

Case Report - Year 2022 - Volume 37 -
Management of complex scalp defects after excision of malignant tumors
Manejo de defeitos complexos do couro cabeludo após excisão de tumores malignos
ABSTRACT
Introduction: Scalp reconstruction after cancer resection remains a challenge for surgeons, especially considering the increasing incidence of skin cancer among elderly patients. Dermal matrix (DM) is a heterogeneous group of wound covering materials that aid in wound closure and replace some of the skins functions, either temporarily or permanently. Patients at higher surgical risk can benefit from the use of DM, which help to generate a new dermis, offering great improvements in coverage of complex and extensive defects
Methods: It is a retrospective study with analysis of medical records and report of two cases of patients at the A.C.Camargo Cancer Center-SP, Brazil.
Results: We report two cases of complex and extensive scalp defects at a single center using DM associated with skin grafting and negative pressure therapy (NPT) in reconstructive surgery after resection of malignant skin neoplasm with satisfactory functional and esthetic results.
Conclusions: Extensive lesions of the scalp are a challenge in clinical practice and a multidisciplinary treatment is essential. The results obtained indicate that DM associated with partial skin grafting and NPT have enormous potential to increase the therapeutic options available to the surgeon and possibly benefit patients, especially those who do not have the clinical conditions for extensive coverage surgery with microsurgical flap.
Keywords: Skin, artificial; Wound healing; Negative-pressure wound therapy; Scalp; Skin neoplasms.
RESUMO
Introdução: A reconstrução do couro cabeludo após a ressecção oncológica continua sendo um desafio para o cirurgião, especialmente considerando a incidência crescente de câncer de pele entre pacientes idosos. A matriz dérmica (MD) é um grupo heterogêneo de materiais de cobertura de feridas que auxiliam no fechamento da ferida e substituem algumas das funções da pele, temporária ou permanentemente. Pacientes com maior risco cirúrgico podem se beneficiar do uso de MD, que ajuda a gerar uma nova derme, oferecendo grandes melhorias na cobertura de defeitos complexos e extensos.
Métodos: É um trabalho retrospectivo com análise de prontuário e relato de dois casos de pacientes do A.C.Camargo Cancer Center-SP, Brasil.
Resultados: Relatamos dois casos de defeitos complexos e extensos de couro cabeludo em um centro único usando MD associada a enxerto cutâneo e terapia de pressão negativa (TPN) na cirurgia reconstrutiva após ressecção de neoplasia maligna da pele com resultados funcionais e estético satisfatório.
Conclusões: As lesões extensas do couro cabeludo são um desafio na prática clínica e um tratamento multidisciplinar é fundamental. Os resultados obtidos indicam que a MD associada com a enxertia de pele parcial e com a TPN tem enorme potencial para aumentar as opções terapêuticas disponíveis para o cirurgião e possivelmente beneficiando os pacientes, especialmente aqueles que não têm condições clínicas para uma cirurgia extensa de cobertura com retalho microcirúrgico.
Palavras-chave: Pele artificial; Cicatrização; Tratamento de ferimentos com pressão negativa; Couro cabeludo; Neoplasias cutâneas.
INTRODUCTION
Scalp reconstruction after oncological resection remains a challenge for the surgeon, especially considering the increasing incidence of skin cancer among elderly patients. Scalp reconstruction can be challenging due to local aggressiveness, with the invasion of adjacent structures, the extension of resection, the possibility of tumor recurrence and the need for adjuvant radiotherapy1.
Treatment options after tumor resection are skin grafting, pedicled and axial local flaps, or microsurgical flaps to correct complex and extensive wounds2. Skin grafting can be very interesting in large resections, but skin grafts cannot be used whenever bones, nerves and tendons are exposed. Skin flaps are good options for reconstruction, but the defect size limits them. Dermal matrix (DM) has been used in treating burns in the acute phase and the management of sequelae and reconstructive surgery for many years3.
DM is a heterogeneous group of wound dressing materials that aid in wound closure and replace some of the skin’s functions, temporarily or permanently, depending on the product’s characteristics. They provide various biological and physiological properties of the human dermis that allow and/or promote new tissue growth and optimize conditions for healing4. Patients with a higher surgical risk can benefit from using DM, which helps generate a new dermis, offering great improvements in the coverage of complex and extensive defects5. This study aims to report two complex cases of extensive lesions on the scalp, with complete closure of the lesion.
CASE REPORT
This study is a case report of two patients authorized by the institutional ethics committee, No. RC 103/21. A 74-year-old male patient was diagnosed with extensive sarcomatoid carcinoma affecting the bilateral parietal region, measuring 12x9cm in diameter. He had his first surgery at another hospital, with a history of 3 previous resections. He was referred to us because he had tumor recurrence after the last resection. The patient had multiple comorbidities. The case was taken to the Tumor Board, with the multidisciplinary team, being discussed between radiotherapy or surgical resection, opting for resection of the lesion, as radiotherapy would entail a high risk of exposure of the skull and evolution to fulminant meningitis.
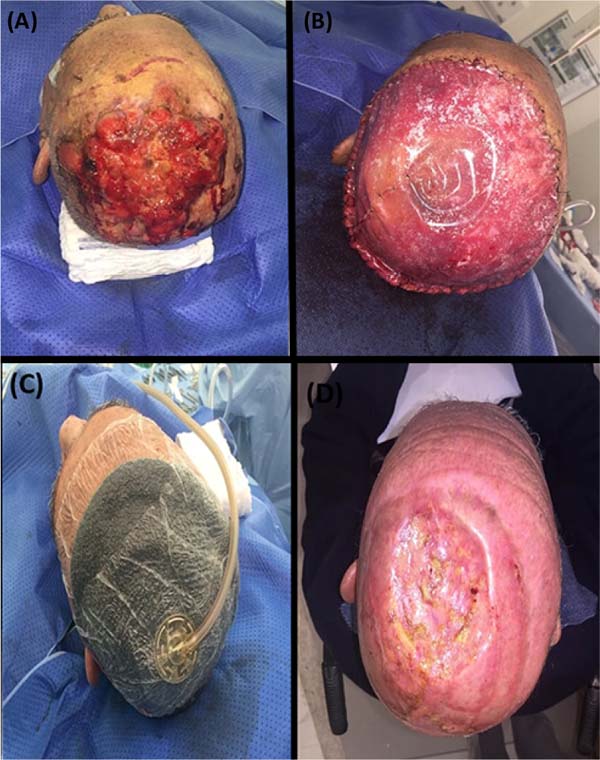
A wide local excision was performed, together with the neurosurgery team that drilled the bone, removing the entire area of the cranial vertex (with a diameter of 8cm). DM was put in place with a size of 20 x 30 cm. A negative pressure therapy (NPT) dressing was applied to cover the DM and was removed 14 days after surgery. There was good integration of DM. For partial-thickness skin grafting, a new surgical procedure was performed (2 months after the first procedure). The skin graft wound was covered with NPT for 7 days. Outpatient follow-up was maintained for at least 1 year after the initial surgical procedure, with no signs of recurrence (Figure 1).
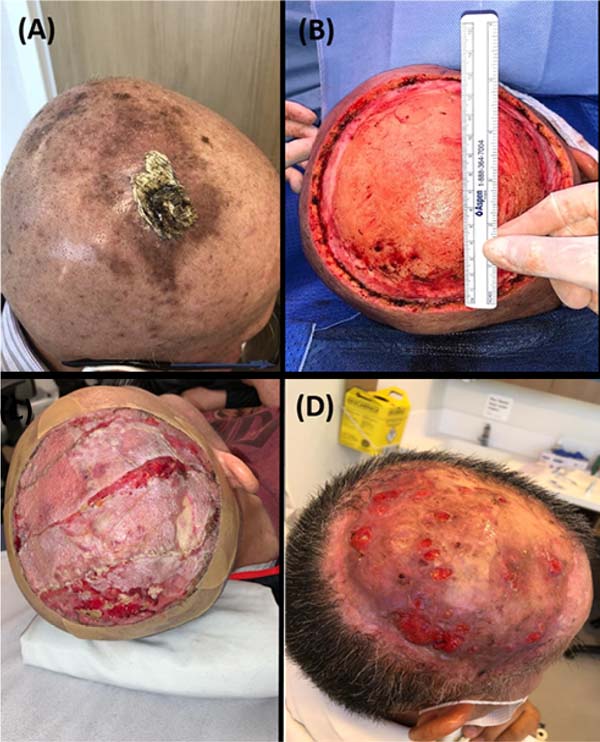
We report another case of a male patient, 64 years old, with a lesion on the scalp, in the right parietal region, measuring 8x5cm in diameter, with the diagnosis of angiosarcoma. He had systemic arterial hypertension and dyslipidemia as comorbidities. He presented an injury without bone involvement of the cranial vault. Cervical lymph node enlargement was identified, and FNAB (fine needle aspiration) was inconclusive. The case was discussed at a Tumor Board meeting, with neoadjuvant chemotherapy indicated (due to the speed of tumor growth and probable neck metastasis), followed by surgical excision and adjuvant radiotherapy. Surgical resection, bone drilling, DM fixation and coverage with NPT dressing were performed. One month after the operation, partial-thickness skin grafting and NPT were performed. The dressing was removed on the seventh postoperative day. The patient evolved with tumor recurrence in some areas of the scalp; resection of recurrences was performed with primary closure and subsequently referred to radiotherapy. The patient followed the scalp radiotherapy treatment with total occlusion of all skin wounds (Figure 2).
DISCUSSION
Reconstruction of scalp defects after resectioning malignant tumors represents a considerable challenge that requires experience and good surgical judgment. Scalp defect repair should provide mechanical protection and an aesthetically acceptable appearance and facilitate a quick return to social life6.
DM is an alternative for treating complex wounds, as it allows its closure with less morbidity and surgical time. It is also a simple procedure compared to the microsurgical flap and can be performed in irradiated areas, allowing coverage of the wound in complex resections, better local control of the disease and early detection of recurrence2. In the reported cases, single-layer DM was used.
When DM is used with a partial skin graft, the resulting skin has less hypertrophic scar formation and contractures and is of better quality, thickness and flexibility than reconstructions using a partial-thickness skin graft alone1,4.
NPT can help remove deleterious substances from the wound, relieve edema, and stimulate cell proliferation, thereby promoting granulation and inhibiting chronic inflammation. In addition, NPT also appears to aid in the neovascularization of skin grafts and DM and may improve the success rate of the skin graft by strengthening the union between the skin graft and the recipient area. At the same time, the advent of a portable device allows patients to move earlier and accelerate their return to social life7.
CONCLUSION
Extensive scalp lesions are challenging in clinical practice, and multidisciplinary treatment is essential. The presence of a nursing team that is used to dressing changes in NPT and DM management is a cornerstone of the entire treatment. The results indicate that DM associated with partial skin grafting and NPT has enormous potential to increase the therapeutic options available to the surgeon and possibly benefit patients.
REFERENCES
1. Komorowska-Timek E, Gabriel A, Bennett DC, Miles D, Garberoglio C, Cheng C, Gupta S. Artificial dermis as an alternative for coverage of complex scalp defects following excision of malignant tumors. Plast Reconstr Surg. 2005;115(4):1010-7.
2. Campagnari M, Jafelicci AS, Carneiro HA, Brechtbühl ER, Bertolli E, Duprat Neto JP. Dermal Substitutes Use in Reconstructive Surgery for Skin Tumors: A Single-Center Experience. Int J Surg Oncol. 2017;2017:9805980.
3. Bertolli E, Campagnari M, Molina AS, Macedo MP, Pinto CA, Cunha IW, et al. Artificial dermis (Matriderm®) followed by skin graft as an option in dermatofibrosarcoma protuberans with complete circumferential and peripheral deep margin assessment. Int Wound J. 2015;12(5):545-7.
4. Rehim SA, Singhal M, Chung KC. Dermal skin substitutes for upper limb reconstruction: Current status, indications, and contraindications. Hand Clin. 2014;30(2):239-52.
5. Magnoni C, De Santis G, Fraccalvieri M, Bellini P, Portincasa A, Giacomelli L, et al. Integra in Scalp Reconstruction After Tumor Excision: Recommendations From a Multidisciplinary Advisory Board. J Craniofac Surg. 2019;30(8):2416-20.
6. Gurtner GC, Evans GR. Advances in head and neck reconstruction. Plast Reconstr Surg. 2000;106(3):672-82.
7. Zhang C, Liu D, Liang Z, Liu F, Lin H, Guo Z. Repair of refractory wounds through grafting of artificial dermis and autologous epidermis aided by vacuum-assisted closure. Aesthetic Plast Surg. 2014;38(4):727-32.
1. ACCamargo Cancer Center, Cirurgia plástica, São Paulo, SP, Brazil
2. ACCamargo Cancer Center, Departamento de Câncer de Pele, São Paulo, SP, Brazil
3. ACCamargo Cancer Center, Ambulatório de curativo- Enfermagem, São Paulo, SP, Brazil
ACVGO Analysis and/or data interpretation, Conception and design study, Conceptualization, Final manuscript approval, Methodology.
IDSF Analysis and/or data interpretation, Conceptualization, Final manuscript approval, Project Administration, Supervision, Writing - Review & Editing.
MC Final manuscript approval, Validation.
MML Final manuscript approval, Validation.
EB Final manuscript approval, Validation.
RON Final manuscript approval, Investigation, Validation.
Corresponding author: Ana Carolina V.G. Otsuka Av. da Aclimação, 314, São Paulo, SP, Brazil. Zip Code: 01531-000, E-mail: ac.otsuka@gmail.com
Article received: August 30, 2021.
Article accepted: April 7, 2022.
Conflicts of interest: none.





 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter