

Review Article - Year 2023 - Volume 38 -
Standardization of reconstructions with flaps after Fournier's gangrene
Padronização das reconstruções com retalhos após gangrena de Fournier
ABSTRACT
Introduction: Fournier's gangrene is characterized by tissue necrosis, which requires treatment employing debridement and antibiotics with wounds of varying sizes. The objective is to standardize the surgical techniques of reconstructions with flaps used to treat wounds after Fournier's gangrene.
Method: A study was conducted by searching the PubMed/Medline, SciELO, and LILACS databases.
Results: In wounds with skin loss of 25% to 50%, a local advancement cutaneous flap or a pudendal flap from the thigh was used; in wounds, greater than 50%, a superomedial thigh flap or myocutaneous flap from the gracilis muscle was used, with the aim of to enable proper reconstruction.
Conclusion: Advancement and pudendal thigh flaps were used for wounds with up to 50% loss of scrotal skin substance, while the myocutaneous gracilis flap and supero-medial flap of the thigh were indicated for wounds with more than 50% of the total scrotal surface affected, after Fournier gangrene.
Keywords: Fasciitis, necrotizing; Fournier gangrene; Surgical flaps; Perforator flap; Myocutaneous flap; Reconstructive surgical procedures
RESUMO
Introdução: Gangrena de Fournier é caracterizada por necrose tecidual, que necessita de tratamento por meio de desbridamento e antibióticos, com feridas de dimensões variadas. O objetivo é padronizar as técnicas cirúrgicas de reconstruções com retalhos utilizadas no tratamento das feridas após gangrena de Fournier.
Método: Realizou-se estudo por meio da busca nas bases de dados PubMed/Medline, SciELO e LILACS.
Resultados: Nas feridas com perdas cutâneas de 25% a 50%, foram utilizados retalho cutâneo local de avanço ou retalho pudendo da coxa, nas maiores de 50% foram necessárias as confecções do retalho superomedial da coxa ou retalho miocutâneo do músculo grácil, com intuito de possibilitar a reconstrução adequada.
Conclusão: Os retalhos de avanço e pudendo da coxa foram utilizados para feridas com perda de substância cutânea escrotal de até 50%, enquanto os retalhos miocutâneo de músculo grácil e superomedial da coxa foram indicados para as feridas com mais de 50% da superfície escrotal total acometida, após gangrena de Fournier.
Palavras-chave: Fasciite necrosante; Gangrena de Fournier; Retalhos cirúrgicos; Retalho perfurante; Retalho miocutâneo; Procedimentos cirúrgicos reconstrutivos
INTRODUCTION
Fournier’s gangrene is an infection caused by aerobic and anaerobic microorganisms1,2, which acting synergistically, determine a necrotizing fasciitis3,4, which affects the genital, perineal, and perianal regions5,6,7. The infection may extend to Scarpa’s fascia on the abdominal wall due to the anatomical communications8,9 existing between the layers of the lining of the perineal, scrotal, penile, and abdominal regions10,11,12.
The infectious process occurs through endarteritis obliterans, which causes thrombosis of the cutaneous vessels and necrosis of the skin in the affected region13,14. Surgical treatment requires debridement of necrotic tissues, causing wounds of varying extents, which require adequate reconstruction15,16.
OBJECTIVE
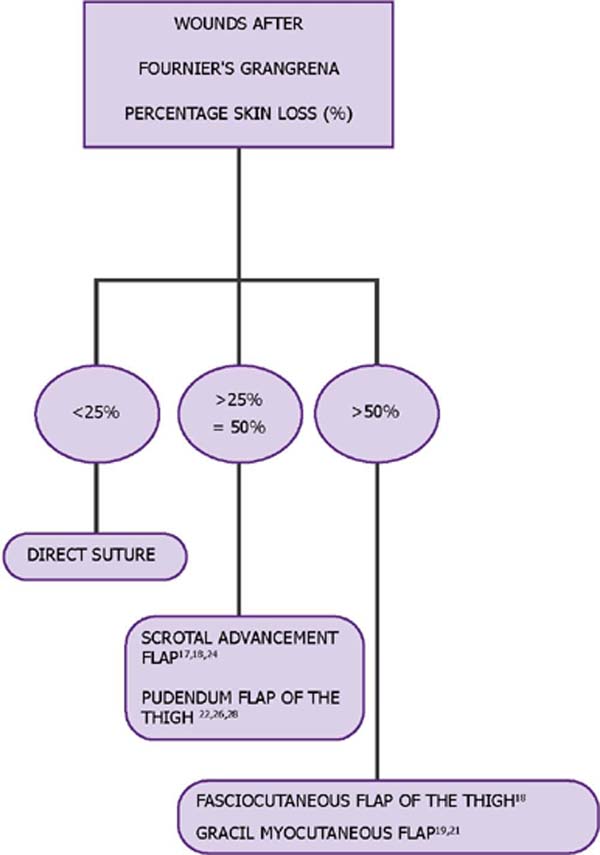
The purpose of the study is to present the standardization of reconstructive surgical treatment of wounds, after Fournier’s gangrene, with the use of flaps, through the elaboration of a flowchart, based on the analysis of the literature.
METHOD
The study consisted of searching for evidence related to surgical techniques for reconstructions after Fournier’s gangrene through a search in the PubMed, SciELO, and LILACS databases, using the descriptors fasciite necrosante (necrotizing fasciitis), gangrena de Fournier (Fournier gangrene), retalhos cirúrgicos (surgical flaps), retalho perfurante (perforator flap), retalho miocutâneo (myocutaneous flap) and cirurgia plástica (plastic, surgery) combined with the Boolean logical operators and or or.
An advanced search was performed, limiting it to words in the title and abstract. All stages of the systematic review were conducted by two reviewers, independently and blindly. The articles related to the descriptors that defined the types of flaps used after Fournier’s gangrene were included. Duplicate articles were excluded, which did not explain the types of flaps used in the reconstructions and those not directly related to the subject.
RESULTS
The results of the study are shown in Table 1 and Figure 1.
| Author | Number of Reconstruction with Flaps* | Kind of study | Surgical technique |
|---|---|---|---|
| Parkash & Gajendran17 | 40 | Retrospective | Scrotal advancement flaps = 40 |
| Ferreira et al.18 | 37 | Retrospective |
Local advancement flaps = 9 Superomedial/thigh flaps = 28 |
| Hsu et al.19 | 8 | Retrospective | Gracilis muscle myocutaneous flaps = 8 |
| Coskunfirat et al.20 | 7 | Retrospective | Perforating flaps of the medial circumflex femoral artery = 7 |
| Lee et al.21 | 14 | Retrospective |
Gracilis muscle flaps = 7 Internal pudendal artery perforating flap = 7 |
| Ünverdi & Kemaloğlu22 | 13 | Retrospective | Internal pudendal artery perforating flaps = 13 |
| El-Khatib23 | 8 | Retrospective | Pudendal thigh flaps = 8 |
| Carvalho et al.24 | 16 | Retrospective | Scrotal advancement flaps = 16 |
| Bhatnagar et al.25 | 12 | Retrospective | Thigh fasciocutaneous flaps = 12 |
| Khanal et al.26 | 14 | Retrospective | Bilateral pudendal flaps = 14 |
| Dadaci et al.27 | 29 | Retrospective | Limberg flaps/thigh = 29 |
| Karaçal et al.28 | 5 | Retrospective | Neurovascular flap / pudendal pedicle = 5 |
* Inclusion and exclusion criteria: cases of reconstructions with flaps were included, and cases of primary closures and skin grafts were excluded.
The flowchart of Figure 1 shows that primary closure was possible in wounds with skin loss of up to 25%. In wounds with skin loss of 25% to 50%, local advancement skin flaps were used.
When skin losses were greater than 50%, it was necessary to create a superomedial thigh flap, pudendal thigh flap, or myocutaneous gracilis muscle flap to enable adequate reconstruction.
DISCUSSION
Flaps can present with complications, such as necrosis, dehiscence, and hematomas. Dehiscence is related to tension in the suture planes, necrosis to the poor blood supply to the vascular pedicle of the flap, and hematoma to inadequate hemostasis17,18,19,20,21,22,23,24,25,26,27,28.
The myocutaneous flap of the gracilis muscle makes it possible to reconstruct wounds with loss of more than 50% of the total scrotal surface, with the advantages of good vascularization, which allows better penetration of antibiotics into the affected tissue, and the ability to fill deep wounds19,20,21.
The scrotal advancement flap offers a good aesthetic result and fulfills the principle of replacing with similar skin, being recommended for scrotal skin loss of up to 50% of the total scrotal surface. The benefits of this method include good skin quality, elasticity, and the presence of the dartos muscle17,18,22,23,24.
The pudendal flap of the thigh has the important benefit of preserving skin sensation in the region reconstructed by the flap, the presence of a reliable blood supply, and low morbidity in the donor area, being used to cover up to 50% of the scrotal skin 22,26,27,28,29.
The superomedial thigh fasciocutaneous flap is indicated for the repair of wounds with skin loss of more than 50% of the total scrotal surface, in a single surgical procedure and with adequate coverage, in patients in a stable clinical condition, after instability resulting from severe gangrene infection of Fournier18,19,20, by aerobic and anaerobic microorganisms12,30,31,32,33,34 associated with diabetes mellitus, heart disease, and renal failure13,14,15.
The surgical technique using the superomedial fasciocutaneous flap1 of the unilateral or bilateral thigh allows the reconstruction of the scrotal region, also indicated for perineal and perianal reconstructions. The superomedial fasciocutaneous flap of the thigh has vascularization through the branches of the femoral artery, the internal pudendal, and the circumflex17, and is safe even in diabetic patients1,35 and patients with vasculopathies36,37.
CONCLUSION
The study carried out allowed us to infer that in the reconstruction of wounds after Fournier’s gangrene, advancement and pudendal flaps from the thigh were used for wounds with loss of scrotal cutaneous substance of up to 50%, while myocutaneous flaps from the gracilis muscle and superomedial thigh were indicated for wounds with more than 50% of the total scrotal surface affected.
1. Universidade Federal Minas Gerais, Faculdade de Medicina, Belo Horizonte, MG, Brazil.
2. Faculdade de Ciências Médicas de Minas Gerais, Belo Horizonte, MG, Brazil.
Corresponding author: Rui Lopes Filho Av. Professor Alfredo Balena, 189, 10º andar, Santa Efigênia, Belo Horizonte, MG, Brazil. Zip code: 30130-100 E-mail: ruilopesfilho@terra.com.br





 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter