

Case Report - Year 2023 - Volume 38 -
Preoperative clinical management of patients who are candidates for facial transplantation
Manejo clínico pré-operatório de pacientes candidatos ao transplante facial
ABSTRACT
Introduction: Face transplantation has gained recognition, changing the clinicalsurgical scenario for restoring complex facial defects, as it attributes functional and aesthetic recovery to patients who have suffered serious accidents. At the time of writing this article, in official publications, 43 patients had already undergone facial transplantation worldwide. Face transplantation has numerous pieces of evidence that can irrefutably provide improvements to the patient. For this, preoperative care for the patient must be carefully established so that there is good surgical performance.
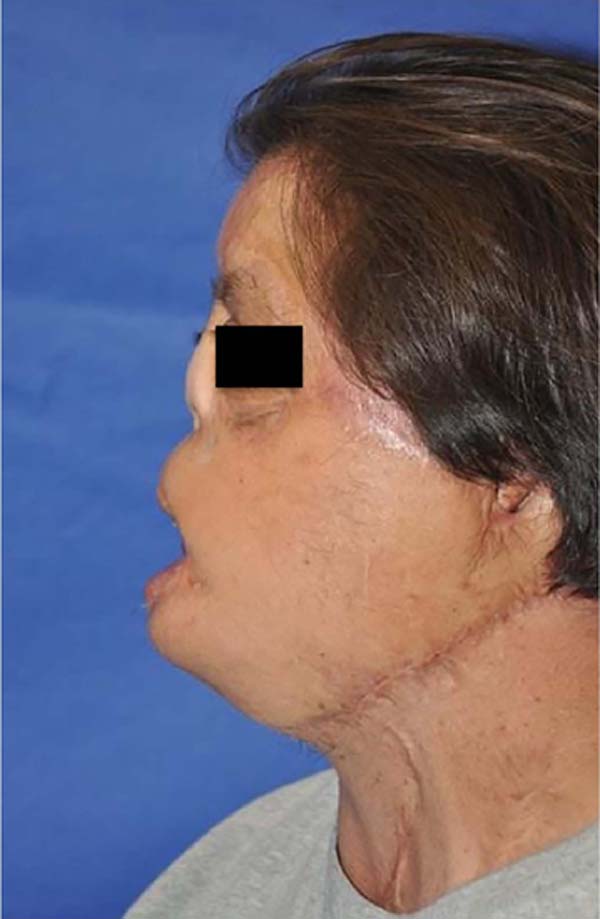
Case Report: Male patient, 46 years old, reports that, at the age of 6, he had burns due to exposure to gasoline, with 72% of his body surface burned, showing sequelae of burns and surgical reconstructions on the face, with redundant and ptotic skin flap on the left cheek, absence of upper and lower lip and exposure of lower teeth.
Conclusion: It is important to publicize this innovative procedure in different medical specialties and preoperative care through a thorough investigation, which attributes better surgical effectiveness, allowing the rescue of their facial identity, once stigmatized.
Keywords: Preoperative care; Facial transplantation; Critical pathways; Reconstructive surgical procedures; Burns; Case reports
RESUMO
Introdução: O transplante de face adquiriu reconhecimento, alterando o panorama clínico-cirúrgico para a restauração de defeitos faciais complexos, visto que atribui recuperação funcional e estética a pacientes que sofreram acidentes graves. Até o momento da redação deste artigo, em publicações oficiais, 43 pacientes já haviam realizado o transplante facial em todo mundo. O transplante de face possui inúmeras evidências que podem fornecer melhorias ao paciente de forma irrefutável. Para isso, cuidados pré-operatórios ao paciente devem ser cuidadosamente estabelecidos para que haja um bom desempenho cirúrgico.
Relato de Caso: Paciente sexo masculino, 46 anos, relata que, aos 6 anos de idade, teve queimadura por exposição à gasolina, com 72% de superfície corporal queimada, apresentando sequelas de queimaduras e reconstruções cirúrgicas na face, com retalho cutâneo redundante e ptótico em bochecha esquerda, ausência de lábio superior e inferior e exposição dos dentes inferiores.
Conclusão: Ressalta-se a importância da divulgação desse procedimento inovador em diferentes especialidades médicas e dos cuidados pré-operatórios através de uma investigação minuciosa, que atribuem uma melhor eficácia cirúrgica, possibilitando o resgate de sua identidade facial, uma vez estigmatizada.
Palavras-chave: Cuidados pré-operatórios; Transplante de face; Procedimentos clínicos; Procedimentos cirúrgicos reconstrutivos; Queimaduras; Relatos de casos
INTRODUCTION
Face transplantation has acquired recognition, changing the clinical-surgical panorama in restoring complex facial defects since it attributes functional and aesthetic recovery.
A study in 2019 in the United States revealed that the incidence of craniofacial injuries by firearms increased by about 31.7%, that of burns reached 240.2%, and that of animal attacks to 173.9%1. Thus, the insertion of facial transplantation in medical practice aims to improve the quality of life, as it reintegrates the functions of swallowing, speech, and the patient’s psychosocial integration.
In 2005, in Amiens (France), the first partial face transplant was performed after the patient was affected by an animal attack. Since then, the procedure has been performed for more than 10 years, seeking surgical improvement, as there is a great clash regarding the numerous risks and immunosuppression, making this procedure, for many, something experimental with unfinished ethical questions, such as adherence and psychological maturity, risks of opportunistic infections and malignancies due to extensive tissue exposure2.
To perform the transplant, the degree of health of the patient and their comorbidities are taken into account, in which the main method of choice for surgeons is vascularized composite allotransplantation (VCA). It refers to the transplant that includes the three embryological layers of multiple tissues in a functional unit, such as muscle, bone, nerve and skin, subcutaneous tissue, blood vessels, and tendons; being from a deceased donor to a recipient with a severe injury, tolerating only a limited period of ischemia, with the rapid establishment of blood flow3.
Adequate revascularization and the functional and aesthetic reintegration of the surgical process are the ultimate goals to be achieved with facial transplantation. However, the major obstacle still being faced is immunosuppression due to the need to change numerous structures on the face and in adjacent areas, making long-term pharmacological use almost inevitable, with potentially fatal side effects, which requires a rigorous medical assessment concerning risk-benefit3,4.
In official publications, at the time of writing this article, 43 patients have already undergone facial transplantation, with only five deaths due to complications of non-adherence to medication, the appearance of tumors, trauma, neoplasms, or unknown cause4. Face transplantation has numerous pieces of evidence that can irrefutably provide improvements to the patient. Thus, it becomes relevant to carry out the present work, which aims to describe an experience of a candidate for facial transplantation in Mexico City - Mexico, in addition to conducting a discussion with an emphasis on preoperative clinical management.
CASE REPORT
Identification
ASM, male, 46 years old, brown, with a high school education, works in a company that manufactures sports uniforms, with residence in Celaya, Mexico.
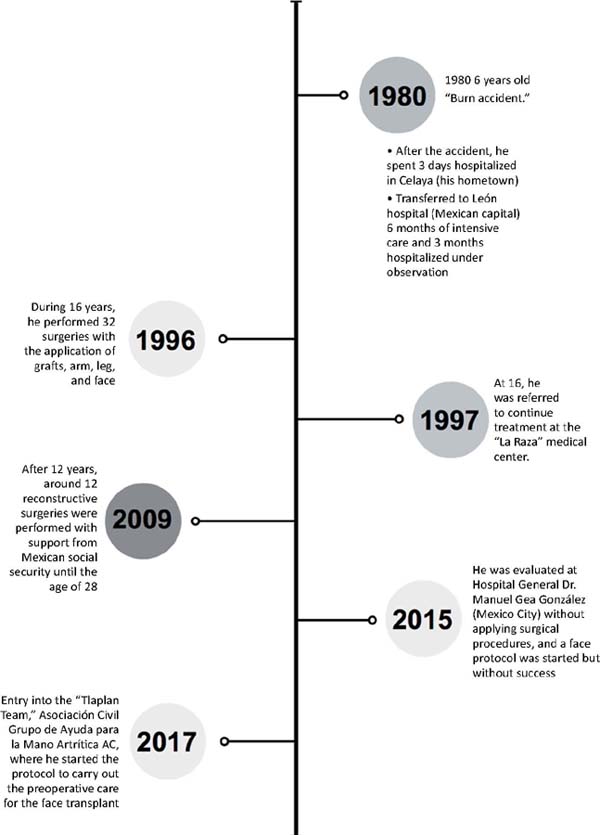
History of current illness (HDA) (Figures 1 and 2)
He reported no visual acuity complications but with the presence of epiphora and bilateral ectropion. Concerning hearing, he denied alterations, with the absence of the left ear and half of the right ear, intact tongue, and difficulty swallowing fluids. He had a loss of nose, with predominantly oral breathing. He had sequelae from burns and surgical reconstructions on his face, with unstable skin.
After an initial evaluation with the plastic surgeon, he underwent a multidisciplinary analysis, namely: specialist in Transplants; Psychiatry; Psychology; Social work; Anesthesiology; Infectology; Occupational Therapist; Neurology; Cardiology; Dentistry; Oral and maxillofacial surgeon; Ophthalmologic Oculoplastics; Urology; Otolaryngology; Internal medicine; Bioreproduction and Nutrology.
Pathological Personal History (PPH)
Diagnosed with type 2 diabetes mellitus in 2017, controlled with metformin; latent tuberculosis diagnosed and treated with isoniazid; multinodular goiter with aspiration biopsy, reporting a hyperplastic nodule and Bethesda II and epidermoid cancer in the burned area of the right forearm, resected in 2017.
General Physical Examination (GPE)
The patient was in good condition, conscious and oriented in time and space, with indifferent attitude and decubitus, facies with changes secondary to facial burn. Patient with severe limitation of movement of the left hand and other extremities with cicatricial lesions.
Orofacial Clinical Examination (OCE)
The skin flap that replaced the nose has two orifices, the left of which is permeable with a flattened shape in a microstoma aspect (resembles the nostrils of a fish) (Figure 3). The atrophic upper lip with a thin red border. The hypertrophic lower lip with multiple scars, both rigid, which prevent manual traction to visualize the labial vestibules.
The malpositioned right maxillary second molar turned inwards partially. Maxillary dental arch with dental crowding. Generalized gingivitis. The right anterior dentoalveolar process is protuberant and exposed outside the mouth.
It has gingival retraction, with lingual root exposure on the right second molar (Figure 4). Other regions analyzed in the buccal area without other alterations. He has Angle class I malocclusion with a crossbite. The maximum oral cavity opening of 3.6 cm is not painful.
Specialty Assessments (SA)
Ophthalmology
The patient reports chronic lacrimation. Upper eyelids with mild dermatochalasis. Lower lid of the right eye with severe tarsal ectropion; Lower left eyelid with retraction. Anterior lamina of the eyelid with a skin graft. 5mm lagophthalmos bilaterally. The cornea with fine dots, a photo-reactive iris, transparent lens.
Psychology
He has the intellectual resources necessary for efficient decision-making, allowing him to be voluntarily and responsibly involved in this transplant protocol. No evidence of symptoms of depression or anxiety. He has stabilized cognitive capacity concerning his physical image (face).
In addition, one of the required criteria is applying a Stanford Integrated Psychosocial Assessment form for Transplantation (SIPAT). It is identified as a high risk of rejection, infection, and mortality. A score greater than 42 is considered incompatible with a successful transplant. However, ASM was considered psychologically adequate for being below the value.
Donor preoperative plan
In the frontal region, the compound flap will be raised subperiosteally until it finds the origin of the supraorbital nerves. The dissection of the frontal flap will be continued in its superficial lateral portion of the aponeurosis of the temporal muscle up to the upper edge of the zygomatic arch. At the neck level, the common carotid, internal and external carotid, and facial arteries will be identified, as well as the external and internal jugular vein and facial vein.
The upper eyelid will be dissected bilaterally above the levator palpebrae aponeurosis in the orbital region.
Elevation of the nasal floor mucosa and the mucosa of the lateral wall of the upper jaw will be performed. It will be sectioned from the insertion of the nasal septum of the palatine crest.
Complementary Exams (CE)
Electrodiagnosis and Electromyography
In the functional evaluation of the facial muscles, facial asymmetry was found at the expense of the right hemiface; on muscle examination, the following classification was identified (Table 1).
| Muscle | Qualification | Sensitivity | ||
|---|---|---|---|---|
| Right | Left | Trigeminal Nerve | ||
| Frontal | 3 | 3 | ||
| Eyebrow Corrugator | 2 | 2 | Preserved ophthalmic branch | Preserved ophthalmic branch |
| Orbicularis oculi | 2 | 3 | Preserved maxillary ascending branch | Preserved maxillary ascending branch |
| Buccinator | 1 | 1 | Maxillary descending branch preserved | Maxillary descending branch preserved |
| Nasal wing lift | 2 | 2 | ||
| Orbicularis oris | 1 | 1 | ||
| Mentonian | 2 | 2 | ||
| Platysma | 3 | 3 | ||
Assessment of facial movement according to House and Brackmann (1985) presenting grade I V, being moderately severe dysfunction with normal symmetry and tone at rest and in movement. The frontal region is absent, the eyes with incomplete closure, and the asymmetrical mouth with maximum effort.
Echocardiogram (January/2019)
Systolic function with an ejection fraction of 68% and impaired systolic dysfunction with a type I filling pattern.
Carotid and vertebral Doppler ultrasound (January/2019)
Presence of common carotid artery, internal and external carotid artery with regular walls; thickness of the intima and media layer in normal parameters, not being identified atheromatous plaques or stenotic lesions. Doppler demonstrates anterograde flow and maintains its settings, velocities, and resistance index within normal parameters.
Vertebral arteries with anterograde flow and velocity in normal parameters. A tracing of the jugular and external veins is also performed, in which permeable veins with an adequate flow are observed.
Laboratory tests (January/2020) (Table 2)
| Exams | Result | Exams | Result |
|---|---|---|---|
| Glycemia | 106 mg/dl | Hematocrit | 45% |
| Erythrocytes | 5.10 106/mm3 | Hemoglobin | 15.2 g/dl |
| Leukocytes | 5,295 mm3 | Segmented | 68% |
| Platelets | 155,000 mm3 | AST | 38 U/L |
| Glycated hemoglobin | 6.2% | ALT | 58 U/L |
| Urea | 29.96 mg/dl | GGT | 93 U/L |
| Serum creatinine | 0.73 mg/dl | Prothrombin time (TAP) | 12s |
| Serum sodium | 140.0 mmol/L | Activated partial thromboplastin time (APTT) | 31s |
| Serum potassium | 4.2 mmol/L | Hbsag | Negative |
| Serum chlorine | 105.0 mmol/L | Anti-HCV total | Non-reactive |
| Serum calcium | 11.33 mg/dl | Anti HAV | Negative |
| Serum phosphorus | 1.9 mg/dl | Anti HIV | Non-reactive |
| Uric acid | 7.45 mg/dl | Anti-hepatitis D | Negative |
| Total cholesterol | 145 mg/dl | C-reactive protein Ultrasensitive | 1.59 mg/dl |
| Direct bilirubin | 0.21 mg/dl | Anti Epstein Baar Ag capsid VCA IgM | 1.56 index |
| Indirect bilirubin | 0.34 mg/dl | Anti-Epstein Baar Ag capsid VCA IgG | 4.56 index |
| Creatine phosphokinase (CKMB) | 26 U/L | Cytomegalovirus IgG | Negative |
| Globulin | 4 gr/dl | toxoplasma IgG | Negative |
| Lactic dehydrogenase (LHL) | 240 U/L |
DISCUSSION
Among the 43 cases already published, in which 13 patients had trauma etiology from extensive burns, only 28 mentioned some management guidelines regarding the pre-transplantation period. In addition, only one study correlates the necessary preoperative care and its applications in the context of immunizations necessary to perform the procedure5.
In general, before transplantation, patients report depressive symptoms and changes in quality of life. In this way, potential candidates undergo a psychosocial assessment. As in the report, the patient can perform his daily activities6.
Caring for these patients offers unique challenges, including immunosuppression, allograft rejection, and impaired communication. ASM underwent a strict screening established by the protocol, identifying new comorbidities that influenced the delay of such a procedure.
The patient was chosen because he was a victim of a burn accident, with 72% of his body surface burned, with more than 40 surgeries without significant progress. According to the American Society of Plastic Surgeons (SACP) and the Society for Reconstructive Microsurgery (SMR), facial transplantation should be performed in patients with severe facial dysfunction, with a loss greater than 25% and after exhaustion of conventional techniques with results unsatisfactory. Therefore, the patient continues to be able to perform preoperative management7.
Furthermore, due to the extent and depth of the burns on the central units of the face, the patient is using a nasal prosthesis in addition to presenting occlusion of the nasal passage, which is reflected in the change in his sleeping habits and the appearance of sinusitis in the left maxillary sinus.
This was similarly demonstrated in two patients who had an exposed nasal cavity with airway occlusion before the transplant and required a prosthetic nose. After facial transplantation, although there was no significant improvement in sleep disturbance, there was a successful restoration of the airways, nasal breathing without obstacles, and the disappearance of sinusitis after some surgical corrections due to the alignment of the donor’s septum7,8.
Inadequate characteristics such as immunosensitization, neuropathology, and adverse reactions represent obstacles to performing surgery. What was not identified in the report, as it presented complete stability in the evaluations and without reactional manifestations8.
Similar to the reported case, a patient who underwent a face transplant was found with the same orofacial characteristics, in which, after the transplant, there was a return of facial agraphesthesia and motor improvements after the 6th month9.
Laboratory monitoring of fasting blood glucose and glycated hemoglobin is of great importance in the patient already has type 2 diabetes mellitus, one of the early complications found in post-transplant patients: transient diabetes9. A patient with a similar clinical picture was identified, who evolved positively with drug treatment after transplantation.
The negative reaction to the cytomegalovirus immunological test was a preponderant factor for management since it influences the degree of allograft dysfunction and patient morbidity and mortality. The mechanism is still unclear, but all patients who developed such an infection were successfully treated with antiretroviral therapy10.
Multiprofessional strategies are launched because of the complexity of this procedure and its repercussions in the pre- and post-surgical phases.
Currently, the patient is in the stabilization phase under control of diabetes mellitus and systemic arterial hypertension, identified during the preoperative period, necessitating the postponement of the procedure. In addition, he is waiting for a compatible donor.
CONCLUSION
A case on the preponderant care for a facial transplant was detailed. Although there is little medical knowledge in Brazil, this is a reality in many developed countries, where the patient manages to enable the return of his skills and facial expressions with a potentially natural appearance.
Furthermore, laboratory and multidisciplinary follow-up within the scope of the preoperative evaluation over a long period is essential since it increases the possibility of detecting possible comorbidities, and they are resolved before the surgical procedure.
It is important to publicize this innovative procedure in different medical specialties and preoperative care through a thorough investigation, enabling the recovery of their facial identity once stigmatized.
1. Grupo de Ayuda para la Mano Artrítica AC, “Tlalpan Team”, Medicina, Tlalpan, Cidade
do México, Mexico
2. Centro Universitário do Estado do Pará (CESUPA), Medicina, Belém, Pará, Brazil
Corresponding author: Mateus de Sousa Borges Rua Municipalidade, 985, sala 2112, Umarizal, Belém, PA, Brazil. Zip code: 66050-350 E-mail: mateus.sousa.borges@hotmail.com











 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter