.
Article accepted: August 20, 2023.
Conflicts of interest: none.












 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter