INTRODUCTION
Mastectomy is a procedure that consists of total or partial removal of breast
tissue, varying according to the extent of resection of additional tissues
(glandular tissue, overlying skin, pectoral muscles, and regional lymph nodes).
Its main indications are for treating breast cancer and for prophylaxis in
patients at high risk of developing breast cancer (such as patients with
mutations in the BRCA1 and BRCA2 genes)1. This surgery constitutes a possible source of
psychological stress that hinders the psychosocial functioning of the patient
who undergoes it, insofar as he will have to deal with tension and body
dysmorphism, in addition to several other related issues2.
Therefore, in recent years, the search for plastic surgeries for post-mastectomy
breast reconstruction has been increasing, mainly due to the benefits generated
by that procedure, such as the tendency for patients to value quality of life
more and to feel more attractive3.
However, performing anesthetic-surgical procedures in patients considered at high
perioperative risk can be a challenge, and due to the concern of
anesthesiologists and surgeons regarding the safety of the procedure, the
current trend is the implementation of protocols that revolutionize
perioperative care, improving the in-hospital management of these patients and
improving outcomes4.
Among the protocols that aim to improve the recovery of patients after surgery,
the systematic review of meta-analyses endorsed by the Enhanced Recovery After
Surgery Society (ERAS) stands out. This protocol consists of a consensus of
recommendations based on scientific evidence, which aim to promote optimal
perioperative care and generate an improved recovery, even after breast
reconstruction plastic surgery5.
Through this set of recommendations, it is possible to ensure a safer and more
efficient approach to pre-, intra-, and postoperative care. The implementation
of the protocol can bring significant benefits, such as patient engagement,
mitigation of the physiological stress associated with the surgery, reduction
of
avoidable postoperative complications (reduction of morbidity and mortality,
faster recovery, reduction of hospital stay), resulting in a reduction in
hospital costs and decrease in hospital readmission rates within 30
days6.
OBJECTIVE
The present study sought to carry out an analysis of the recommendations of the
ERAS protocol in breast reconstruction plastic surgery used in two hospitals
in
the south of the country, generating strategies for the implementation of a
protocol that aligns practice with scientific evidence, promotes institutional
leadership and encourages work in a team, engaging all parties involved in
patient care, in addition to the other previously mentioned benefits7.
METHOD
Cross-sectional study using a database of physical and electronic medical
records. The University of Southern Santa Catarina’s Research Ethics Committee
approved the study under opinion 5,570,697, CAAE 59026222.8.0000.5369, on August
9, 2022.
Female patients aged 18 years or older who underwent plastic surgery for
post-mastectomy breast reconstruction in two general hospitals in southern
Brazil between 2018 and 2021 were evaluated. The sample was of the census
type.
Variables related to the patient’s sociodemographic characteristics were
collected from the medical records (gender, age, presence of social habits,
comorbidities, BMI (Body Mass Index), and the type of procedure to be
performed); presence of preoperative advice and guidance, especially regarding
smoking cessation, pre-surgery weight loss and alcohol abstinence; performance
of pre-surgical computed tomography angiography; preoperative fasting time for
clear liquids and solid foods determined by the anesthesiologist; performance
of
preoperative conditioning with carbohydrates.
Also verified prophylaxis for venous thromboembolism and methods; skin
preparation and which substance used; administration of antibiotics before
surgery and time of its pre-surgical administration; medications used for
postoperative nausea and vomiting (PONV); pre and intraoperative multimodal
analgesia; standard anesthetic protocol, containing the type of intraoperative
anesthesia used; prevention of intraoperative hypothermia; intraoperatively
administered fluids; prescription of postoperative analgesics; time to start
oral fluid intake and to walk after surgery; time to hospital discharge.
Additionally, we analyzed immediate complications and readmissions.
Categorical variables were presented as absolute frequencies and percentages, and
continuous variables as mean and standard deviation (SD). The follow-up rate
per
patient was calculated by simple arithmetic mean. Spearman’s correlation
coefficient was used to assess the statistical dependence between two variables.
The adopted statistical significance level was 5%
(p<0.05).
RESULTS
During the study period, 99 breast reconstruction procedures were performed, 100%
of which were female patients. The median age of patients was 56 years
(SD=15.75), ranging from 19 to 81. Mean BMI was 26.97 kg/m2
(SD=4.22). Data related to the study and procedure participants are presented
in
Table 1.
Table 1 - Characteristics of patients undergoing breast reconstruction surgery
(n=99).
| Variable |
n |
% |
| Age |
|
|
| 19-30 years |
15 |
15.2 |
| 31-50 years |
34 |
34.3 |
| > 50
years
|
50 |
50.5 |
| Social habits / Comorbidities
(pre-admission) |
| Smoking |
8 |
8.1 |
| Obesity |
26 |
26.3 |
| Alcoholism |
4 |
4.0 |
| BMI |
| < 18.5 |
1 |
1.0 |
| 18.6 - 24.9 |
34 |
34.4 |
| 25.0 - 29.9 |
43 |
43.4 |
| 30.0 - 34.9 |
16 |
16.1 |
| 35.5 - 39.9 |
6 |
5.1 |
| > 40 |
- |
0.0 |
| Procedure to be
performed |
| Prosthesis And/Or Expander |
35 |
35.4 |
| Post-Quadrantectomy Partial Reconstruction |
45 |
45.5 |
| Muscular or myocutaneous flap |
13 |
13.1 |
| Regional Skin Flaps |
6 |
6.1 |
Table 1 - Characteristics of patients undergoing breast reconstruction surgery
(n=99).
Of the patients who participated in the study, 100% underwent pre-anesthetic
evaluation, receiving information, education, and detailed preoperative
counseling, as seen in Figure 1. The data
presented are followed by their Level of Evidence (LE).
Figure 1 - Adherence to the indications strongly recommended in the ERAS
protocol for breast reconstruction plastic surgery. ERAS: Enhanced
Recovery After Surgery.
Figure 1 - Adherence to the indications strongly recommended in the ERAS
protocol for breast reconstruction plastic surgery. ERAS: Enhanced
Recovery After Surgery.
The optimization of pre-admission - which consists of carrying out, before
surgery, one month of abstinence from tobacco for smokers (LE = moderate); one
month of abstinence from alcohol for alcoholics (LE = moderate); and weight
reduction in obese patients to reach a BMI ≤ 30kg/m2 (LE = high) -
was performed by 52.5% of patients. Flap planning, with preoperative mapping
of
perforating vessels with angiotomography (LE = moderate), was performed by only
1.0% of patients (n=1).
Minimized perioperative fasting was indicated for 84.8% of patients, who were
allowed to drink clear liquids up to two hours before surgery (LE = moderate).
None of the patients were given preoperative drinks based on maltodextrin in
the
two hours before the surgery (LE = low).
During the preand intraoperative period, multimodal analgesia to alleviate pain
was performed in 100% of patients (LE = moderate). The standard anesthetic
protocol with total intravenous anesthesia (TIVA) was not performed on any
patient; in contrast, all patients received combined general anesthesia.
Preoperative and intraoperative measures to avoid hypothermia, as well as
perioperative intravenous fluid management, in an attempt to avoid excessive
or
insufficient fluid resuscitation (LE = moderate), were indicated in only 2.0%
of
the medical records (n=2).
Postoperatively, 22.2% of patients were encouraged to take liquids and food
orally as soon as possible, preferably within 24 hours after surgery (LE =
moderate) (n=22). Frequent monitoring of the flap in the first 72 hours after
the operation was indicated by the nursing team in only 2% of the medical
records (n=2).
No information was found in the medical records about early mobilization in the
first 24 hours after surgery (LE = moderate) and post-discharge home support
and
physiotherapy (LE = moderate).
The average rate of compliance with the ERAS protocol per participant was 50.7%.
Regarding the perioperative procedures performed, as shown in Table 2, surgical management was performed
in 99% of patients, all receiving conventional sutures for incisional closure
(LE = high) (n=98).
Table 2 - Procedures performed in patients undergoing breast reconstruction
surgery (n=99).
|
n |
% |
| Wound
management |
|
|
| Conventional
suture
|
98 |
99.9 |
| NPWT |
- |
0.0 |
| Prophylaxis of venous
thromboembolism in high-risk patients |
| Mechanical prophylaxis |
56 |
56.6 |
| Pharmacological prophylaxis with LMWH |
24 |
24.2 |
| Pharmacological prophylaxis with UFH |
23 |
23.1 |
| Skin
preparation |
|
|
|
Chlorhexidine
|
90 |
90.9 |
| Antibiotic given
within 1 hour before incision
|
97 |
98.0 |
| Alcoholism |
4 |
4.0 |
| Medications for VONV |
|
|
| Dexamethasone |
65 |
65.7 |
| Ondansetron |
67 |
67.7 |
| Metoclopramide |
36 |
36.7 |
| Other |
11 |
11.1 |
| Pre and intraoperative analgesia and
sedation |
| Opioid |
99 |
100.0 |
| Muscle
relaxant
|
99 |
100.0 |
|
Benzodiazepine
|
99 |
100.0 |
| Standard anesthetic protocol |
|
|
| TIVA |
- |
0.0 |
| Balanced general anesthesia |
99 |
100.0 |
| Postoperative analgesia |
|
|
| Dipyrone |
44 |
44.4 |
|
Acetaminophen
|
60 |
60.6 |
| INES |
68 |
68.7 |
|
Corticosteroid
|
36 |
36.4 |
| Weak
opioida |
21 |
21.2 |
| Strong
opioidb |
29 |
29.3 |
| Other |
8 |
8.1 |
Table 2 - Procedures performed in patients undergoing breast reconstruction
surgery (n=99).
The risk of venous thromboembolism was assessed in 80.8% of patients (n=80), with
56.6% receiving mechanical methods for prophylaxis (n=56); 24.2% received low
molecular weight heparin (LMWH) (n=24); and 23.1% received unfractionated
heparin (UFH) (n=23) until ambulation or discharge (LE = moderate).
Antimicrobial prophylaxis was performed in 99.0% of patients (LE = moderate)
(n=98). Of these, 90.9% had their skin prepped with chlorhexidine (n=90), and
98.0% received intravenous antibiotics covering common skin organisms within
one
hour of incision (n=97).
Preand intraoperative medications to attenuate postoperative nausea and vomiting
were administered to 85.9% of patients (LE = moderate) (n=85). Of the drugs
used: dexamethasone 65.7% (n=65); ondansetron 67.7% (n=67); metoclopramide 36.7%
(n=36); and another 11.1% (n=11). For pain control, 100% of patients received
multimodal drug regimens (LE = high).
Of these drugs: dipyrone 44.4% (n=44); acetaminophen 60.6% (n=60); non-steroidal
anti-inflammatory drugs (NSAIDs) 68.7% (n=68); corticosteroid 36.4 (n=36); weak
opioid (codeine, tramadol, dextropropoxyphene, hydrocodone) 21.2% (n=21); strong
opioid (fentanyl, methadone, hydromorphone, morphine, oxycodone) 29.3% (n=29);
another 8.1% (n=8).
According to the results shown in Table 3,
which represents the postoperative outcomes, all patients were discharged.
However, there was a prevalence of 29.3% of cases of complications. The three
main causes of complications were pain (15.2%), nausea and vomiting (11.1%),
and
constipation (3.0%). In addition, 20.2% of patients needed to be readmitted.
Table 3 - Outcomes of patients undergoing breast reconstruction
surgery.
|
n |
% |
| Discharge |
99 |
100.0 |
| Complication |
29 |
29.3 |
| Pain |
15 |
15.2 |
| Nausea and vomiting |
11 |
11.1 |
| Cold |
3 |
3.0 |
| Readmission |
20 |
20.2 |
Table 3 - Outcomes of patients undergoing breast reconstruction
surgery.
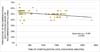
When analyzing the mean length of stay (11 hours and 52 minutes) and its
relationship with the number of indications with a strong degree of
recommendation achieved, a moderate negative correlation was observed between
the variables. Figure 2 shows this
statistical dependence as a decreasing monotonic trend; that is, as the number
of indications with a strong degree of recommendation achieved increases, the
length of stay decreases until the patient is discharged (Spearman ρ = -0.397)
(p<0.001).
Figure 2 - Relationship between the number of ERAS protocol recommendations
followed and length of stay until discharge.ERAS: Enhanced Recovery
After Surgery.
Figure 2 - Relationship between the number of ERAS protocol recommendations
followed and length of stay until discharge.ERAS: Enhanced Recovery
After Surgery.
DISCUSSION
Each element of the ERAS protocol is designed to decrease the physiological
stress of the surgical intervention, and there is evidence in the literature
that each recommendation is associated with several clinical benefits, including
a shorter hospital stay. However, low adherence or implementing only a few
recommendations is insufficient to achieve all the expected benefits. Compliance
with most items can be crucial to achieving a desired clinical outcome,
producing greater clinical benefits than their parts8.
The present study’s results align with a pilot study of ERAS in the National
Surgical Quality Improvement Program (PNMQC) of the American College of Surgeons
(ACS), which included 16 hospitals that implemented the protocol in more than
1,500 patients. The study found that the mean length of stay increases as
adherence to the ERAS protocol decreases (p<0.001),
reinforcing the importance of complete adherence to recommendations to achieve
the expected clinical benefits8,9.
This information is important, as most patients with breast cancer have a
time-dependent disease, which means that the recovery time and the effectiveness
of the treatment directly affect the post-mastectomy result; that is, the faster
and more effective the recovery, the greater the chance of cure or control of
the disease. Furthermore, mastectomy is often followed by additional therapies
such as chemotherapy and radiotherapy, which can also have significant adverse
effects. Therefore, recovery optimization can help to minimize the total
treatment time and reduce the risk of related complications10.
It is known that not all ERAS protocol steps apply to each patient. However,
collecting data from medical records about their adherence at an individual
level allows providers to identify which protocol components are problematic
and
target their interventions to improve compliance9.
In this order of ideas, we have, for example, that, during the preoperative
evaluation, smoking cessation should be oriented to all patients; however, only
half reached this recommendation. Studies point out that the persistence of
smoking in the perioperative period results in higher rates of postoperative
complications, mainly infection of the incisional wound11. Spontaneous smoking cessation
is related to several biopsychosocial factors. Therefore, to achieve this
recommendation, it is necessary to implement a multidisciplinary
follow-up12.
Preoperative optimization using carbohydrates such as maltodextrin prevents the
catabolic state induced by the surgical stress response, reduces postoperative
nitrogen and protein losses, helps maintain lean body mass and muscle strength,
and decreases insulin resistance. Added to this, it reduces preoperative thirst,
hunger, and anxiety13. This
recommendation, however, still qualifies as a low level of evidence, and its
benefits vary according to the type of surgery and the patient evaluated, which
would explain the low adherence in the target sites of the present
study14.
In large centers, physiotherapy is still performed in the post-anesthetic
recovery room, even with the patient on mechanical ventilation15. This study, however,
demonstrated that there was no early mobilization in the patients studied. As
a
result of the various barriers that are imposed on this recommendation, its
implementation requires the efforts and engagement of a multidisciplinary
team.
Furthermore, it was noted that the analgesia was administered intravenously,
predominantly, which goes against the current literature, which recommends
multimodal perioperative analgesia, using combinations of analgesic medications
that act in different sites and routes, in an additive or synergistic, to obtain
pain relief with minimal or non-existent consumption of opioids16.
A standard anesthetic protocol with TIVA is intended to minimize anesthetic side
effects and facilitate rapid awakening and recovery after surgery. However,
compared to balanced techniques, the superiority in choosing this anesthetic
technique was seen only in some specific situations. Among the main obstacles
to
its adherence are the high cost, the low availability of equipment, and the need
to train professionals who are possibly already used to other techniques,
according to the respective anesthesiology service17.
It is known that hypothermia occurs in 70% of patients undergoing operations
lasting two or more hours, increasing intraoperative blood loss. It is usually
preventable through active warming using a blanket and thermal mattress. The
use
of dynamic monitors and fluid-responsiveness measurements also guide fluid
utilization. However, in small to moderate surgeries with a non-prolonged
duration and low risk of bleeding, the cost and availability of these
instruments often constitute an obstacle to their use18.
Adherence to the ERAS protocol can be deficient due to several reasons. One of
the main barriers is the lack of knowledge of the protocol by health
professionals who are part of the surgical team. The difficulty of raising
awareness about the need to change habitual behaviors can be hard in this
process. Another barrier may be the lack of resources or adequate infrastructure
to implement the protocol, especially in smaller hospitals or with fewer
available resources19.
To achieve better clinical outcomes, these barriers must be addressed and
overcome. Education of surgical teams and training for the ERAS protocol can
be
essential to improve adherence and understanding of the corresponding benefits.
It is also important to provide adequate support and resources for implementing
the protocol in hospitals, including the availability of a multidisciplinary
team to support its implementation. Continuous monitoring and evaluation of
results are essential to ensure that the protocol is being properly implemented
and to identify opportunities for improvement20.
Furthermore, the ERAS protocol offers a unique opportunity to leverage existing
resources by instituting a standardized approach to anesthesia and
surgery-related challenges. This allows growing hospitals to increase their bed
capacity and, consequently, the surgical volume, generating a potential increase
in gross revenue due to the savings in hospitalization days21.
CONCLUSION
The average rate of compliance with the ERAS protocol per participant was 50.73%.
The mean length of stay was 11 hours and 52 minutes. The number of indications
with a strong degree of recommendation achieved showed the ability to reduce
the
time, in minutes, from hospitalization to discharge (Spearman’s ρ = -0.397)
(p<0.001). This demonstrates the need for greater
protocol adherence to reduce the length of hospital stay.
Study limitations
It is important to consider the inherent limitations of ecological studies
that use medical records as a database. One of the main concerns is the
quality of the data, which can vary widely between health professionals
responsible for completing the records, affecting the accuracy of the
results obtained and the validity of the conclusions reached. Another
important aspect to be considered is data availability. Medical records do
not always contain all the information relevant to a study, which may limit
researchers’ ability to explore certain questions. In addition, charts are
generally collected from a specific sample of patients in a particular
geographic location, which may restrict the generalizability of results to
other populations or locations.
1. Universidade do Sul de Santa Catarina, Tubarão,
SC, Brazil
2. Nossa Senhora da Conceição, Tubarão, SC,
Brazil
Corresponding author: André Gabriel Gruber Avenida
José Acácio Moreira, 787, Tubarão, SC, Brazil., Zip Code: 88704-900, E-mail:
andre.gruber@hotmail.com