INTRODUCTION
Classic aesthetic ideals for surgeons and their patients include straight dorsum
and projecting tips1-4. For this, hump reduction has
been the most applied method5-8. However, this procedure is not
the only one possible9,10, in addition to being able to
cause aesthetic and functional impairments, such as internal valve
insufficiencies, inverted V, supratip deformities, and other
complications11,12.
Despite these potential complications, systematic hump removal to correct dorsal
convexity remains the most common practice. What explains this massive
predominance of the reduction procedure? Ineffectiveness of radix and tip
augmentation methods? Since patients usually request reductions, would surgeons
fear perceiving a large nose after augmentation procedures13?
Several authors have investigated the ideas underlying the perception of
reduction after augmentation rhinoplasties14-16. For example,
Constantian14,15 stated that unbalanced and
bottom-heavy noses seem less pleasing and that increasing the radix makes the
nose appear smaller. This perception may be due to the phenomenon of the
illusion of size contrast, in which the volume of a given structure alters the
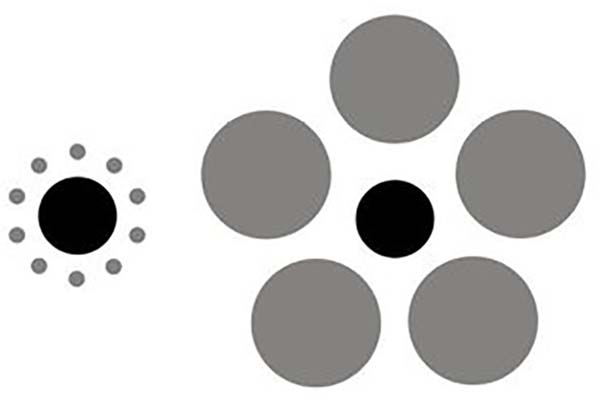
perception of the volume of adjacent structures, as shown in Figure 117-19.
Figure 1 - Tichener circles. The black circle on the left is the same size
as the one on the right but appears larger because of an illusion of
size contrast.
Figure 1 - Tichener circles. The black circle on the left is the same size
as the one on the right but appears larger because of an illusion of
size contrast.
Our group has previously reported an objective reduction in size perception after
radix and tip augmentation20.
However, the study had limitations in sample size, which may have weakened the
conclusions. To our knowledge, no other study has exclusively investigated the
perception of reduction after augmentation procedures.
Although surgical rhinoplasty (SR) has been considered the therapeutic gold
standard for individuals who seek to improve the aesthetic appearance of the
nose21, exclusive
augmentation procedures are often performed by injection of fillers22-25. Early reports of injection molding or non-surgical
rhinoplasty (NSR) date back to the mid-1980s. At that time, treatment options
were limited to bovine collagen and silicone4,26.
Although the use of dermal fillers in NSR remains an off-label application of
hyaluronic acids (HA) and calcium hydroxyapatite (CaHA), its use in the
correction of nasal deformities has been widely reported27, and the procedure has been
popularly called rhinomodelation.
One of the authors has been practicing NSR for the last five years and observed
that, for the primary corrections, the changes are more marked in the profile
than in the frontal view. Thus, in these cases of primary correction, it started
to indicate the NSR only for patients whose main complaint is in the profile
image. Since this procedure has been incorporated into her practice, there have
been several opportunities to notice that noses look smaller.
OBJECTIVE
Given the anecdotal evidence of size reduction perceived by patients after NSR,
we aimed to assess two questions. Does the perception of reduction occur in the
NSR? Is the perception of reduction important in the NSR?
METHOD
The study retrospectively evaluated the perceived size and quality of nose
corrections after non-surgical augmentation procedures in a consecutive case
series. Primary patients who underwent midline NSR with the main author from
February 2015 to October 2018 in Fortaleza - CE were included in the study.
Patients who had undergone surgical or non-surgical nose procedures before the
study were excluded. Any nasal filling performed outside the midline was not
included. The study was conducted following the principles of the Declaration
of
Helsinki, and all patients provided informed consent. The Federal University
of
Ceará Research Ethics Committee approved the study under protocol number
22928719.7.0000.5054.
Image documentation
As the profile view was considered more representative of changes in the
nose, only profile images were used in the study. The profile view on the
right side was chosen by lot. The images were captured digitally28,29, with a Canon EOS 70D dSLR camera, 20 MPixels
(Canon Inc., Tokyo, Japan), and a 135mm lens placed 190cm away from the
object. Images were stored in JPEG format. Patients were oriented so that
they naturally looked straight ahead30,31.
After photographic documentation, each patient received advice on the
possible risks and benefits of the procedure. Only patients who indicated
that they wanted to improve their profile view were accepted for treatment.
Patients knew their information and photos would be used in the study.
NSR protocol
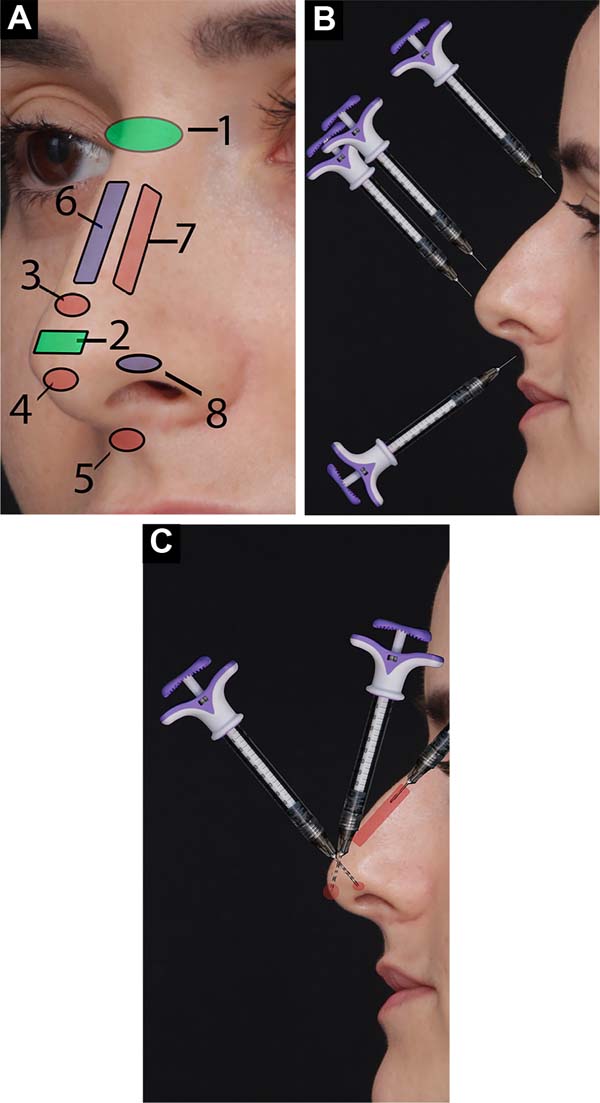
The injection technique followed that described by Wu32-34. Areas to be injected include the radix
(nasofrontal angle, just above the periosteum), tip (subcutaneous plane over
the domus), supratip (juxtaperichondrial), infratip (subcutaneous), nasal
spine (nasolabial fold, subcutaneous), dorsum (anterior aspect of the nasal
dorsum in the middle third, juxtaperichondrial). The areas are shown in
Figure 2A. After careful
aspiration, the injections were made in small boluses (between 0.05cc and
0.1cc) to avoid intravascular injection. A needle was introduced
perpendicular to the skin to increase the nasal spine, radix, tip, supratip,
and infratip (Figure 2B). To fill the
dorsum, a microcannula was used, placed parallel to the skin, deeply
(juxtaperichondrial), as in Figure 2C.
The Vycross Allergan™ line (Allergan Inc., Irvine, CA, USA).
Figure 2 - A: Application areas. 1 - root; 2 - tip; 3 -
supratip; 4 - infratip; 5 - nasal spine, 6 - dorsum;
B: Application technique. The needle is placed
perpendicular to the skin’s surface in these areas;
C: Cannula lies parallel to the skin in the
back area.
Figure 2 - A: Application areas. 1 - root; 2 - tip; 3 -
supratip; 4 - infratip; 5 - nasal spine, 6 - dorsum;
B: Application technique. The needle is placed
perpendicular to the skin’s surface in these areas;
C: Cannula lies parallel to the skin in the
back area.
Photographic documentation was performed immediately after the procedure and
at a 6-month follow-up. The physician and staff nurse were available for
extra consultations during the follow-up period. During these visits,
photographs were taken, and further, HA injections were performed in areas
where the injected volume had decreased when necessary. As the study’s
objective was to evaluate the perception of the shape/size relationship
rather than the longevity of the procedure, only the images obtained after
the first procedure were used.
Image preparation and evaluation
Adobe Photoshop™ software was used to crop the images at the following
reference points: superiorly - at the top of the eyebrow; left side - at the
most posterior point of the iris; inferiorly - between the upper and lower
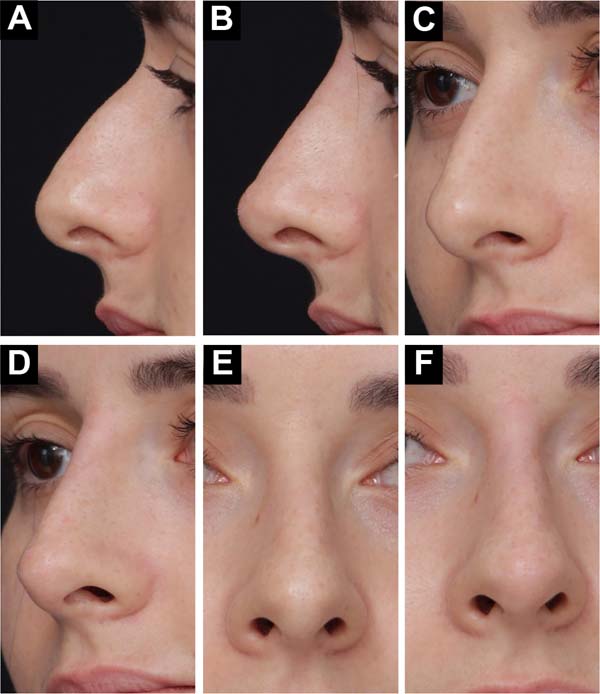
lip, and; right side - enough to see the background of the image (Figure 3).
Figure 3 - A: Images from before and immediately after NSR,
with 0.3cc of hyaluronic acid at the root and 0.2cc at the tip.
A, C, and E before the procedure and B, D, and F after NSR. NSR
- non-surgical rhinoplasty; B: Images from before
and immediately after NSR, with 0.3cc of hyaluronic acid at the
root and 0.2cc at the tip. A, C, and E before the procedure and
B, D, and F after NSR. NSR - non-surgical rhinoplasty;
C: Images from before and immediately after
NSR, with 0.3cc of hyaluronic acid at the root and 0.2cc at the
tip. A, C, and E before the procedure and B, D, and F after NSR.
NSR - non-surgical rhinoplasty; D: Images from
before and immediately after NSR, with 0.3cc of hyaluronic acid
at the root and 0.2cc at the tip. A, C, and E before the
procedure and B, D, and F after NSR. NSR - non-surgical
rhinoplasty; E: Images from before and immediately
after NSR, with 0.3cc of hyaluronic acid at the root and 0.2cc
at the tip. A, C, and E before the procedure and B, D, and F
after NSR. NSR - non-surgical rhinoplasty; F:
Images from before and immediately after NSR, with 0.3cc of
hyaluronic acid at the root and 0.2cc at the tip. A, C, and E
before the procedure and B, D, and F after NSR. NSR -
non-surgical rhinoplasty.
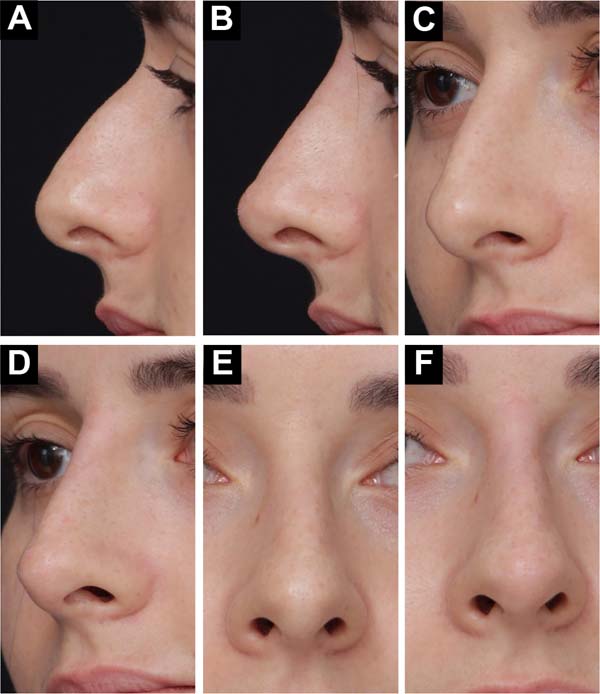

Figure 3 - A: Images from before and immediately after NSR,
with 0.3cc of hyaluronic acid at the root and 0.2cc at the tip.
A, C, and E before the procedure and B, D, and F after NSR. NSR
- non-surgical rhinoplasty; B: Images from before
and immediately after NSR, with 0.3cc of hyaluronic acid at the
root and 0.2cc at the tip. A, C, and E before the procedure and
B, D, and F after NSR. NSR - non-surgical rhinoplasty;
C: Images from before and immediately after
NSR, with 0.3cc of hyaluronic acid at the root and 0.2cc at the
tip. A, C, and E before the procedure and B, D, and F after NSR.
NSR - non-surgical rhinoplasty; D: Images from
before and immediately after NSR, with 0.3cc of hyaluronic acid
at the root and 0.2cc at the tip. A, C, and E before the
procedure and B, D, and F after NSR. NSR - non-surgical
rhinoplasty; E: Images from before and immediately
after NSR, with 0.3cc of hyaluronic acid at the root and 0.2cc
at the tip. A, C, and E before the procedure and B, D, and F
after NSR. NSR - non-surgical rhinoplasty; F:
Images from before and immediately after NSR, with 0.3cc of
hyaluronic acid at the root and 0.2cc at the tip. A, C, and E
before the procedure and B, D, and F after NSR. NSR -
non-surgical rhinoplasty.
The pre-images were placed on the left side, and the post-images on the right
side of the screen, with the same size and position. Below each pair of
images was a quiz with two questions:
1. Compared to the left image, the right image’s nose is:
1 = much smaller to 10 = much larger. Response:
2. Do you consider this fix:
1 = very bad to 10 = very good.
Response:
All study cases were prepared as described above and entered into a Google
form (Google Inc, California, USA). A link was created with the form ready
with all the images. The link was sent to the observers through WhatsApp
(WhatsApp LLC, Meta, Inc), along with a thank you message for participating
in the survey. The evaluation form used in the study can be found at
https://forms.gle/xPJmkxM7NFcX2iVD6. Another form with the
same content is available in two parts: https://forms.gle/MK4tMCauqUo4zhG2A and https://forms.gle/2aBz8yYrHwiB5x297. The reader is invited
to answer the questions.
The evaluators were divided into 3 groups: NSR, SR, and MA. The NSR group
consisted of all patients who underwent NSR, in the same service, in the
last 3 months, totaling 21. The SR group consisted of all patients who
underwent SR in the last 3 months at the same service, totaling 16. The MA
group consisted of all patients who underwent breast augmentation in the
last 3 months in the same service, totaling 18. All 55 evaluators were
unaware of the study objectives. Responses were exported to a Microsoft
Excel® spreadsheet (Microsoft Corporation, Redmont,
Washington, USA).
RESULTS
One hundred eighty-one consecutive patients underwent NSR between February 2015
and October 2018. Of these, 64 were not included because they had undergone a
previous surgical or non-surgical procedure on the nose. Two cases were excluded
because post-procedure photographs were not taken.
Therefore, 115 patients were included in the study. They consisted of 14 men
(12.06%) and 101 women (87.93%) between 15 and 65 years of age (mean age=35.75
years, standard deviation - SD=10.18). The follow-up period ranged from 174 to
1502 days (mean=550.29 days; SD=227.91).
Mild pain and redness for up to 3 days after the procedure were not considered
complications. Intermittent redness was also not considered a complication when
exposed to low or high temperatures up to 8 weeks after the procedure. One
patient (0.85%) was dissatisfied with the result and requested a reversal. She
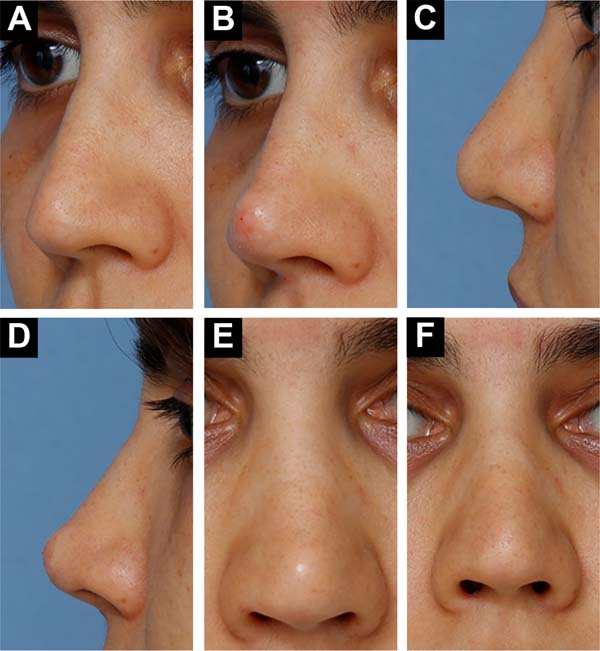
described her nose as having “a ball at the tip” (Figure 4). Hyaluronidase was injected 4 days later, with
satisfactory results.
Figure 4 - A: Images before and after injection in the tip and
spine areas. This patient was dissatisfied and requested the
withdrawal of injectable hyaluronidase hyaluronic acid. A, C, and E
- before. B, D, and F - after NSR. NSR - non-surgical rhinoplasty;
B: Images before and after injection in the tip and
spine areas. This patient was dissatisfied and requested the
withdrawal of injectable hyaluronidase hyaluronic acid. A, C, and E
- before. B, D, and F - after NSR.NSR - non-surgical rhinoplasty;
C: Images before and after injection in the tip and
spine areas. This patient was dissatisfied and requested the
withdrawal of injectable hyaluronidase hyaluronic acid. A, C, and E
- before. B, D, and F - after NSR. NSR - non-surgical rhinoplasty;
D: Images before and after injection in the tip and
spine areas. This patient was dissatisfied and requested the
withdrawal of injectable hyaluronidase hyaluronic acid. A, C, and E
- before. B, D, and F - after NSR.NSR - non-surgical rhinoplasty;
E: Images before and after injection in the tip and
spine areas. This patient was dissatisfied and requested the
withdrawal of injectable hyaluronidase hyaluronic acid. A, C, and E
- before. B, D, and F - after NSR. NSR - non-surgical rhinoplasty;
F: Images before and after injection in the tip and
spine areas. This patient was dissatisfied and requested the
withdrawal of injectable hyaluronidase hyaluronic acid. A, C, and E
- before. B, D, and F - after NSR NSR - non-surgical
rhinoplasty.
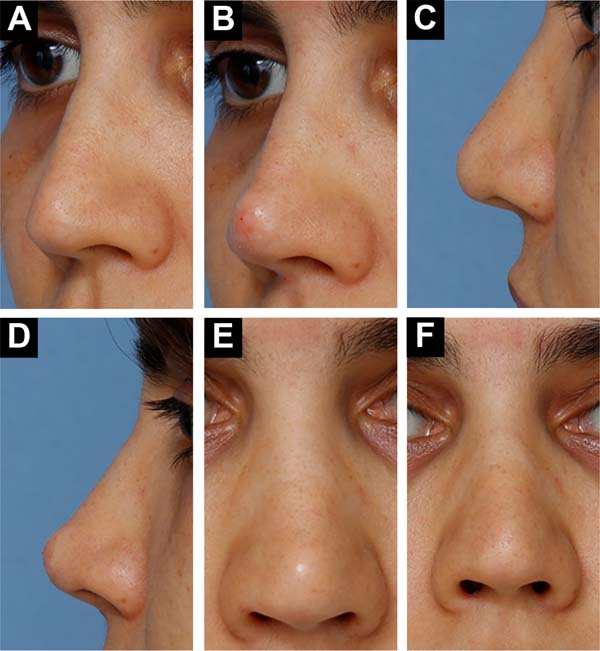

Figure 4 - A: Images before and after injection in the tip and
spine areas. This patient was dissatisfied and requested the
withdrawal of injectable hyaluronidase hyaluronic acid. A, C, and E
- before. B, D, and F - after NSR. NSR - non-surgical rhinoplasty;
B: Images before and after injection in the tip and
spine areas. This patient was dissatisfied and requested the
withdrawal of injectable hyaluronidase hyaluronic acid. A, C, and E
- before. B, D, and F - after NSR.NSR - non-surgical rhinoplasty;
C: Images before and after injection in the tip and
spine areas. This patient was dissatisfied and requested the
withdrawal of injectable hyaluronidase hyaluronic acid. A, C, and E
- before. B, D, and F - after NSR. NSR - non-surgical rhinoplasty;
D: Images before and after injection in the tip and
spine areas. This patient was dissatisfied and requested the
withdrawal of injectable hyaluronidase hyaluronic acid. A, C, and E
- before. B, D, and F - after NSR.NSR - non-surgical rhinoplasty;
E: Images before and after injection in the tip and
spine areas. This patient was dissatisfied and requested the
withdrawal of injectable hyaluronidase hyaluronic acid. A, C, and E
- before. B, D, and F - after NSR. NSR - non-surgical rhinoplasty;
F: Images before and after injection in the tip and
spine areas. This patient was dissatisfied and requested the
withdrawal of injectable hyaluronidase hyaluronic acid. A, C, and E
- before. B, D, and F - after NSR NSR - non-surgical
rhinoplasty.
Twelve of the 55 evaluators who received the questionnaire answered it (three
from the SR group, five from the NSR group, and four from the MA group). Each
rater’s average size perception score was 4.71 (range = 3.08 to 7.00, SD =
0.83). A score of 5.5 was considered neutral. Twenty cases (17%) were perceived
as an increase in size, while 92 (79%) were perceived as a reduction in
size.
The mean score for correction quality was 8.29 (range=5.83 to 9.58, SD=0.76).
Cases that were perceived to be enlarged (size perception score -SPS>5.5) had
a mean quality correction score (QCS) of 7.71 (SD=0.7), which was lower than
the
series mean, from 8.29. Cases perceived as reduced (SPS <5.5) had a mean QSC
of 8.41 (SD=0.72), higher than the series mean. The 115 cases were also divided
into four groups according to the perceived degree of increase/decrease, as
shown in Table 1.
Table 1 - Distribution of correction quality scores according to size
perception scores.
| Group |
EMPT* |
N** |
AQCS*** |
SD |
| A |
<4 |
19 |
8.68 |
0.88 |
| B |
<5 |
77 |
8.55 |
0.7 |
| C |
<6 |
107 |
8.32 |
0.68 |
| D |
>6 |
8 |
7.82 |
0.68 |
Table 1 - Distribution of correction quality scores according to size
perception scores.
DISCUSSION
Although several augmentation procedures show improvement in contour and
respiratory function35, the
overwhelming predominance of reduction procedures is still observed7. The surgeon’s reluctance to
augmentation procedures can have several causes, such as fear of infection,
displacement, visibility, and distortion of grafts35. In addition, patients usually ask to reduce
the size of their nose, not to enlarge it36.
In a series by Foda8, there was
no increase in the dorsum in any of 500 consecutive cases, despite the hump of
the dorsum being the most common diagnosis. Was there no one with a low radix
in
those 500 cases?
Becker & Pastorek7 raised
the radix in 5% to 10% of their cases, while Constantian9,37 found that 38% of their 50 primary cases and 93% of
their 150 secondary cases had a low radix or dorsum. Could these authors have
a
study population so different from Foda8, or is there really a reluctance to perform augmentation
rhinoplasty?
Constantian9,14,15,37, who has written extensively
on balance concepts, claims that raising the radix of bottom-heavy noses makes
them look smaller and prettier. This concept can be very reassuring for surgeons
who want to perform augmentation procedures but are concerned about patient
reactions.
Unfortunately, the current literature does not provide definitive objective
evidence to support this idea. The objective investigation of size perception
was carried out in this study to help fill this gap since, as far as we know,
only one published article used this approach20.
NSR has proven to be a good testing ground for augmentation rhinoplasty for
several reasons. First, there are no concomitant reduction maneuvers. Thus, we
guarantee that the reductions do not cause the perception of reduction. Second,
it offers immediate results. Third, it is a common procedure that offers wide
sampling possibilities. Even so, despite being considered high risk, there is
little information about NSR in the medical literature regarding results,
technique, and safety. This indicates the urgent need for more studies like the
current one.
Although the photographs differ from the real objects, the possible distortions
inherent to the method are equally present both in the preand postoperative
images, reducing the chance of bias. Digital photography can also be considered
valid for this purpose and greatly facilitates everyday life. Therefore, it was
chosen as a documentation method29,38,39.
We created one because there is no specific methodology to measure the perception
of nose size. For this, we set up a 10-point Likert-type scale40. This new tool was based on
the Rhinoplasty Outcome Evaluation questionnaire and a previously published size
perception scale of our own20.
The process was also applied to construct the correction quality scale. Although
there are some self-assessment tools for quality of life after rhinoplasty,
there is no tool to assess the quality of the correction by third parties. As
we
were trying to assess the influence of shape on the perception of size and
correction quality, we believed that external observers would have less bias
than patients themselves. Thus, an ordinal numeric ruler was constructed (using
a 10-point system from “very poor” to “very good”) to assess correction
quality.
Our results showed a mean size perception score (EMPT) of 4.7, which was lower
than the neutral point of 5.5. Seventy-nine percent of cases scored below 5.5.
This indicates that observers tended to perceive size reduction after
augmentation procedures. This is in line with observations by
Constantian9,14,15,37, when he
suggested that augmentation rhinoplasty may cause a perception of reduction.
This is also in line with our results from a previous study20. However, 17% of cases were
perceived as enlarged. While this does not suggest a poor correction, the
augmentation is not what patients expect. Therefore, these results indicate that
further investigations should be carried out to refine the criteria for
indicating the procedure.
According to our results, the more perceived reduction, the higher the correction
quality score. This may suggest that there is an indirect correlation between
these two parameters. Therefore, perception seems to be important in
rhinoplasty.
We think non-surgical approaches to correct nose deformities have many
limitations and do not replace the surgical approach. NSR can slightly improve
appearance in the front view but has almost no effect on wing flair and very
little effect on rounded ends. Therefore, we do not indicate the procedure to
treat primary patients whose main complaints are focused on frontal vision.
Secondary patients who need correction of small irregularities can benefit from
NSR, even if the complaint is in the frontal view.
NSR also has limitations for side view corrections. Patients with very low radix
often lose part of the treatment effect within a few days. Attempts to correct
it with more filler injection may enlarge the area, making the front-view image
worse. Patients with a dorsal hump and a radix higher than the supratarsal
crease of the upper eyelid have a Roman nose appearance, which may be unpleasant
for some. NSR results on very long noses are often disappointing. It is also
difficult to achieve good shape in thick-skinned patients, especially in thicker
areas such as the tip.
Blindness and skin infarcts have been reported as possible serious complications
related to NSR or injection rhinoplasty23. These complications were first reported with HA in
200241. Although we
did not experience such complications, our study did not have a large enough
sample to attest to the safety of the NSR.
Tansatit et al.42 studied the
microscopic soft tissue from the midline from root to tip in 45 cadavers and
determined that it was a relatively safe area, with no arteries large enough
for
cannula embolization. However, compared to other areas, they identified a
high-risk area in the subcutaneous plane of the overtip (supratip). The area
of
the nasal spine has not been studied, but it is known to contain the labial
artery and its columellar branch43.
To make the procedure safer, we recommend using cannulas whenever possible.
However, when using needles, prefer the juxtaperichondrial or periosteal plane;
always aspirate before injecting and do so only in the midline of the nose,
avoiding the overlap region. NSR can be a powerful procedure in reaching people
who are hesitant to undergo surgery, acting as a bridge to surgical solutions
or
an end in itself.
CONCLUSION
Enlargement by the NSR may cause a perception of reduced nose size in the profile
view. The degree of perceived reduction may be indirectly related to the degree
of quality of the correction in the profile view.
1. Clínica Médica Eduardo Furlani, Fortaleza, CE,
Brazil
2. Universidade Federal do Ceará, Faculdade de
Medicina, Fortaleza, CE, Brazil
Corresponding author: Eduardo Antonio Torres
Furlani Rua Tibúrcio Cavalcante, 1750, Aldeota, Fortaleza, CE,
Brazil., CEP: 60.125-045, E-mail: eduardofurlani@hotmail.com