

Review Article - Year 2023 - Volume 38 -
Body Dysmorphic Disorder and the influence of the media in demand for plastic surgery: the importance of proper evaluation
O Transtorno Dismórfico Corporal e a influência da mídia na procura por cirurgia plástica: a importância da avaliação adequada
ABSTRACT
Introduction: Since the beginning, plastic surgery has improved self-esteem and acceptance in a society that idealizes the cult of the body. The pressure of consumption and the ease of undergoing plastic surgery becomes an obsession in these patients' lives.
Method: Female patients who underwent psychological evaluation and follow-up throughout the surgical and plastic surgery procedure, aged between 19 and 57, answered the Sociocultural Attitudes Questionnaire concerning appearance and the Body Dysmorphophobia Symptom Scale.
Results: Of the 38 patients evaluated, 17 have the media as an influence concerning their body image and have symptoms of Body Dysmorphic Disorder (BDD), 13 patients have the media as an influence on their body image, but they do not have BDD symptoms, and in eight patients the media does not influence their body image, and they do not have BDD symptoms.
Conclusion: The importance of a multidisciplinary team, with a psychologist, is highlighted to evaluate and monitor the patient throughout the surgical process, as the early diagnosis of BDD will avoid dissatisfaction with the result of the plastic surgery and, mainly, future court lawsuits.
Keywords: Body dysmorphic disorders; Reconstructive surgical procedures; Mass media; Health's judicialization; Obsessive-compulsive disorder
RESUMO
Introdução: Desde os primórdios, a cirurgia plástica melhora a autoestima e a aceitação em uma sociedade que idealiza o culto ao corpo. A pressão do consumo e a facilidade de se submeter a um procedimento de cirurgia plástica acabam tornando-se obsessão na vida desses pacientes.
Método: Pacientes do sexo feminino que passaram por avaliação e acompanhamento psicológico em todo o processo cirúrgico, e procedimento de cirurgia plástica, com a idade entre 19 e 57 anos, responderam ao questionário de Atitudes Socioculturais em relação a aparência e a Escala de Sintomas de Dismorfobia Corporal - Body Dysmorphic Scale.
Resultados: Dos 38 pacientes avaliados, 17 têm a mídia como influência em relação a sua imagem corporal e apresentam sintomas do Transtorno Dismórfico Corporal (TDC), 13 pacientes têm a mídia como influência em relação a sua imagem corporal, mas não apresentam sintomas do TDC, e em oito pacientes a mídia não influencia em relação a sua imagem corporal e não apresentam sintomas do TDC.
Conclusão: Destaca-se a importância de uma equipe multidisciplinar, com a presença de um psicólogo, para avaliar e acompanhar o paciente em todo processo cirúrgico, pois o diagnóstico precoce do TDC evitará uma insatisfação com o resultado da cirurgia plástica e, principalmente, futuros processos judiciais.
Palavras-chave: Transtornos dismórficos corporais; Procedimentos cirúrgicos reconstrutivos; Meios de comunicação de massa; Judicialização da saúde; Transtorno obsessivo-compulsivo
INTRODUCTION
“Currently, we live in an exaggerated litigation society, where even the small details of everyday life and common annoyances end up in front of a judge” (the numbers of judicialization in medicine)1.
We become people who are psychically weakened by society’s demands and run the risk of becoming spiritually and psychically ill.
According to a survey carried out in 2016 (ISAPS/ IBOPE), Brazil was the second country where the most cosmetic surgeries were performed, with 1.45 million in total. The United States led, with 1.48 million procedures, and Russia appeared in third place, with 579,000 surgeries2.
Since the beginning, plastic surgery has improved self-esteem and acceptance in a society that idealizes the cult of the body.
According to Lima et al.3, in the article “The ideology of the perfect female body. A question with the real”, “[...] the body is an object of private property in which the subject can do anything; however, capitalist society omits that ‘this can do anything’ is an illusion, as it imposes standards for the body ideal. Therefore, the subject is a mere executor of the norms of consumption in his own body [...]” (p. 50).
The pressure of consumption and the ease of undergoing plastic surgery becomes an obsession in these patients’ lives.
This enormous suffering increases when these standards are exposed at all times by the media as attainable, purchasable, and healthy, transforming bodies into true laboratories to achieve complete well-being and especially the solution to all problems in the lives of these people4.
The details of the human mind, such as personality disorders and image disorders, are decisive in the search for plastic surgery. If they are not correctly diagnosed, they cause future problems, such as dissatisfaction with results and lawsuits.
“The screening of psychological aspects in the selection phase is decisive for the success or failure of the aesthetic surgical procedure. That is, patients’ mental health interferes with the perception of surgery results” 5.
Evolution of the doctor-patient relationship
Camila Vasconcelos cites Foucault in her article “Medical responsibility and judicialization in the doctor-patient relationship” that: “[...] the power relationship is articulated to discourse, configuring an underlying dimension of communication between people. It is a relationship between power and knowledge inherent in the discourse itself, in which someone carrying the fact of knowledge – knowledge – elevates him to the condition of power in a given environment that recognizes him as such”6.
The relationship between service providers and their customers has ethical and unethical aspects.
For a professional in Plastic Surgery to carry out his work, 6 years of graduation in Medicine, 2 years of medical residency in General Surgery, and 3 years of medical residency in Plastic Surgery are required.
The professional without adequate training harms patients’ health, physical, and, mainly, mental well-being. Many carry out procedures outside the legislation.
On the other hand, the increase in the number of professionals, even qualified ones, puts pressure on relationships towards a purely mercantilist trajectory, ignoring the main thing, which is the patient’s emotions.
When looking for a plastic surgeon, the person has numerous questions, insecurities, and uncertainties. The professional present there is often fixated on the number of patients to be operated on, not on the service quality.
The doctor-patient relationship to provide humanized care is increasingly scarce in Plastic Surgery. This ends up becoming negative in all aspects, as there may be dissatisfaction on the part of the patient with the result of the surgery, and if he has a personality disorder that was not identified from the beginning in the preoperative consultations, this patient is a candidate to cause future problems for that professional.
According to Pellegrino (1993), quoted by Vasconcelos6, “The doctor’s knowledge, therefore, is not private property; it is not intended primarily for personal gain, prestige or power. Rather, the profession holds medical knowledge in trust for the patient’s good. By accepting the provenance of medical education, those who enter medicine become part of an alliance with the society that cannot be unilaterally dissolved. Medical students, from day one, enter a community bound by a moral pact. They accept the privileges of medical education in exchange for the physician’s knowledge management responsibility” 6.
Psychic disorders and the influence of the media and social networks
“Human beings traverse history in search of the fullness and perfection of the body. The actors change, the scenario changes, the sociocultural context, the tastes and interpretations, the meaning, and the search for the ideal body remains4.”
To what extent does undergo plastic surgery have its limitations? Due to the influence of the media, it ends up becoming an obsession in some people’s lives, wanting to “be” or look like a certain celebrity, such as famous actresses and actors, comic book characters, and dolls like Barbie and Ken.
Many of these images posted on social networks, which directly influence these people, undergo several modifications, not correspond to reality.
“The body is a living organism that has its own characteristics and with its own uniqueness. Performing cosmetic surgery means improving an imperfection and increasing the positive traits of each patient. Therefore, the final objective of the surgery is to seek a positive aesthetic improvement and never a transformation. A dysmorphic patient is a dissatisfied person constantly looking for a mutation, getting into a loop from which he will not easily get out. When the patient has dysmorphophobia, he usually complains of a spot that cannot be objectified and should be an alarm for the specialist visiting him” 7.
According to Pereira de Oliveira8, behind this great fantasy, there is mental suffering, often unconscious, unfortunately not diagnosed by the professional, due to not having sufficient preparation, or for not having an interdisciplinary team, or else that professional who does not follow ethical norms, performing the procedure on the patient.
The doctor-patient relationship is also an extremely important factor in managing these conditions.
Today, in the artistic world, we can encounter several celebrities with customs and habits that are not common in our daily lives, influencing people worldwide.
Anonymous people transformed themselves physically to become famous. Many do not know, but behind that exposed image, obsessive psychic factors transform the lives of these subjects.
Body Dysmorphic Disorder is one of the psychopathologies observed in these people. “The recently published World Health Organization International Classification of Diseases states that BDD is characterized by persistent preoccupation with one or more perceived defects or flaws in appearance that are unnoticeable or faintly noticeable to others. Individuals experience excessive self-consciousness, usually with ideas of reference (i.e., the conviction that people are noticing, judging, or talking about the perceived defect or flaw).”9.
The individual triggers an obsession, in which the imaginary defect migrates to various parts of his body. Undergoing an aesthetic surgical procedure will alleviate the psychic pain he feels. Mental pain will turn into bodily pleasure.
In an interview for Revista Quem10, Rodrigo Alves (36), the “human Ken,” reported that he started having aesthetic procedures because he felt ugly and excluded in childhood, with few friends. After the surgery and the apparent changes, people began to notice him: “Today I am the fruit of my imagination. I am everything I wanted to be in life.”
As a teenager, he had no friends; he felt insecure; he used to wear black clothes and sat in the background in the classroom. His colleagues called him a little potato and beat him. “It had nothing to do with my appearance; it was more with my psychology. I excluded myself”10.
Goulart11 mentions that the perception of the body as one’s own seems natural and intuitive; however, in reality, it is not quite like that: [...] “throughout life, the vision of the body will be marked not only by images but also by definitions (signifiers) and own sensations. So, we have a body that is apprehended by its imaginary aspect (appearing), by its symbolic aspect (being), and by its real aspect (body experience not imagined or symbolized by the subject and which emerges abruptly)”.
OBJECTIVE
In this study, we intend to evaluate how the media influences body standards in adopting behavior to modify the body, which can cause dissatisfaction and disappointment with the result, leading to lawsuits.
METHOD
The study consisted of 38 patients who underwent a plastic surgery procedure, all female (aged between 19 and 57 years).
All procedures were performed in different locations and by four different teams.
The patients underwent psychological assessment and follow-up throughout the surgical process and were invited to participate in the study, having received the Sociocultural Attitudes Questionnaire (SATAQ-3) concerning appearance and the Body Dysmorphophobia Symptom Scale - Body Dysmorphic Symptoms Scale.
The Questionnaire of Sociocultural Attitudes towards Appearance (SATAQ-3) is an instrument developed to assess sociocultural pressure and internalization of the standard of beauty. It is composed of 30 questions, with answers in the form of a Likert scale from 1 (totally disagree) to 5 (totally agree), intended to assess the influence of the media on the body. The sum of the responses calculates the final score, and the score proportionally represents the influence of sociocultural aspects on body image12.
The Body Dysmorphophobia Symptom Scale is designed to measure the symptoms of Body Dysmorphic Disorder (BDD) in individuals seeking plastic surgery who are preoccupied and distressed about their physical appearance. The scale consists of ten items that objectively and quickly identify BDD’s psychopathological characteristics in individuals concerned about their physical appearance and who seek plastic surgery. The final score corresponds to the sum of positive responses to all questions. Higher scores indicate the presence of BDD symptoms13.
RESULTS
Of the 38 patients evaluated, 17 (44.74%) have the media as an influence concerning their body image and have symptoms of BDD, 13 (34.21%) patients have the media as an influence on their body image, but do not have BDD symptoms, and in eight (21.05%) patients the media does not influence their body image, and they do not have BDD symptoms.
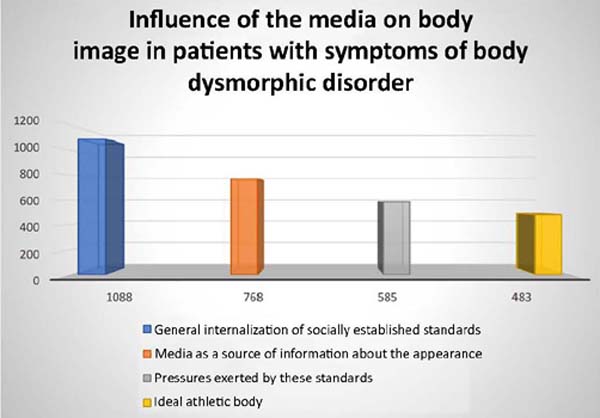
Tables 1 2 3 4 show the items that prevailed in evaluating the sum of the results of the four subscales of the SATAQ-3 questionnaire.
| Patients evaluating | scores |
|---|---|
| Media influences the patient’s body image (presents dysmorphophobia) | 323 |
| Media influences the patient’s body image (does not have dysmorphophobia) | 254 |
| Media does not influence the patient’s body image (does not have dysmorphophobia) | 191 |
| Total | 768 |
| Evaluated patients | scores |
|---|---|
| Media influences the patient’s body image (presents dysmorphophobia) | 197 |
| Media influences the patient’s body image (does not have dysmorphophobia) | 157 |
| Media does not influence the patient’s body image (does not have dysmorphophobia) | 129 |
| Total | 483 |
| Evaluated patients | Scores |
|---|---|
| Media influences the patient’s body image (presents dysmorphophobia) | 480 |
| Media influence on the patient’s body image (does not have dysmorphophobia) | 403 |
| Media does not influence the patient’s body image (does not have dysmorphophobia) | 205 |
| Total | 1088 |
| Evaluated patients | Scores |
|---|---|
| Media influences the patient’s body image (presents dysmorphophobia) | 274 |
| Media influences the patient’s body image (does not have dysmorphophobia) | 214 |
| Media does not influence the patient’s body image (does not have dysmorphophobia) | 97 |
| Total | 585 |
Figure 1 shows the subscales of the SATAQ-3 questionnaire that had the highest scores.
DISCUSSION
The results show that the media greatly influences people to opt for surgical and/or non-surgical correction, especially in patients with image disorders.
The “media” effect sometimes generates “surreal” expectations or even sublimation of results.
In cases of dysmorphia, the acceptance of the result obtained with the intervention will rarely be positive, which can lead to problems in the relationship with the doctor, becoming an endless “motus continuo”.
CONCLUSION
It is up to the plastic surgeon to explain the possibilities and their results, clearly and realistically, with details and risks associated with the surgery. No makeup to avoid future problems. The plastic surgeon should establish a good doctor-patient relationship, based on an attentive look, with sensitivity, acceptance, and care when relating to the patient. Based on ethical principles and moral conscience when dealing with the patient. They are inseparable factors in the interaction of this binomial that will result in professional success.
We cannot ignore that, aware of the professional and ethical commitment, the doctor, in addition to human solidarity, has an indispensable role in the political and social commitment inherent to the citizen in the transformation the now globalized world has undergone.
The Code of Medical Ethics brings the rules of conduct that physicians must practice and observe. Article 2nd, Chapter I, states that “the target of all physician attention is the human being, for whose benefit he must act with the utmost zeal and to the best of his professional capacity.” It is evident that the professional must have zeal, appreciation, respect for the human condition, and technical competence. Chapter V (Relationship with patients and family members) focuses on the principle of patient autonomy: priority of life over material and moral goods, responsibility in dealing with the patient, and respect for their vulnerability14.
Body Dysmorphic Disorder should no longer be neglected and should be identified; therefore, the psychologist must participate with the plastic surgeon in the diagnostic and therapeutic process. We know that surgical and plastic treatments seem ineffective in BDD and can pose risks to the physicians who perform them since patients can become aggressive and violent and generate litigation.
1. Hospital Ruben Berta, Cirurgia Plástica, São Paulo, São Paulo, Brazil
2. Hospital da Baleia, Belo Horizonte, Minas Gerais, Brazil
3. Fundação Hospitalar do Estado de Minas Gerais, Hospital João XXIII, Belo Horizonte,
Minas Gerais, Brazil
Corresponding author: Alexandre Kataoka Av. Paulista, 2494, cj 14, Bela Vista, São Paulo, S P, Brazil. Zip code: 01310-300 E-mail: drkataoka@hotmail.com








 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter