

Articles - Year 2004 - Volume 19 -
Hydroliposuction: 22 Years Experience with Tumescent Lipoplasty
Hidrolipoaspiração: 22 Anos de Experiência com Lipoplastia Intumescente
ABSTRACT
The author presents his experience with Hydroliposuction, a procedure developed in 1980 and 1981 as the first enhancement of the Illouz's technique. This study includes considerations on the history of liposuction; the natural evolution of Curettage and Suction Curette and, particularly, it addresses how this form of suction came about, after the use of tumescent hydration of the fat tissue to be suctioned. From the first steps in the suction of fat in 1980, when Ivez Illouz arrived to Brazil, invited by Vinicius Faria, the author found that it would be better to work with thin cannulas in an excessively hydrated region and has defended this method, which he regards as the safest in the technique of liposuction, intensely discussed in the first three years of lipoplasty in Brazil, in contrast with the dry technique, initiated in 1982, which defefended conducting the surgery without any previous hydration. The technique and its statistical results are presented.
Keywords: Liposuction; hydroliposuction; HL-suction; tumescent lipoplasty
RESUMO
O autor apresenta sua experiência com a Hidrolipoaspiraçâo, um procedimento desenvolvido em 1980 e 1981 como primeiro refinamento da técnica de Illouz. Tece considerações sobre a história da lipoaspiraçâo, evolução natural da Curetagem e Curetagem-Sucção e, em particular; de como chegou a essa forma de aspiração, precedida de hidratação intumescente do tecido gorduroso a ser aspirado. Desde seus primeiros passos na sucção de gorduras em 1980) quando Ivez Illouz chegou ao Brasil) convidado por Vinicius Faria) o autor determinou que seria melhor trabalhar com cânulas finas em uma região excessivamente hidratada e tem defindido este método) o qual considera o mais seguro na técnica de lipoaspiração, intensamente discutido ao longo dos três primeiros anos da lipoplastia no Brasil) em comparação com a técnica seca) surgida em 1982) que defindia a realização da cirurgia sem nenhuma hidratação prévia. Descreve a técnica e apresenta resultados estatísticos.
Palavras-chave: Lipoaspiração; hidrolipoaspiração; HL-sucção; lipoplastia intumescente
The precursor of today's "Lipoplasty" techniques was the "Curettage"(1-3) of fat also called "Lipexheresis" by Schrudde in 1972. Also called "Steatomeries" by Vilain(4), localized fat and lipodystrophies were being scraped with a curette by Fischer(5), when Kesselring(6), in 1978, began using suction with hollow curettes, which facilitated considerably the process called "Suction curettage" by Teimourian(7), in 1981.
Criticism to these processes was related to the curettes, because they caused vascular lesions, displacements and excessive injury to the conjunctive tissue, leading to frequent seromas, as well as to excessive fibrous nodes with retraction on the skin surface, causing irregularities.
Illouz called "Lipolysis" the technique he published in 1980(8), whose merit was to only use suction with cannulas with a single lateral orifice on the blunt end. Those cannulas were then still very thick, as their diameter ranged between 8 and 14 mm. In his technique, Illouz described the injection of a small amount of hypotonic saline solution (about 80 to 200 ml in the abdominal or trochanteric region, for example) with hyaluronidase starting suction after about 20 minutes, waiting for the permeability of the conjunctive tissue to increase.
Also in 1980, following what was described by Hackme(9), we started to perform "Lipolysis". We noticed, however, that the use of thick cannulas made the process unsafe, because of the suction of "blocks" of subcutaneous tissue that frequently blocked cannulas due to their very wide inner diameters, and therefore could easily cause excessive suction, like what happened in one of our first cases. Bearing in mind making surgeries safer, less traumatic and less worri-some for surgeons, we made a few changes which led us to the procedure called Hydroliposuction (HL-suction), a term we used for the first time in presentations in 1981 (10 and 11). We placed, in that manner, more importance on greater forced hydration and tumescence, which had not yet been used by Illouz.
We found in the in vivo histological examination of subcutaneous abdominal tissue during abdominoplasties with tumescent injection of several concentrations of hyaluronidase on the edges of the abdominal flaps before resection, that the enzyme, with a quantity 10 times greater than that used by Illouz, did not cause lipolysis, but rather an increase in the hydration speed of adipocytes. The highly hydrated adipocytes were "swollen" by the dilution of their cytoplasm, which made us decide for tumescence because it facilitated the use of thin cannulas.
Illouz, approved the procedure and called it "Hydroliposuction", and asked us for some slides for his presentations, after the panel in the 1983 Brazilian Congress in Brasilia, because at the time, he was teaching intensely and showing his technique in many countries.
The Significant changes we introduced were the following:
I. Excessive hydration.
II. Use of hyaluronidase as an important agent for the diffusion speed of the injected saline and proportionally up to 10 times more than in Illouz's solution, which, besides providing a more uniform and intense hydration of adipocytes, accounting for greater absorption of hemorrhagic transudate in the immediate postoperative period.
III. Suction immediately after hydration, without any waiting period.
IV. Use of quite thinner cannulas with several small orifices that due to tumescence, do not get blocked.
V. Drainage by continuous suction through the same surgical incision.
VI. Strong uniform and continuous compression, for 4 days, performed by a compressive dressing, covered by a girthe.
During the two first years we were encouraged by the satisfactory results attained by other pioneers who believed in these changes, like Dr. William Bonhotte, who performed neck and face liposuctions as early as 1981, and Dr. José Valdivia Murillo who performed suction of fat around gynecomastias.
In that initial phase, Hydroliposuction was criticized because it caused an effect, which is globally accepted today: tumescence. Still today, some surgeons believe that tumescent infiltration causes assessment difficulties and, for this reason, they choose its opposite, "Lipodissection" or the dry technique of Fournier and Otteni(12). In 1984, Assumption(13) mentioned the tumescent technique, wich he came to know through one of our papers (14) in 1982, but he chose the dry technique, because he thought it provided a better idea of how much suction was necessary.
At that time, we frequently defended Hydroliposuction(15-19), because the technique caused less bleeding, facilitated the introduction of cannulas and removed fat finely fragmented and diluted. We sent a Previous Note for publication in Plastic and Reconstructive Surgery in 1982, which, however was not published (Fig. 1), because the editor preferred to wait until the work was complete. The article was sent in April 1983, but, in spite of the commended results, was refused for publication due to flaws in the English and due to the lack of understanding of the refinements added to Illouz's technique.
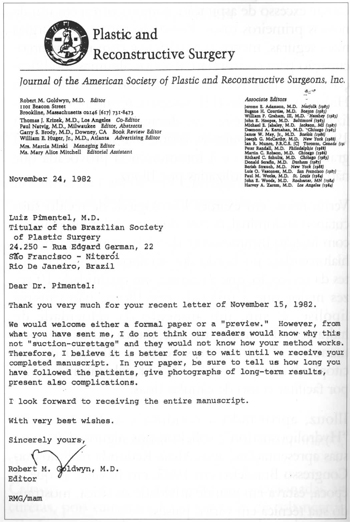
Fig. 1 - Reply letter from the editor of Plastic and Reconstructive Surgery (Nov/82).
In the same year in wich the American Lipolysis Society was founded, the journal published, in November, papers by Illouz(20), Teimourian(21), Fournier(22), and Kesselring(23) with interesting discussions by Grazer(24) and Reed(25).
Fournier believed the injection of liquid unnecessary and classified his Lipodissection as the "Dry Technique" and Lipolysis as the "Wet Technique". Grazer appointed the real pioneer of fat removal, Dr. Joseph Schrudde, with the use of curettage. He classified Kesselring's and Fisher's suction curettage as second generation and, Illouz's Lipolysis as third generation.
Dr. Grazer believed that the fourth generation would be the development of these techniques into reconstructive surgeries. Unfortunately Grazer did not know, as it had not been published then, that the fourth generation had already arrived in 1980, with the performance of liposuction with tumescence and that, in 1983, we were already doing reconstructions with suctioned fat grafts.
Reed, in his discussion, emphasized principles, which had always been important for us too, like the strict selection of patients, and performing the surgical procedure only for localized fat and in non flaccid skin with good elasticity.
TECHNIQUE
The technique is based on suction immediately after making each area tumescent (larger areas should be subdivided into smaller areas; abdomen, for example, may be divided into 2, 3 or 4). Each area is successively infiltrated before suction, because high concentrations of hyaluronidase lead to quick absorption of the liquid and reduction in the tumescence, if the procedure takes long. Cannulas should be long, so as to enable fewer incisions, and thin, with no more than 4 mm diameter; mey may be straight or curved to better adapt to anatomical contours.
Absorption is slower in lower limbs, quicker in me torso and more so in me upper limbs and head. For that reason, enzyme concentration in me solution used in me torso should be half of that used for me lower limbs; on the face, neck and upper limbs it should be half of that used on the torso.
FORMULA OF THE SOLUTION
Preparation: for each 1,000 ml of saline solution (SS) (0.9% NaCl) add 200 ml of bi-distilled water (BW) and hyaluronidase (HLD), depending on me body region, 10,000 UTR for the lower limbs, 5,000 UTR for me torso, and 2,500 UTR for me face, neck and upper limbs.
That is, 1 ml SS + 0.2 ml BW + 10 or 5 or 2.5 UTR HLD.
The use of vasoconstrictors is optional, at me maximum proportion of 0.5 ml for every 1,000 ml of solution. It also is possible to add local anesthetic, if so desired.
INJECTION
In our practice twenty years ago, we used to use syringes or infusion devices.
Since 1983, we have been infiltrating by gravity, keeping the saline solution bottle at the height of 2.5 m and interconnecting two infusion sets to the level of me needle or infiltration cannula (Fig. 2a - Bonhötte Manouver), that should make slow introductions to several depths until the region becomes tense and distended, with no concern with me amount of liquid. The needle should be long enough to reach me entire area through the same incision made for suction (Fig. 2b).
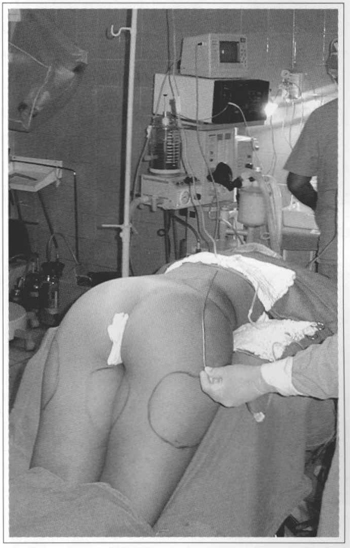
Fig. 2a - Infiltration by gravity. Flask with solution at 2.5 m height, interconnected by two infusion sets to a needle or cannula hydrating waist and hip.
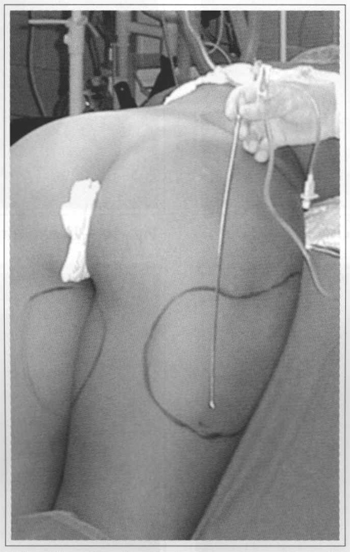
Fig. 2b - 2.5 mm long multi-perforated needle that will be introduced through the surgical incision in order to infiltrate the trochanteric region and hip.
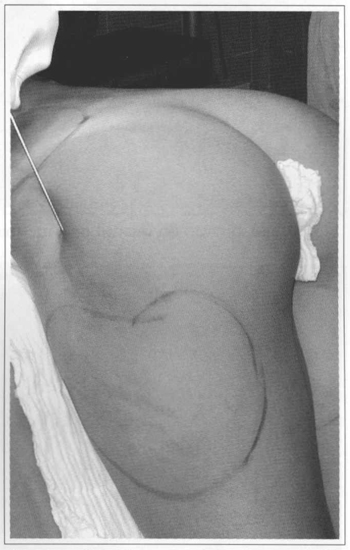
Fig. 2c - Right trochanteric region being infiltrated.
SUCTION
Suction is performed with a liposuction device or with syringes, using 4 mm or thinner cannulas, with several small diameter orifices, usually introduced through a single incision, whenever possible. Cannulas should be long to allow for the suction of the entire area, preferably longitudinally to me body, because we see fewer undulations on me skin with a longitudinal suction. For mis reason, the suction of the whole abdomen is performed wough two incisions in me pubic region. The same principle applies to limbs. However, when necessary, we also work transversally to remove more fat, as is customary with the thorax.
Para a trochanteric region, me patient is placed, part of me time or all me time, in me knee-chest position for better assessment of uniform removal, and suction is done through an incision between this region and me hip (Fig. 3a), whose suction is also performed wough me same incision (Fig. 3b).
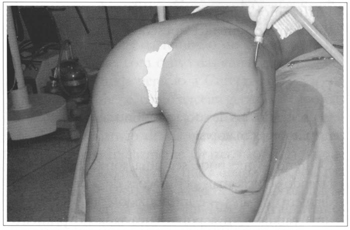
Fig. 3a - Suction of the trochanteric region in the knee-chest position, initiated by the borders of the delimited area.
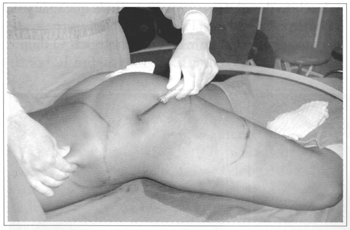
Fig. 3b - Suction of the hip through the same incision.
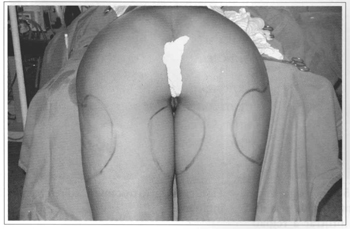
Fig. 3c - View of both trochanteric regions after a HL-suction.
We move the cannulas slowly, to several depths and vary the position of orifices, including upwards, avoiding me subdermal plane in me abdomen, hip, trochanteric region, and thighs. We use superficial planes, including me subdermal, on me face, neck, thorax, arms and legs.
DRAINAGE
The continuous use of suction drains is indispensable for large areas.
The drain - which can be a Levine 12 probe, with more wholes in it, according to the diameter of the area - is introduced with the help of a cannula with its tip fitting the first orifice of the drain, through the incision itself, and placed on the center or on the side of greater declivity in relation to the supine position. The cannula that comes off from the drain is rotated and removed (Figs. 4a and 4b). The drain is fixed with a skin suture and with surgical tape. The drain can be removed between 12 and 24 hours. In 12 hours, it drains about 80 to 90% of the total serosanguineous liguid, reaching the high totals of 300 to 400 ml in the larger areas, such as the trochanteric or abdominal region. We do not usually drain small areas. Sometimes, we use a ingle drain for two wide regions, like the gluteus and hips (Fig. 4c).
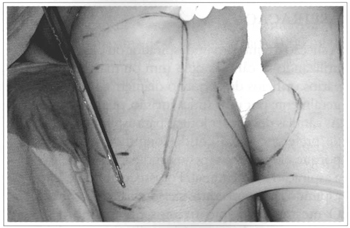
Fig. 4a - Multi-perforated drain and a 3.5 mm cannula for introducing it.

Fig. 4b - Drain introduced through the whole extent of the area.
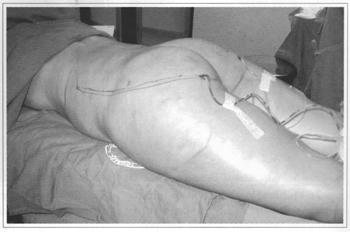
Fig. 4c - Drain reaching gluteus, hip and waist regions in another patient.
DRESSING
Compressive, modeling and adhesive dressing is as important as drainage. It should be made with elastic adhesive bandages (Leukoband, Tensoplast or Elastoplast), keeping continuous compression for 3 or 4 days (Fig. 5). After the removal of drains, patients are discharged with a compressive girdle over the bandage. The girdle should be used for 2 to 4 weeks more after bandages are removed. Our patients tolerate the initial compression days with the adhesive band well. It should be removed dry, without the use of solvents like ether or benzene, because they react with the gum, causing urticaria-like manifestations in some patients.
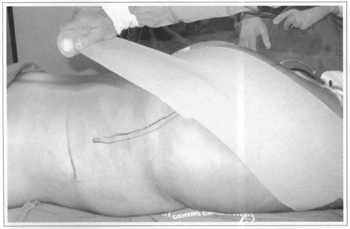
Fig. 5a - Beginning of dressing, contouring and compressing.

Fig. 5b - Completed dressing.
RESULTS
Along these 22 years, 2,317 patients have undergone Hydroliposuction. This number does not include suctions made in adjacent areas to improve the results of conventional surgeries. Trochanteric regions were the most freguent areas submitted to suction (42%), but usually associated to the suction of hips or abdomen or both.
There were very few ecchymoses, wluch only occurred in areas not drained, or in which there was some type of blocking, or when air entered the drain. Most patients were very satisfied because they did not have ecchymoses (Figs. 6, 7 and 8). Other results are shown in figures 9 and 10.
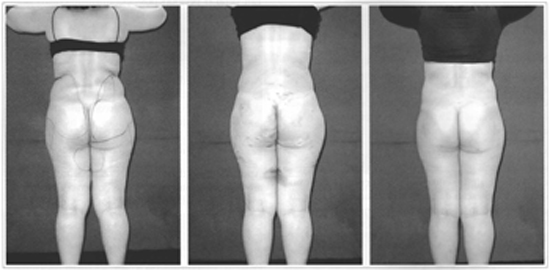
Figs. 6a-c - Minimum ecchymoses. Same 27 year-old patient of figures 4 and 5, with hip suction, gluteotrochanteric regions and internal surface of the thighs. Pictures from the preoperative, 4th day and 5th postoperative month in a dorsal view. In 6b, after removal of dressing, note rests of adhesive glue on the skin and smal ecchymoses in the non-drained area of the internal surface of the thighs.
Figs. 6d-f - Preoperative, 4th day and 5th postoperative month in a left lateral view. Note small ecchymoses on the base of the trochanteric region that was not drained on purpose.
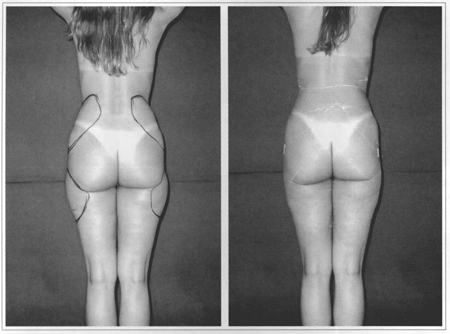
Figs. 7a & 7b - Absence of ecchymoses. 32 year-old patient in a dorsal view in the preoperative and 4th postoperative day of HL-suction of the hip and trochanteric regions. Note signs of adhesive and absence of ecchymoses.
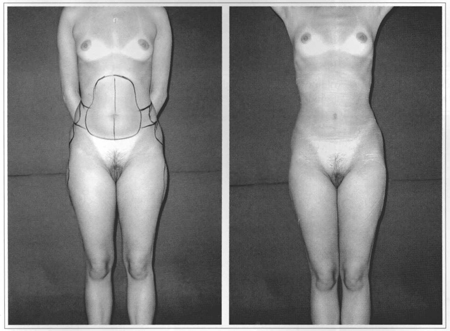
Figs. 7c & 7d - Front view of preoperative and 4th postoperative day of HL-suction in abdomen, hip and culottes. Without ecchymoses.
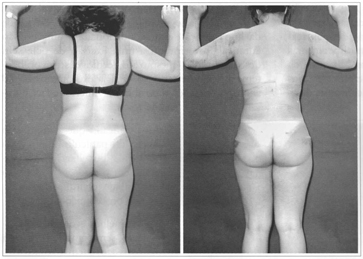
Figs. 8a & 8b - 28 year-old patient in a dorsal view in the preoperative and immediate (4th day) postoperative of HL-suction in arms, thoracic back, hip and waist. Note signs of adhesive and minimal ecchmoses in non-drained area of the left arm it and below the left hip.
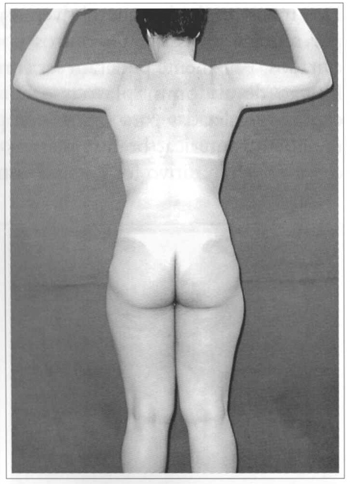
Fig. 8c - 1st postoperative year.

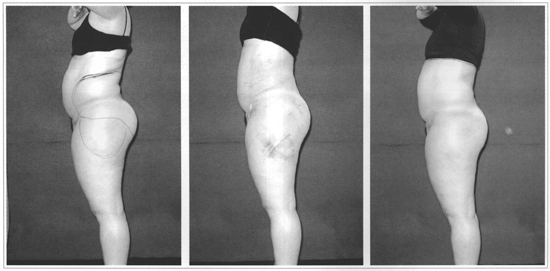
Figs. 9a-d - 35 year-old patient with flaccid skin and large-volume thighs and gluteus. Dorsal view of the preoperative and 6th postoperative month. Note undulations on the bases of the gluteus and thighs and their persistence, and the emergence of other milder ones, laterally, by skin accommodation.
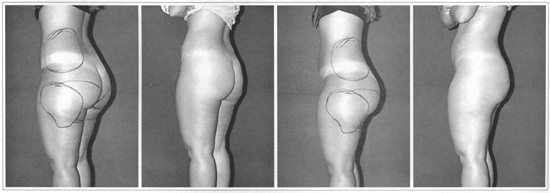
Figs. 9e-h - Oblique view of the preoperative and 6th postoperative month.
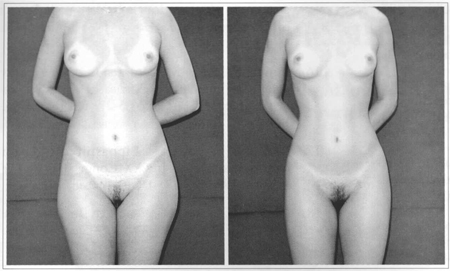
Figs. 10a & 10b - 24 year-old patient, with tense skin and small volumes in hip and trochanteric regions. Frontal view of the preoperative and 6th postoperative month.
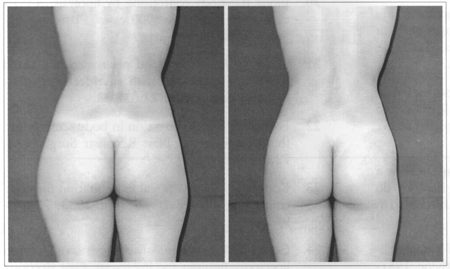
Figs. 10c & 10d - Dorsal view of preoperative and 6th postoperative month.
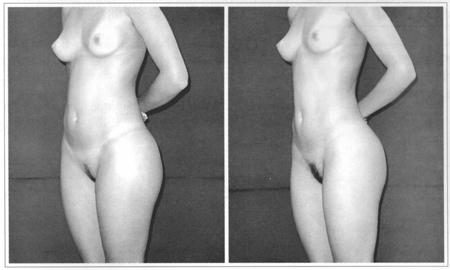
Figs. 10e & 10f - Oblique view of preoperative and 6th postoperative month.
There have never been any cases of systemic complications or any cases of important local complications, such as hematoma, infection or seroma, and our patients have never needed transfusion or correction of electrolytes. The largest suction volume was 4 liters in a 92-kg patient, but we have rarely removed more than 2.5 to 3 liters. Some sparse minor complications were observed in the scarring of incisions (57 cases), such as late scarring due to suffering of borders, certainly caused by burning resulting from the friction of cannulas, leading to hypertrophic scars or retractions that were easily corrected. This began to be avoided, by making slightly larger incisions to avoid friction, and whenever necessary, by a small resection on burned borders.
In general, the immediate postoperative period of these patients went well, despite occasional complaints of low intensity pain in some areas, always related to the drain and easily solved with analgesics during hospitalization.
After drain removal, there were no more complaints of pain, although the regions operated on remained tender upon touch. Analgesics were unnecessary after discharge. For all cases, we prescribed antibiotics for a week and loratadine to avoid itching while using the adhesive band.
After the fourth day, we allowed patients to resume their routine activities. Tenderness of the regions operated was enough to limits exercises.
There were 21 cases (0.90 %) of unsatisfactory results. One (01) case, in 1981, in which excessive suction was done in the internal surface of the thigh, utilizing thick cannulas (9 mm). Five (05) patients in which abdominal suction was below desirable in order to try to avoid undulations and a cellulite aspect (orange peel) remained, an effect that can occur even when there is small skin excess after pregnancy. Ten (10) patients over 40 years of age, in whom surgery was performed in large-volume saddlebags, presented a skin fold in the aspirated region. There were three (03) cases of cervical folding and two (02) of folds in the internal-posterior surface of the arms.
We considered 75% of results adequate and that 24% resulted in partial satisfaction to surgeon and patients.
DISCUSSION
Since me beginning of our work with liposuction we have defended that the fat suction process should be used with strict selection criteria so that surgeries were not indicated in those cases in which results may be unfavorable.
Of all our unsatisfactory results, only one was due to excessive removal. The remainder could have been avoided. Fortunately all of them could be corrected by abdominoplasties and elliptical dermolipectomies, performed for removing me central fold of the trochanteric region, brachioplasties and cervical rhytidoplasties. A positive conclusion was mat once real cutaneous excess is diagnosed, and is impossible to be reabsorbed, me patient should be warned of the possibility of me liposuction being conditioned to a posterior skin excision or a skin excision without detachment in the same procedure, a technique brilliandy described by Avelar(26), that we have been performing for 20 years, although only in the lower abdomen and internal surface of the thighs.
Instead of making it difficult, we have verified that excessive hydration of the fat pad makes suction easier wimout impairing the evaluation of quantity. Therefore, we have continued to perform me procedure.
In order to attain better postoperative development, without complications, ecchymoses, or pronounced edemas, and result in minimal discomfort, we have valued me utilization of the described amounts of enzyme, drainage and continuous and uniform compression for 4 days.
We are against excessive removal or utilization of large cannulas because they may produce true lipectomies, causing conjunctive extraction of me subcutaneous tissue, then fibroses and retractions, and then these problems can only be solved with physiotherapy. We defend an almost exclusive fat-cell liposuction with maximum preservation of me conjunctive mesh in which me fat pad remains between me skin and me aponeurosis and there are no palpable fibrous nodules.
We believe, however, in me efficacy of physiotherapy mat helps solve edemas and comforts the patient, and in physical exercise programs to stimulate muscular tonus and skin retraction.
CONCLUSIONS
We conclude that the method herein presented-which we have been using since 1980-can be done without evaluation errors that may be attributed to the large liquid injection. It is the first refinement of the Illouz technique.
Tumescent liposuction is very well known, since me publication of Klein(27), but it actually began to be performed in Brazil in 1980, with the name of Hydroliposuction, and in me beginning mere were more chances of errors, until its principles were well established.
We believe that it is better to perform a more laborious technique and with some initial discomfort to the patient, due to drains and adhesive compressive dressing, to attain less blood loss, less edema, no large ecchymoses and better initial results.
Good or bad results, with the technique, depend on me criteria for evaluating the relation between me contingent (skin) and the content (fat) to determine when and how much to aspirate.
It is a technique that has proven to be safe, which is similarly utilized to obtain fat cells for transplants and, due to me induced tunlescence, it is indispensable for performing the methods mat emerged afterwards, such as ultra-sonic liposuction, for example.
REFERENCES
1. Schrudde J. Lipexheresia for the correction of local adiposity. Abstract book, First Congress of the Intern Soc of Aesth and Plast Surg; 1972 Feb 6-11; Rio de Janeiro, Brasil.
2. Schrudde J. Lipexhaerese zur beseitigung der lokalen adipositas. Plastiche chirurgie des kopf - und halsbereichs und der weiblichen brust. 1975; Stuttgart, Thieme.
3. Schrudde J. Lipekrornie und lipexhaerese im bereich unter en extremitaten. Langenbecks, Arch Chir. 1977; 345:127.
4. Vilain RC. Surgical correction of steatomeries. Clin Plast Surg. 1975; 2: 467.
5. Fischer A. Revised technique for cellulites fato Reduction in riding breeches deformity. Bull Int Acad Cosm Surg. Dec. 1977; 2:4.
6. Kesselring UK, Meyer R. Suction curette for removal of excessive local deposits of subcutaneous fato Plast Reconstr Surg. 1978; 62:305.
7. Teimourian B, Fisher JB. Suction curettage to remove excess fat for body contouring. Plast Reconstr Surg. July 1981; 68(1):50-8.
8. Illouz YG. Une nouvelle technique pour les lipo-dystrophies localisées. Rev de Chir Esthet de Lang Franç. 1980; 19:3-10.
9. Hackme F. Historical evolution of liposuction in Brazil. In: Avelar J. Abdomino-plasty without panniculus undermining and resection. 1. ed. São Paulo: Hipocrates; 2002. p. 337-59.
10. Pimentel LAS. Correção das lipodistrofias localizadas pela lipoaspiração. In: II Jorn Carioca de Cir Estética; 1981 Ago 6-8; Rio de Janeiro, Brasil.
11. Pimentel LAS. Lipectomia por aspiração - a hidrolipoaspiração. In: Centro de Estudos do Hospital dos Estivadores de Santos; 1981 Set 10; Santos, Brasil.
12. Fournier PF, Otteni E Treatment of localized lipodystrophies by aspiration. Chir Esthetic, 1981- 1982; 59-78.
13. Assumpção EA. Lipoaspiração no tratamento das adiposidades localizadas. A F Méd. 1984; 88(3):79-86.
14. Pimentel LAS. Hidrolipoaspiração gluteotrocantérica. In: XIX Congr Bras de Cir Plástica. 1982 Out 31-Nov 5; Recife, Brasil.
15. Pimentel LAS. Lipoaspiração - princípios anatomofisiológicos. In: Curso de Lipodistrofias, SBCP. Regional Minas Gerais. 1983 Abril 8; Belo Horizonte, Brasil.
16. Pimentel LAS. Lipoaspiração. In: Recentes Aquisições em Cirurgia Plástica. IV Jorn Carioca de Cir Estética. 1983 Ago 25-27; Rio de Janeiro, Brasil.
17. Pimentel LAS. Lipoaspiração ou hidrolipoaspiração? In: XX Congr Bras de Cir Plástica. 1983 Nov 27-Dez 2; Brasília, Brasil.
18. Pimentel LAS. Hydroliposuction. In: XX Congr Bras de Cir Plástica. 1983 Nov 27-Dez 2; Brasília, Brasil.
19. Pimentel LAS. Suction-curettage or hydroliposuction? In: XX Congr Bras. de Ciro Plástica. 1983 Nov 27-Dez 2; Brasília, Brasil.
20. Illouz IG. Body contouring by lipolysis: 5-years experience with over 3000 cases. Plast Reconstr Surg. 1983; 72:591-7.
21. Teimourian B. Face and neck suction-assisted lipectomy associated with rhytidectomy. Plast Reconstr Surg. 1983; 72:627-33.
22. Fournier PE. Lipodissection in body sculpturing: the dry procedure. Plast Reconstr Surg. 1983; 72:598-609.
23. Kesselring UK. Regional fat aspiration for body contouring. Plast Reconstr Surg. 1983; 72:610- 9.
24. Grazer FM. Suction-assisted lipectomy, suction lipectomy, lipolysis and lipexeresis. Plast Reconstr Surg. 1983; 72:620-3.
25. Reed LS. Some thoughts on suction-assisted lipec-tomy Plast Reconstr Surg. 1983; 72:624-6.
26. Avelar JM. Avelar. Abdominoplasty without pan-niculus undermining and resection. 1. ed. São Paulo: Hipocrates; 2002.
27. Klein JA. The tumescent technique for liposuction surgery Am J Cosmet Surg. 1987; 4: 263.
I - Senior Member of the Sociedade Brasileira de Cirurgia Plástica
Address for correspondence:
Luiz Alberto Soares Pimentel, MD
R. Nilo Peçanha 59, Ingá
24210-480 - Niteroi - RJ Brazil


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter