

Original Article - Year 2023 - Volume 38 -
Bipedicled and structured mammoplasty "in three pillars"
Mamoplastia bipediculada e estruturada "em três pilares"
ABSTRACT
Introduction: Reduction mammoplasty has a long and established history. Since the end of the 19th century, numerous techniques for reducing and elevating breast tissue have been described, seeking the best aesthetic result and greater safety in relation to areolar vascularization and innervation. The purpose of the present study is to describe a new bipedicled and structured mammoplasty technique: safe, reproducible, with a fast-learning curve and predictable esthetic results.
Method: From January 2015 to August 2021, 86 patients underwent surgical treatment of mammoplasty using the technique in question. The analysis of the cases was carried out retrospectively through the evaluation of medical records and review of pre and postoperative photographs.
Results: The support and projection achieved were lasting results. There were no hematomas or necrosis of the nipple-areola complex or other areas.
Conclusion: The technique has high reproducibility, easy execution, high applicability and versatility, extremely satisfactory aesthetic and functional results for surgeon and patient, and above all, a high degree of safety.
Keywords: Mammaplasty; Breast implants; Breast; Reconstructive surgical procedures; Nipples.
RESUMO
Introdução: A mamoplastia redutora tem uma história longa e estabelecida. Desde o final do século XIX, foram descritas inúmeras técnicas para redução e elevação do tecido mamário, buscando não apenas o melhor resultado estético, como também maior segurança em relação a vascularização e inervação areolar. O presente estudo tem como propósito a descrição de uma nova técnica de mamoplastia bipediculada e estruturada: segura, reprodutível, de baixa curva de aprendizado e com resultados estéticos previsíveis.
Método: De janeiro de 2015 a agosto de 2021, 86 pacientes foram submetidas ao tratamento cirúrgico de mamoplastia com a utilização da técnica em questão. A análise dos casos foi realizada de forma retrospectiva, através de avaliação de prontuários e revisão de fotografias de pré e pós-operatório.
Resultados: A sustentação e projeção atingidas foram duradouras. Não houve ocorrência de hematomas ou necrose do complexo areolomamilar ou de quaisquer outras áreas.
Conclusão: Trata- se de uma técnica de alta reprodutibilidade, fácil execução, alta aplicabilidade e versatilidade, resultados estéticos e funcionais extremamente satisfatórios para cirurgião e paciente, além de, principalmente, um alto grau de segurança.
Palavras-chave: Mamoplastia; Implantes de mama; Mama; Procedimentos cirúrgicos reconstrutivos; Mamilos
INTRODUCTION
Reduction mammoplasty is one of the most common plastic surgeries in the world. According to data from the American Society of Plastic Surgeons, there were more than 40,000 procedures in the United States in 20181.
Unlike many surgical procedures, reduction mammoplasty has a long and established history. Since the end of the 19th century and the beginning of the 20th century, numerous techniques have been described for breast tissue reduction, seeking the best aesthetic result and greater safety in terms of vascularization and areolar innervation2. Thorek, in 1922, described amputation of the lower pole of the breast and free graft from the nipple3.
In 1956, when introducing his standard skin resection, Wise4 used preoperative marking, geometric parenchymal resections, and positioning of the nipple- areolar complex (NAC). Wise’s model has become one of the most popular techniques to date2.
The 1960s and 1970s presented several options to improve the pedicle in reduction mammoplasty2. Strombeck5, in 1960, used a bipedicled horizontal flap to maintain the nipple-areola complex, based on the medial and lateral perforators for perfusion associated with the dermoglandular pedicle described by Schwartzman around 19306. The superolateral dermoglandular pedicle was described by Skoog7 in 1963, while Pitanguy and Weiner described the dermoglandular pedicle based on the superior pedicle about 10 years later, in 19738. McKissock9,10, a year earlier, transformed Strombeck’s horizontal bipedicular technique into a vertical bipedicular technique.
Many other surgeons worldwide began to develop reduction mammoplasty techniques using a small scar and based on the superior pedicle throughout the 1980s and 1990s2.
Despite the various studies and techniques described in the literature that address reduction mammoplasty, there is a lack of current studies that describe procedures that use two or more pedicles to reduce breast tissue, as well as consistent results, success rates, and complications1.
The purpose of this study is to describe a new technique for bipedicled and structured reduction mammoplasty: safe, mainly due to greater preservation of breast irrigation, easy understanding and reproducibility, low learning curve, and promising aesthetic results. Furthermore, above all, maintaining the natural shape of the breast brings satisfaction to patients.
OBJECTIVE
To present and describe a new bipedicled and structured mammoplasty technique for treating breast tissue excess, flaccidity, and ptosis that is easily reproducible, simple, safe, and efficient.
METHOD
As of January 2015, the authors began to use the technique described below in their mammoplasties, with a progressive increase in the frequency of its use. As of 2016, they started to use the technique in all their cases of mastopexy without prosthesis and reduction mammoplasty.
From January 2015 to August 2021, 86 patients underwent surgical treatment of mammoplasty using the technique in question. During this period, the authors performed the technique in clinical and hospital settings. Patients who required the use of silicone implants were excluded from the data analysis.
The analysis of the cases was carried out retrospectively through analysis of medical records and review of pre- and postoperative photographs. The elaboration of the article followed the principles of Helsinki.
The volume removed from each breast ranged from zero grams to 1200 grams. The rise of the nipple- areolar complex ranged from 3 to 15 cm, with the marking of point A showing a mean distance to the sternal notch of 19.6 cm.
Technique description
The structured bipedicle mammoplasty technique basically consists of dividing the breast into three parts – which we will call pillars. Thus, the breast is divided into a lateral pillar (L), a medial pillar (M), and an intermediate pillar (I). In this sense, the intermediate portion will be fixed and structured through suture points. The lateral and medial will similarly involve the intermediate, which is already structured.
Marking: we marked the rise of the nipple-areola complex using a bidigital maneuver and Strombeck- Wise molds5. We believe that the type of reduction mammoplasty marking used is not influential in the technique.
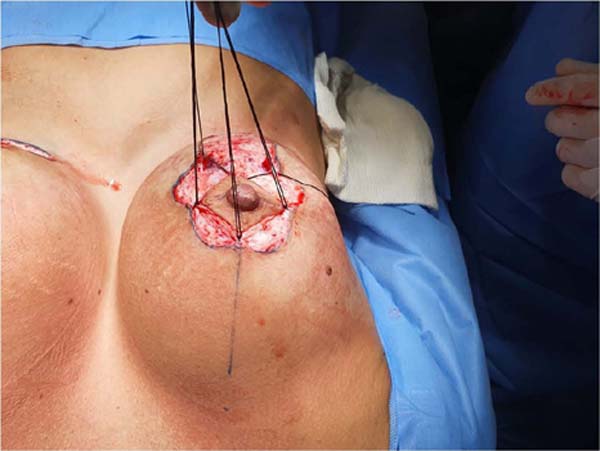
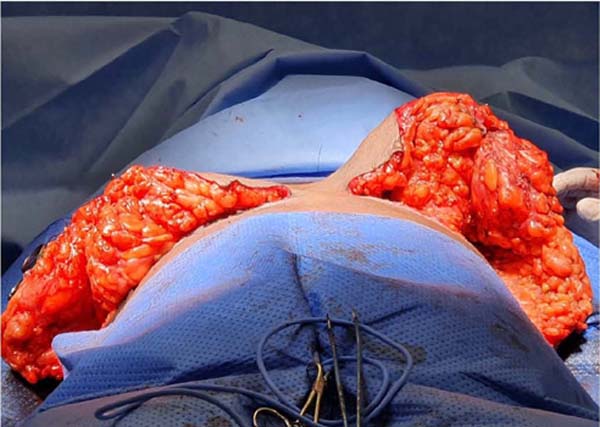
The surgery begins with periareolar de - epidermization, according to Schwartzman6, preserving the innervation and circulation coming from the subdermal plexus, and the superior pedicle areolar flap described by Pitanguy8 is made (Figure 1).
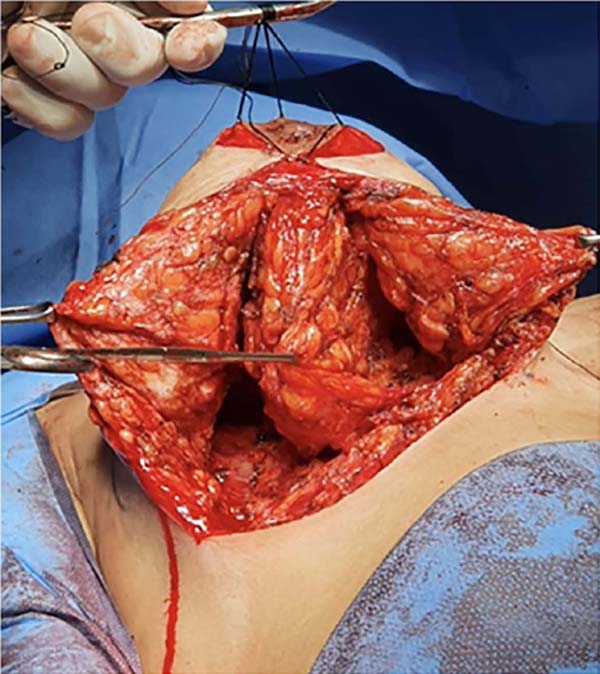
Next, a transverse incision is made 3 cm caudal to the areola, joining the other two longitudinal incisions in this caudal ptosed flap to be resected. These incisions go down to the base of the breast in the inferior mammary fold. At this moment, the entire lower pole exceeding the breast is resected when there are excesses or if you want to reduce the volume (Figure 2). The retroglandular detachment must be limited to the inframammary region and not reach the fifth intercostal space cranially. Thus, the central (or glandular) pedicle containing the intercostal perforating arteries is preserved to irrigate the nipple- areolar complex. In addition, the fourth intercostal nerve, which is of fundamental importance for NAC sensitivity, is preserved11. What remains is a single block running from the clavicular musculature to the fifth intercostal space.
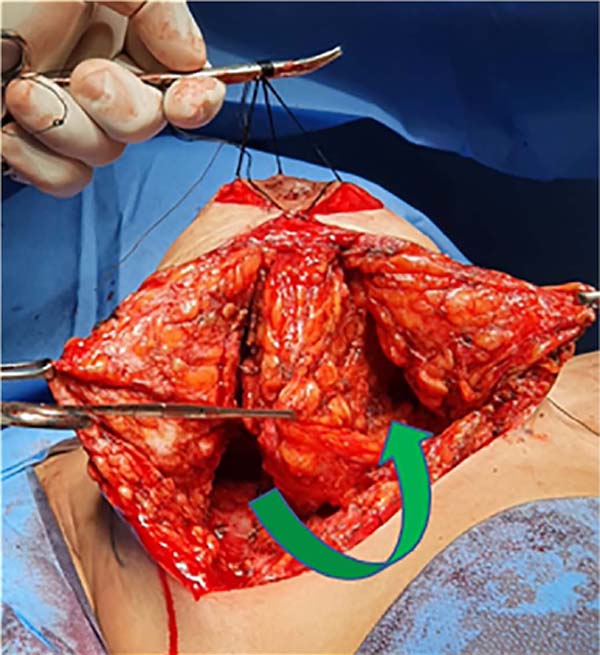
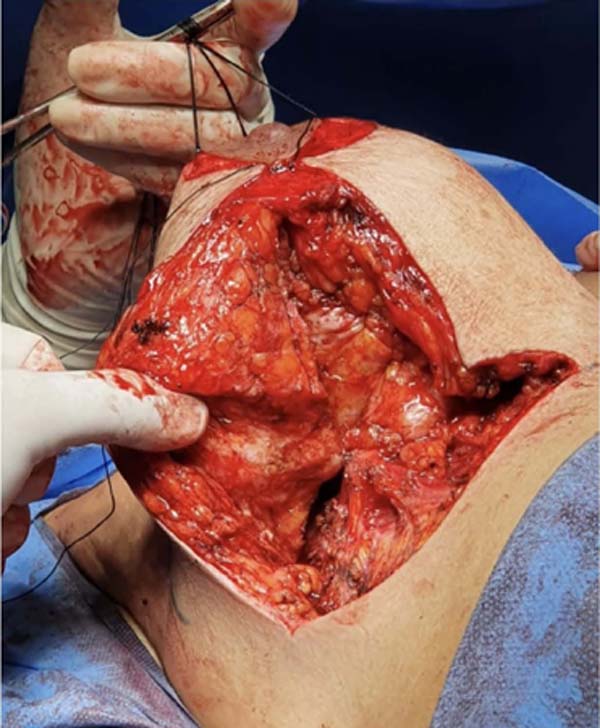
This block will then be divided longitudinally into three parts, three flaps, through two incisions, resulting in a lateral, medial, and intermediate block (Figure 3). This retroareolar intermediate block should be close to the width of the areola (between 3 and 5 cm). The two incisions that will divide this mammary block into three must have the depth of the entire mammary gland, reaching the subcutaneous fat close to the skin (approximately 2 cm). With this, the medial and lateral pillars are released, subsequently involving the intermediate pillar.
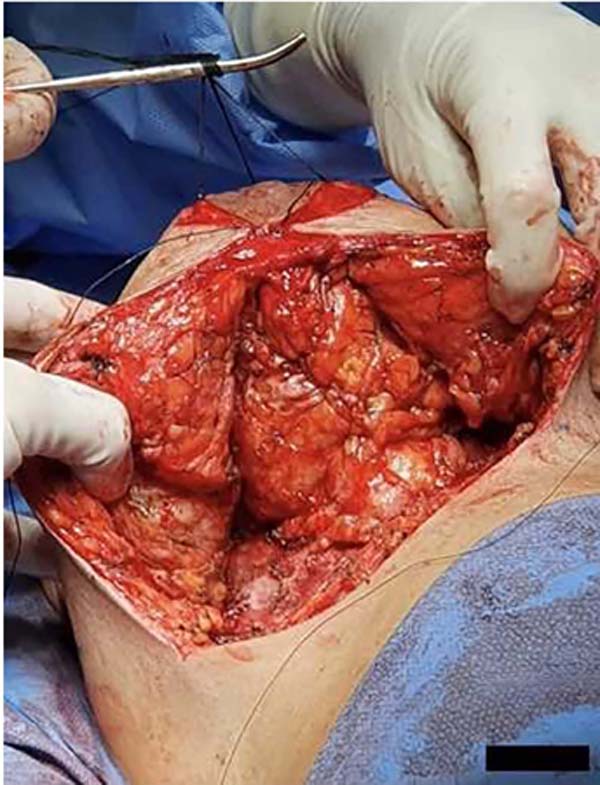
At that moment, the breast can be modeled by reducing or not the medial and lateral pillars, defining the desired projection of the breast (Figure 4). The intermediate abutment must not be reduced or devascularized. Once the necessary reduction has been made on the lateral and medial pillars, the intermediate pillar is modeled and structured – which is pedicled on the perforating arteries of the thorax up to the nipple- areola complex. Thus, in practical terms, the nipple- areolar complex will be irrigated superiorly by the subdermal plexus and superior pedicle and inferiorly by the inferior pedicle, therefore being bipedicled11.
Starting from the nipple-areola complex and towards the pectoral muscle, we measured the desired length of the intermediate pillar. In this location, the lateral border of the intermediate pillar is fixed, through suture, to the pectoral muscle in the most cranial part possible of the incision made for the division of the breast (Figure 5). Other points at the base of the intermediate pillar can be given for greater fixation of the same to the muscle, tensioning and fixing it medially.
Until this moment, the three pillars are still not structured, and the breast has not reached the desired shape and support. For this reason, some X-shaped sutures will be made, joining the lateral and medial edges of the intermediate pillar, making its tubular shape like a cigar (Figure 6). Thus, the successive tensioning sutures promote stiffening of the intermediate pillar, ensuring the greatest breast projection obtained with this technique (Figures 7, 9, and 10).
The next and last step of the surgery will be to pull the medial and lateral pillars towards the mammary sulcus, involving the pedicled and reinforced intermediate tubular pillar. Then, the lateral and medial pillars are advancement flaps that will be pulled toward the submammary crease. This traction must be fixed with Baroudi-type 12 adhesion points throughout its base, avoiding lateral and medial dead space and dispensing with drains13 (Figure 8).
The closure of the skin and the finishing of the areolas can be done as usual by the surgeon.
RESULTS
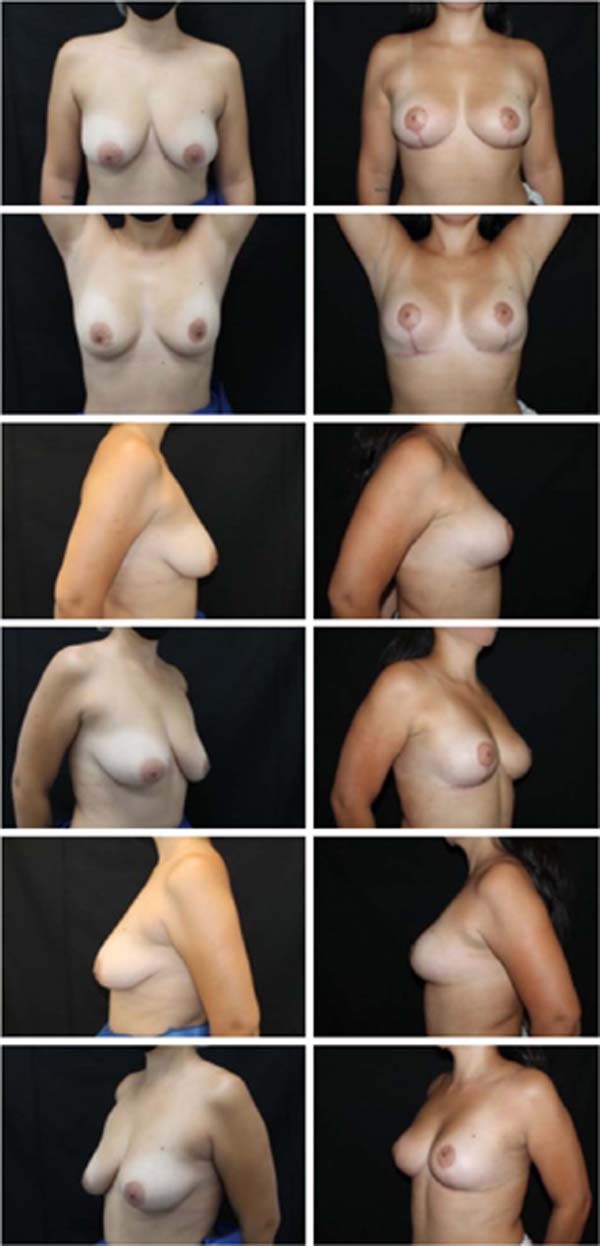
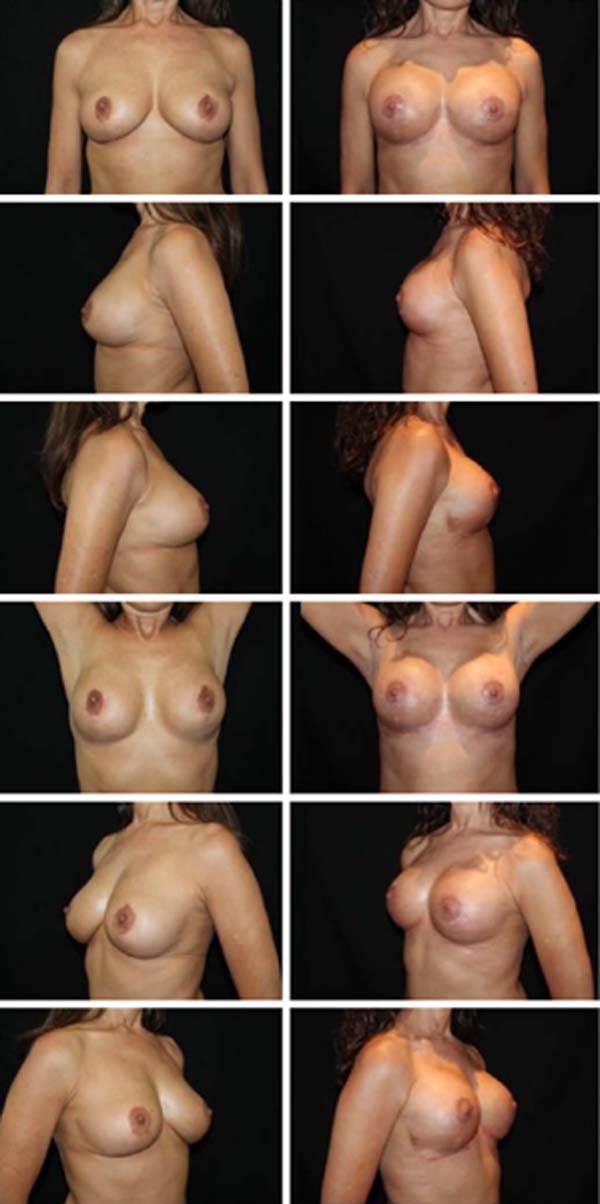
The authors examined results through in-office clinical evaluations and the analysis of standardized preoperative and postoperative photographs at one, six, and twelve months. From an aesthetic point of view, there was a clear improvement in the shape and consistency of the breasts. Subjectively, the aesthetic result was maintained throughout the follow-up period of these patients. The increase in patient satisfaction with the techniques previously used by the authors was also clinically remarkable.
The complication rate was below the average described in the literature14. Of the 86 operated cases, 14 patients had some complication, with 4 suture dehiscence (4.6%) and 9 occurrences of seroma (9.6%), all treated uneventfully conservatively or with a single puncture in the office. There was no occurrence of hematomas that required drainage, surgical or not.
There was also no necrosis of skin flaps, the nipple-areola complex, or ischemic suffering requiring complementary therapy. There was no increase in the rate of other complications, such as infections and sensitivity changes, compared with rates of already established techniques2,14. These numbers allow us to state that this is an extremely safe technique compared to already established mammoplasty techniques (Figures 11, 12, 13, 14, 15, 16, 17).
DISCUSSION
Numerous surgical techniques are described for treating the breasts, many of which are highly acclaimed by Brazilian authors, such as the techniques by Pitanguy8 and Liacyr Ribeiro15.
Some authors already presented bipedicled techniques for mammoplasty, such as McKissock9, in 1972. However, we observed a scarcity of techniques based on double pedicles in the literature.
A systematic review carried out by Wirthmann et al.16 in 2018 showed a rate of complications related to reduction mammoplasties of 33%, and if minor complications that do not involve the need for any reintervention are disregarded, the incidence drops to 9.5%. The most common ones observed were dehiscence and delayed healing of surgical wounds, followed by hematomas. Necrosis of the nipple-areola complex, feared mainly in large reductions and large fixations, had an incidence of 0.7%, all of which were partial16.
The risk of areola necrosis leads the surgeon to prioritize safety when choosing the technique14. Therefore, the vascular pedicles of the chosen flaps will define which surgical technique will be used. The greater the number and the better the quality of the pedicles, the safer the technique will be11. Based on this principle, the authors believe that a bipedicled technique brings greater safety than a single pedicle, whether superior or inferior.
The technique described here is based on a double pedicle, being a superior areolar pedicle, with irrigation coming from the subdermal plexus preserved around the entire areola, in addition to an inferior pedicle, based on the preservation of the main perforators of the thoracic muscles, branches of the internal thoracic arteries and external, from the first to fourth intercostal spaces11. The presence of multiple sources of irrigation for the nipple-areola complex ensures superior safety concerning the vitality of breast tissues14,17,18,19,20,21.
Concerning the innervation of the nipple-areolar complex, the technique provides greater neuronal supply through the superior, subdermal and periareolar pedicle and by preserving the intercostal nerve in the intermediate pillar of the inferior pedicle11.
Another fact that contributes to the safety and prevention of complications is the fact that the lateral and medial pillars are fixed to the thoracic muscles using Baroudi stitches12, reducing dead space in such a way that it significantly reduces the risk of seromas and hematomas, eliminating the need for the use of drains13.
In addition to the increased safety associated with the technique, the authors believe that another important advantage is the possibility of greater breast structuring, with results demonstrating increased consistency and improved shape and contour, with the upper poles becoming more filled without silicone prostheses.
Moreover, it is an easily reproducible technique, with simplicity to perform, a small learning curve, and reducing surgical time compared to other reduction mammoplasty techniques22. It is a versatile technique that can be used both in large breast reductions and in large fixations that do not require the removal of breast tissue.
CONCLUSION
The mammoplasty technique presented here is an innovative proposal that has been carried out since 2015. During this period, 86 patients underwent surgery using the bipedicled and structured mammoplasty technique, with a low rate of complications, most of which were minor. The double pedicle provides great security for preserving the vascularization and innervation of the nipple-areola complex, with no case of necrosis associated with the technique to date. The aesthetic result was surprising, with long- lasting projection and support. Moreover, it is a highly reproducible technique, easy to perform, highly applicable, and versatile, in addition to extremely satisfactory aesthetic and functional results for both surgeon and patient.
1. Hospital da Plástica Contorno, Belo Horizonte, MG, Brazil.
2. Hospital Felício Rocho, Belo Horizonte, MG, Brazil.
3. Núcleo de Cirurgia Plástica, Belo Horizonte, MG, Brazil.
4. Universidade Federal de Minas Gerais, Belo Horizonte, MG, Brazil.
Corresponding author: Victor Izidro Alves de Almeida Avenida do Contorno, 6975, Santa Efigênia, Belo Horizonte, MG, Brazil. Zip code: 30110-076 E-mail: izidrodealmeida1@gmail.com





























 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter