

Ideas and Innovation - Year 2023 - Volume 38 -
Double transposition flap for lower eyelid reconstruction: case report of a new surgical approach
Retalho de dupla transposição para reconstrução de pálpebra inferior: relato de caso de uma nova abordagem cirúrgica
ABSTRACT
Introduction: Non-melanoma tumors frequently affect the lower palpebral region and constitute a challenge for reconstructing the surgical wound without causing functional or aesthetic changes. Primary closure is generally impossible, and flaps are preferred over grafts as they generate less eyelid retraction. This article aims to describe a new surgical reconstruction technique.
Method: A modified McGregor flap technique is described for correcting a surgical defect greater than 50% of the anterior lamella of a recurrent basal cell carcinoma lesion in the lower eyelid.
Results: The patient was evaluated on the 7th, 14th, 21st, and 45th postoperative days. She presented a good functional and aesthetic response to the technique used.
Conclusion: Using the double transposition flap, we demonstrate a new technique for closing defects larger than two-thirds in the lower eyelid.
Keywords: Reconstructive surgical procedures; Surgical flaps; Carcinoma, basal cell; eyelid neoplasms; Eyelids
RESUMO
Introdução: Os tumores não melanomas acometem frequentemente a região palpebral inferior e consistem em um desafio para a reconstrução da ferida operatória sem ocasionar alteração funcional ou estética. O fechamento primário geralmente não é possível e os retalhos são preferenciais aos enxertos por gerarem menor retração palpebral. Este artigo tem como objetivo descrever uma nova técnica de reconstrução cirúrgica.
Método: Descreve-se técnica modificada do retalho de McGregor para correção de defeito cirúrgico maior que 50% da lamela anterior, de lesão recidivada de carcinoma basocelular localizada em pálpebra inferior.
Resultados: Paciente foi avaliada no 7º, 14º, 21º e 45º dia de pósoperatório. Apresentou boa resposta funcional e estética com a técnica utilizada.
Conclusão: Demonstramos uma nova técnica de fechamento de defeitos maiores do que dois terços na pálpebra inferior através do retalho de dupla transposição.
Palavras-chave: Procedimentos cirúrgicos reconstrutivos; Retalhos cirúrgicos; Carcinoma basocelular; Neoplasias palpebrais; Pálpebras
INTRODUCTION
Cutaneous neoplasms are frequent on the face and cause functional and aesthetic morbidity in patients, with basal cell carcinoma (BCC) being the most common type1. Melanoma and non-melanoma skin cancer affect the eyelid region in 5 to 10% of cases2. Reconstruction of the lower eyelid after excision of neoplasia or trauma is challenging due to the small amount of excess tissue.
The choice of the best flap depends on the location, size, and depth (if there is tarsal involvement, that is, the posterior lamella). Superficial surgical defects only require reconstruction of the anterior lamella (skin and muscle), whereas full-thickness defects require both anterior and posterior lamellae (tarsus and conjunctiva) to be reconstructed3,4. This article aims to describe a new technique option for surgical wound reconstruction.
Flaps are preferred in defects greater than 33% of the affected eyelid to avoid retraction of the area and prevent ectropion due to the vertical tension at the site. The flaps most used for eyelid reconstruction are advancement with or without canthotomy; transposition; mustard; McGregor; Fricke; Landolt-Hughes; Dutupuys-Dutemps-Hughes (uses skin and mucosa of the upper eyelid); and Abbe3.
OBJECTIVE
This article presents a new surgical proposal to facilitate the reconstruction of the lower eyelid when the anterior lamella is affected by more than two-thirds, using a double transposition flap.
METHOD
Female patient, 70 years old, with recurrence, 9 years after the first surgery without margin control, of BCC in the topography of the lower right eyelid, was admitted to Instituto Azulay in Rio de Janeiro, RJ. A pearly lesion appeared 6 months ago on clinical examination, with exulcerations and 19x12mm in diameter (Figure 1). Dermoscopy revealed the presence of erythema, ulceration, maple leaves, some ovoid nests, and chrysalis.
On October 19, 2021, the patient underwent local anesthesia with Klein’s modified tumescent solution and complete tumor excision with intraoperative freezing. After enlarging the surgical margins of an infiltrative BCC, a defect greater than 50% of the anterior lamella was obtained (Figure 2).
The McGregor flap was chosen first to close the wound; however, due to the tissue’s low mobility, it was impossible to perform the programmed flap advancement movement after interpolating the z-plasty triangles.
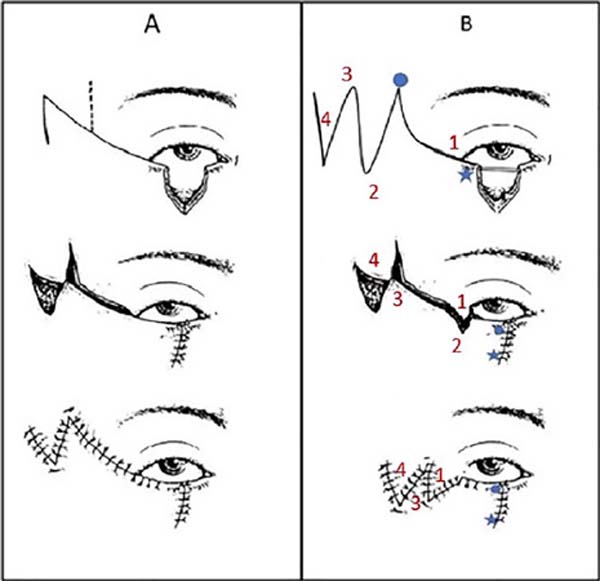
Therefore, the McGregor flap was modified. After making an M-shaped incision in the temporal region – lateral to the defect – two symmetrical triangles were created with their largest axis, the size of the largest radius of the wound (Figure 3). The tissue was detached from the malar and temporal regions, and the first triangle was transposed towards the wound to close the primary defect, and then the second triangle was transposed to close the area of the first triangle. Finally, the space of the second triangle was primarily closed. Thus, the movement of the first triangle was a combination of transposition and rotation movements to move the tissue toward the surgical wound.

Gilles stitches were made to fix each tip of the transposed triangles and internal and external stitches with mononylon 5.0 (Figure 4).
RESULTS
The patient had no major complications during the postoperative period. Eyelid swelling is expected, with difficulty opening the eyes and a slight hematoma in the first days after surgery, which usually resolves within a week. She received prophylactic antibiotic therapy with cefadroxil. The stitches were removed on the 14th postoperative day, and from the 21st day onwards, massage was recommended for drainage of residual edema and photoprotection. The photos were taken immediately, on the 7th, 14th, 21st, and 45th postoperative days (Figure 5).
The result was satisfactory, maintaining aesthetics and local functionality and providing a discreet and barely perceptible scar.
DISCUSSION
Eyelid reconstruction is challenging due to this area’s anatomical and physiological characteristics. It is mainly based on two factors: thickness and extension of the defect5. The lower eyelid and medial canthus are the most affected regions, and these periorbital cutaneous tumors can be difficult to manage, commonly treated with surgical excision6.
Although many surgical techniques are available, there is no preferred method of choice. Among the available modalities for closing the lower eyelid transposition flaps such as the Tripier, which consists of a myocutaneous transposition flap, the Fricke flap, the Kreibig flap, and the nasolabial flap with an upper base. Among the advancement flaps, there is the McGregor (which associates the advancement technique with z-plasty) and the Imre flap. As for the rotation ones, the Mustardè technique is a widely used option to repair extensive defects in the anterior lamella of the lower eyelid or combination with cartilage and mucosa grafts to close the posterior lamella7.
The transposition flap with zetaplasty is a possibility for closing several surgical defects on the face, as it allows a complete redirection of the stress vector through islands of healthy skin. Due to these characteristics, it is indicated for closing defects close to the free margins, such as the nasal wing, lips, helix, and eyelids8.
In 1973, McGregor published the lateral periorbital z-plasty associated with forward movement, an excellent alternative within the reconstructive therapeutic arsenal6,9. In this case, z-plasty is performed at the lateral end of the incision, with the defect’s width corresponding to the central branch of the Z. The lateral descending branch and the ascending branch of the Z are the same length as the central branch and form an angle of 60 degrees with it. Lateral canthotomy is performed to allow advancement of the flap and coverage of the eyelid defect. After interpolation of the flaps, any excess skin is trimmed6,9.
In contrast, instead of performing the forward movement after interpolation of the z-plasty triangles, in this patient, we performed an M-shaped incision. We combined the movement of transposition and rotation of the first triangle (Figure 6) with the subsequent transposition of the second triangle. In the other studies found in the literature, the construction of a double, triple, or even quadruple transposition flap is performed at opposite angles and equidistant from the largest diameter of the surgical defect. However, in this case, there would be a risk of ectropion, a different technique than those already published.
Thus, this report demonstrates a technique of a double transposition flap, in which its design was inspired by the McGregor flap, differing from the other described techniques.
1. Instituto de Dermatologia Prof. Rubem David Azulay, Cirurgia Dermatológica, Rio
de Janeiro, Rio de Janeiro, Brazil
Corresponding author: Lissiê Lunardi Sbroglio Bastian Departamento de Cirurgia Dermatológica, Instituto de Dermatologia Professor Ruben David. Azulay. Rua Santa Luzia, 206, Centro, Rio de Janeiro, RJ, Brazil. Zip code: 20020-022 E-mail: lissiesbroglio@gmail.com













 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter