

Articles - Year 2001 - Volume 16 -
Silicone Gel Implants for Calf Augmentation: 14 Years Experience
Implantes de Silicone Gel em Panturrilhas: 14 anos de Experiência
ABSTRACT
Based on an experience of 131 operated patients submitted to calf augmentation, the authors describe the indications, surgical technique and complications of the method. The procedure is recommended to correct calf volume of congenital origin, neurological or traumatic sequela.
Keywords: Silicone implants; calf; inclusions
RESUMO
Os autores, baseados na experiência de 124 pacientes operados para introdução de implantes de silicone em panturrilhas, descrevem as indicações e a técnica cirúrgica empregadas em sua casuística, recomendando o procedimento para casos de deficiência de volume de panturrilhas de origem constitucional ou em seqüelas de doenças neurológicas ou traumáticas, chamando a atenção para as vantagens do método e relatando as complicações ocorridas.
Palavras-chave: Unitermos: Implantes de silicone; panturrilhas; inclusões
Since first described by Cronin and Gerow(1) in 1963, silicone implants for calf augmentation have proved to be viable and effective, showing lasting results.
In 1979, Julien Glicenstein(2) pioneered in Paris the implantation of 124 silicone prostheses in 84 patients with poliomyelitis sequela of the lower limb. Later, the works of Carlsen(3), published in 1979, report his experience with 130 cases of muscle atrophy resulting from polio sequela of the lower limb, for both cosmetic and reconstructive purposes.
In our hemisphere, we have the works of Montellano(4) and more recendy of Nicola M Netto(5), demonstrating by extensive statistics the precise indication and efficiency of the method.
Encouraged by the good results of previous papers, in the last 14 years we have operated 131 patients mainly for aesthetic purposes, inserting premolded silicone gelfilled implants with smooth coverage.
PATIENTS AND METHODS
131 patients were operated since 1986, mostly with complaints of thin calfs. 71 % were congenital cases and 29% were due to neurological problems or trauma resulting in muscle atrophy or loss of substance on the area, especially in poliomyelitis.
Most patients (124) were female. Out of the 7 male patients, 4 presented congenital problems and 3 poliomyelitis sequela or trauma (Figs. 1 and 2). A total of 243 implants were used.

Fig. 1 - A: Male patient presenting loss of substance by trauma. B: Postoperative view of placement of individual implant.

Fig. 2 - A: Congenital atrophy. B: Postoperative view after a inclusion of implant in each limb.
93 patients showed congenital atrophy of both limbs, needing only one implant for each calf to correct the deformity. Two implants were also placed in the inner side of both thighs on five of these patients to give the lower limbs contour a more natural aspect (Fig. 3).
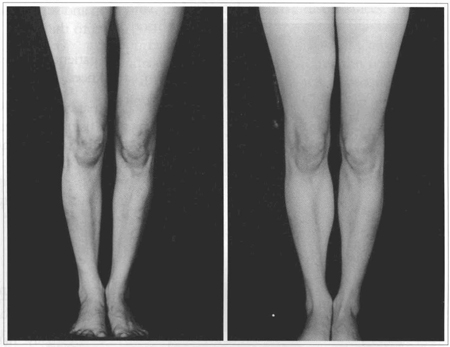
Fig. 3 - A: Hypotrophy of legs and thighs. B: Six months postoperative view of 4 implants inclusion (2 thighs and 2 calfs).
In 38 cases only one of the limbs was operated, in order to correct asymmetry. Among these, 9 patients presented severe polio sequelae and received two implants on a single calf during the same operation, consisting of two separate pockets made under the aponeurosis of the medial and lateral gastrocnemius muscle.
The patients were operated by the same surgical team and referred to the same private clinic.
The two types of premolded implants used were:
The surgeon selects the length, volume and model of the implants according to the biotype and deformity of each patient.
SURGICAL PROCEDURE
The popliteal fold and area to be corrected are marked just before the operation, with the patient in a standing position still in his room. In the O.R. the patient receive epidural anesthesia with or without sedation.
The patient is placed in prone position. A transverse incision approximately 5 cm long is made over the previously marked popliteal fold. After skin and subcutaneous tissues are dissected, the structures superficial to the aponeurosis of the medial gastrocnemius are dearly exposed at the level of the incision. A 2 cm distal undermining is carried out and a transverse incision is made over the aponeurosis on this position. A blum forceps, long enough to reach the distal extremity of the area marked to receive the implant, is introduced and cautiously undermines the muscle aponeurosis so as not to cause any injury The pocket thus created should be 1 cm larger than planned.
A mold is introduced and the result evaluated. We advise to keep at hand other sizes and models in the operation room since the preoperative indication maybe different when compared to the healthy limb or with what was agreed with the patient. Besides, different models or sizes may be needed for both limbs on a same patient.
When the precise size decided, the mold is then removed, 2 or 43.0 mononylon single and key stitches are placed between the aponeurosis borders. The silicone implant is inserted between the key sutures that are firmly tied with the knee slightly flexed.
5.0 mononylon is used both for the subcutaneous tissue with separate inverted stitches and for intradermal running sutures. When needed, the same procedure is carried out on the other limb.
Dressings are with gauze and micropore over the incision and supported by a slight pressure bandage from the leg down to the foot.
The patient is placed in prone position with a support under the knees.
The patient is released after 24-hour hospitalization and may walk using mid pressure supporting stockings. It is requested that the patient maintain a certain degree of rest during the first 5-7 days, with the legs up to avoid edema. After that, walking is no longer restricted, although the supporting stockings must be kept up to the 40th. postoperative day, when normal activity may be resumed.
RESULTS
We found a 97% rate of good results, the criteria of evaluation being as follows:
Complications compromising the final results rated 4% and were excluded from the good result rate. As follows :
As another complication event, one case of immediate postoperative hematoma that we drained in the O.R. and right away reintroduced the implant, presented no hazards to the final result.
DISCUSSION
The premolded gel-filled silicone implant has proved to be fairly satisfactory in our cases (Fig. 4). However, some fell short of the ideal size for a few patients, who wished for larger sizes than those available. A plaster mold to create a customized implant size could have been made, but high costs and time consuming technicalities of such a procedure would make it impracticable (Fig. 5).
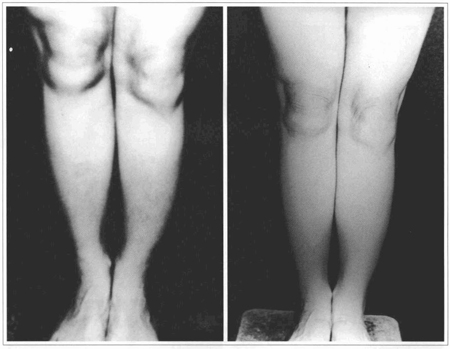
Fig. 4 - A: Post-poliomyelitis atrophy of the left Limb. B: Five years postoperative view of single implant already in place.
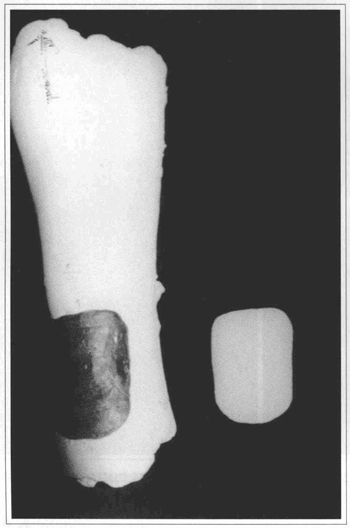
Fig. 5 - Plaster mold to prepare customized implant.
At present, the prevailing opinion commends the inclusion of a smooth/hard silicone gel(6) as it does not rupture easily and inserts easily into the subaponeurotic pocket. Not being available in our market, we did not use this material in our cases and, therefore, we are unable to establish any comparison between results.
Due to a severe complication of compartment syndrome in double implantations on the same limb, we have now abandoned this type of procedure. However, when a second implant on the same limb is required, the operation will be undertaken at least 3 months after the first procedure.
In our experience, surgery of a healthy limb with inclusion of a single prosthesis and adequate technique offers a large margin of success and few complications.
We wish to advise surgeons interested in this field about two major complications of limb implantations. They are the Compartment Syndrome(7) and the Reflex Sympathetic Dystrophy(8) usually seen in the first postoperative days or hours. The characteristics of both are intense pain uncharacteristic to surgical trauma, oedema and sensitive disturbances. Immediate postoperative foot sensitive alteration followed by important oedema and pain show that Compartment Syndrome has settled in, indicates the need for removal of the implant, which will subsequendy promote relief of the symptoms.
When detected at onset, the Reflex Sympayhetic Dystrophy will disappear with instant corticotherapy. Although this complication presents symptoms similar to those of the Compartment Syndrome, these will appear more or less after 7 days postoperatively. Diagnosis is obtained by means of a bone scintigraphy.
At first we used only asymmetric implants; presently we prefer symmetric models that confer a better aesthetic contour to the limb. Asymmetric implants are only used in especial cases, such as those of increased volume deficit at the upper third of the limb.
We believe that a subaponeurotic insertion is more adequate since it provides more regular contours than a subcutaneous approach. It is also an easier and less risky procedure than the submuscular insertion commended by some authors.
In spite of their smooth coverage, no capsular contracture was observed on the calf implants in an observation period of 10 years of most of the cases. We believe that the vigorous and constant massage of the steady movement of the gastrocnemius muscle over the implant since the first postoperative day is responsible for the absence of fibrous capsule formation (Fig.6).

Fig. 6 - A: Patient presenting disproportional implants. B: 13 years postoperative view after the replacement of implants in each limb.
Calf implant complications affect mostly atrophied limbs that have less tissue elasticity and is, therefore, more susceptible to compression. Complication rate in our casuistry was unimportant.
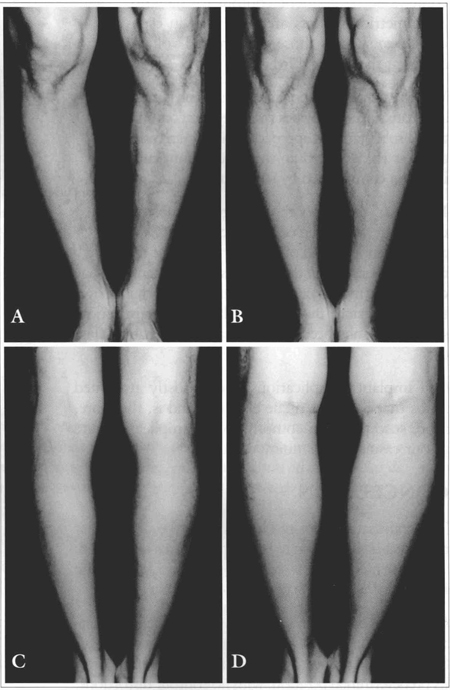
Fig. 7 - A: Male patient presenting Geno Varo congenital deformity. B: Postoperative anterior view. C: 7 months postoperative after injection of 120 ml of Glicenstein in each leg. D: Postoperative posterior view showing almost imperceptible scars.
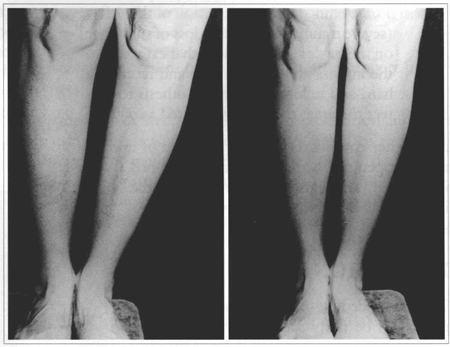
Fig. 8 - A: 60 years-old patient presenting congenital hypertrophy. B: 2 years postoperative of a 140 ml implantatin in both legs.
CONCLUSION
To obtain satisfactory results one must be certain that the defect is situated on the two upper dllids of the limb, an area that is subject to correction by this method. The lower third will not be corrected adequately.
Surgical procedure must be followed precisely, with attention to the correct plane (subaponeurotic) and sufficient undermining to easily introduce the implant in its predetermined position, with no contour distortions.
Since Compartment Syndromes usually occurs during the immediate postoperative of limbs atrophied by neurological or traumatic disorders, this period should be closely observed.
Based on our experience of gel-filled silicone prosthesis implantation in the calf of 131 patients, we believe this procedure to be surgically safe and efficient to 16 correct deficient calf volume of congenital or neurological origin.
REFERENCES
1. REES TD. Plastic surgery of the breast. Converse JM, Littler JW. Reconstructive plastic surgery. WB Saunders, 1965. v. V, pp. 1930-1.
2. GLICESTEIN J. Correção das amiotrofias dos membros com implantes de silicone. Rev. Soc. Bras. Cir. Plást. 1979; 69:117-21.
3. CARLSEN LN. Calfaugmentation: a preliminary report. Ann. Plast. Surg. 1979; 2:508-12.
4. MONTELLANO L. Plástica de panturrilha. Anais do XXI Congr. Bras. Cir. Plást. 1984.
5. MENICHELLI N. Correction of limb deformities with silicone prostheses. Aesth. Plast. Surg. 1999; 23:13-17.
6. OTERO NUNES G. Personal communication. II Raps recent advances. Plastic Surgery, São Paulo, Brasil, 1991.
7. MUBARAK SJ, HARGENS AR. Síndromes compartimemais agudas. Clin. Cir. Am. Norte. 1983; 3:569-98.
8. ROCKWOOD DC, GREEN D, BUCHOLZ R. Fraturas em adultos. São Paulo: Manole, 1993. p.377-84.
I - Senior Member, Brazilian Society of Plastic Surgery.
Address for correspondence:
Augusto Cesar Teixeira, MD
Av. N. S. Copacabana, 1183/302
22070-010 - Rio de Janeiro - RJ Brazil
Phone/fax: (55 21) 267-6512
e-mail: cirmao@terra.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter