

Original Article - Year 2022 - Volume 37 -
Clinical-epidemiological profile of chemical burns in a Burn Therapy Unit (BTU) in Brazil
Perfil clínico-epidemiológico de queimaduras químicas em uma Unidade de Terapia de Queimados no Brasil
ABSTRACT
Introduction: Chemicals have a relatively low prevalence among the causes of burns. However, they are important because most accidents occur in the scope of work and in an economically active population. The objective is to perform an analysis of the profile of patients hospitalized for chemical burns in a Burn Unit.
Methods: Retrospective analysis of patients hospitalized in the Burn Unit of the State Hospital of Bauru, Bauru, SP, Brazil, between 2008 and 2018. Multiple variables were analyzed, such as age, gender, chemical agent, place where the accident occurred, need for ICU stay and days of hospitalization.
Results: In total, 40 (1.7%) patients were hospitalized due to chemical burn. The mean age was 35 years, with predominance of males, with 30 (75%) individuals. The main site of trauma was in the workplace, in 20 cases (50%). Based accidents were responsible for 20 (50%) admissions. The mean burned body surface was 7.5%. Eye burn occurred in 11 (27.5%) patients. Intensive care bed was required for 10 (25%) cases. When comparing accidents between acid iced substances and bases, we noted a difference in the number of ICU patients, with eight patients in lesions involving bases and two with acids (p=0.04).
Conclusion: The sample and results presented in this article are similar to the world literature on the subject. We evidenced the importance of this burn in the work environment and the involvement of individuals of active age, as well as the greater severity of accidents with chemical substance.
Keywords: Burns; Burns, chemical; Burn units; Epidemiology; Brazil.
RESUMO
Introdução: Substâncias químicas apresentam uma prevalência relativamente baixa dentre as causas de queimaduras. Porém, têm importância, pois a maioria dos acidentes ocorrem no âmbito do trabalho e em população economicamente ativa. O objetivo é realizar uma análise do perfil dos pacientes internados por queimaduras químicas em uma Unidade de Queimados.
Métodos: Análise retrospectiva de pacientes internados na Unidade de Queimados do Hospital Estadual de Bauru, Bauru, SP, Brasil, entre os anos de 2008 e 2018. Múltiplas variáveis foram analisadas, como idade, sexo, agente químico, local onde ocorreu o acidente, necessidade de internação em UTI e dias de hospitalização.
Resultados: No total, 40 (1,7%) pacientes foram internados devido a queimadura química. A média de idade foi de 35 anos, com predominância do sexo masculino, com 30 (75%) indivíduos. O principal local do trauma foi no ambiente de trabalho, em 20 casos (50%). Acidentes com base foram responsáveis por 20 (50%) internações. A superfície corporal queimada média foi de 7,5%. Queimadura ocular ocorreu em 11 (27,5%) pacientes. Leito de terapia intensiva foi necessário para 10 (25%) casos. Quando comparados os acidentes entre substâncias ácidas e bases, evidenciamos diferença no número de pacientes internados em UTI, com oito pacientes em lesões envolvendo bases e dois com ácidos (p=0,04).
Conclusão: A casuística e resultados apresentados neste artigo são semelhantes à literatura mundial sobre o assunto. Evidenciamos a importância dessa queimadura no ambiente de trabalho e o acometimento de indivíduos em idade ativa, assim como a maior gravidade de acidentes com substância química.
Palavras-chave: Queimaduras; Queimaduras químicas; Unidades de queimados; Epidemiologia; Brasil.
INTRODUCTION
Burns are an important trauma mechanism impacting the number of hospitalizations in the Unified Health System1. Between 2008 and 2014, 1,291,585 people were admitted to Brazilian hospitals as victims of burns2. The etiologies of these injuries vary between electrical, scalding, flame, contact or chemical causes3.
Burns caused by chemical agents do not occur frequently, ranging from 1.5 to 8.5% of hospitalization cases due to burns in different countries4,5. Injuries caused by acidic substances cause intracellular dehydration and protein coagulation, leading to coagulation necrosis, but there is less spread of the lesion to the tissues; the bases, on the other hand, cause necrosis by liquefaction, through the cellular destruction of fat and by the hydrolysis of proteins, which may affect adjacent tissues more intensely6.
The importance of epidemiological studies on chemical burns is due to multiple factors. The most prevalent etiological agents vary according to the countries and regions, motivated by altering the industrial park, culture and even armed conflicts7. This burn is reported more frequently in work environments, thus affecting the economically active population, causing an economic impact not only due to the treatment but also due to the loss of hours worked4.
OBJECTIVE
This study aims to analyze the profile of patients hospitalized due to chemical burns in a burn unit, evaluating the etiological agent’s impact and the accident’s place on these injuries.
METHODS
This descriptive, retrospective study analyzes the epidemiological profile of patients with chemical burns admitted to the State Hospital of Bauru Burn Therapy Unit between 2008 and 2018.
The Burn Unit is located at the State Hospital of Bauru, in Bauru, SP. It was created in 2004 and is one of the 19 burn treatment units in São Paulo and a reference for patients from the 645 municipalities. The Burn Center consists of an Intensive Care Unit (ICU) and a ward with four and 12 beds, respectively, and has the structure to treat all age groups.
The variables analyzed in the medical records were: age, sex, location, comorbidities, chemical agents involved in the burns, body surface area burned (BSB), anatomical regions involved, the place where the burn occurred, need for an ICU bed, inhalation injury, number of surgical interventions, complications and mortality.
All variables were collected in an Excel spreadsheet (Microsoft©). Statistical analyzes were performed using the T-Student test for quantitative variables and Chi-square for qualitative variables, with values lower than p<0.05 considered statistically significant.
All procedures performed in this study followed the 1964 Declaration of Helsinki and its subsequent amendments. The local Ethics Committee approved this study (protocol number: 35971220.4.0000.5411).
RESULTS
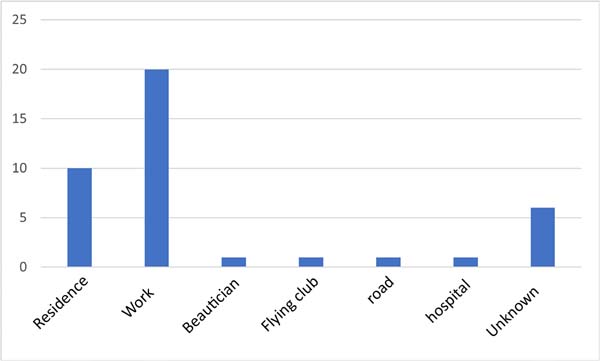
In total, 2364 medical records were reviewed, and 40 (1.7%) patients were found in whom the etiology of the burn was chemical. The mean age was 35 years (ranging from 1 to 53 years), with a predominance of males, with 30 (75%) hospitalized individuals (Table 1). The main site of trauma was the work environment in 20 cases (50%), followed by the home environment in 10 (25%) (Figure 1). In this last group are the two cases of aggression and one case of attempted self-extermination.
| General data | |
|---|---|
| Age years) | 35 |
| Sex | |
| Man | 30 |
| Women | 10 |
| BSB | |
| 0-10% BSB | 29 |
| 10-20% BSB | 7 |
| 20-40% BSB | 3 |
| > 40% BSB | 1 |
| Eye injury | 11 |
| Airway injury | 1 |
| Days of hospitalization | 17 |
| Need ICU | 10 |
| Deaths | 0 |
BSB: Burned body surface
ICU: Intensive care unit
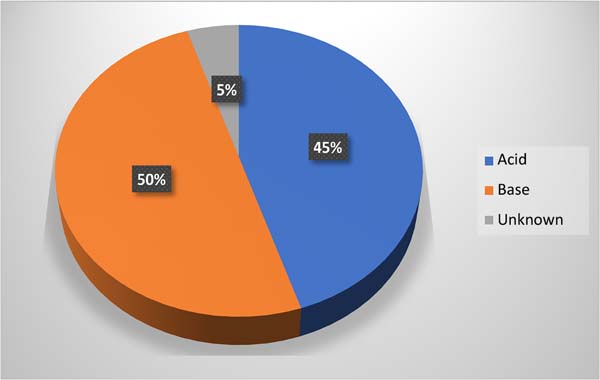
Base accidents were responsible for 20 (50%) admissions, with caustic soda (27.5%) and lime (10%) as the main products involved; acids corresponded to 18 (45%), and the most common substance was sulfuric acid (10%) (Figure 2) (Table 2).
| Chemical agent | Cases | % |
|---|---|---|
| Acids | ||
| Sulfuric acid | 4 | 10.0 |
| Citric acid | 1 | 2.5 |
| Chromic acid | 1 | 2.5 |
| Hydrochloric acid | 1 | 2.5 |
| Acetic acid | 1 | 2.5 |
| Mixture of acids | 3 | 7.5 |
| Unspecified acid | 8 | 20.0 |
| Bases | ||
| Caustic soda | 11 | 27.5 |
| Lime | 4 | 10.0 |
| Sodium bicarbonate | 1 | 2.5 |
| Unspecified base | 4 | 10.0 |
| Unknown chemical agent | 2 | 5.0 |
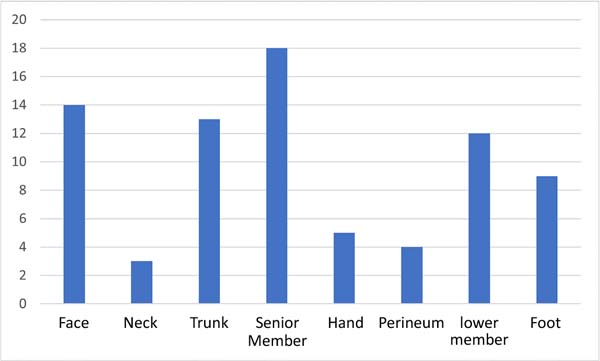
The average BSB was 7.5%, with only four (10%) patients totaling more than 20% of the BSB (Table 1). The anatomical sites most involved were the upper limbs in 18 cases (23.1%), the face in 14 (17.9%), the trunk in 13 (16.7%) and lower limbs in 12 (15.4%) (Figure 3). Eye burns occurred in 11 (27.5%) patients, and two had impaired vision. Only one (2.5%) individual had an airway injury.
Thirty (75%) patients underwent surgical procedures comprising debridement, grafting, and flaps, with an average of 1.6 procedures per patient.
An intensive care bed was required for 10 (25%) cases. During hospitalization, five (12.5%) patients developed complications. The mean length of stay was 17 days (Table 1). There were no deaths during hospitalization in our sample.
When comparing the injuries that occurred at home and work, we did not find statistical significance concerning sex (p=0.56), age (p=0.24), etiology (p=0.24), BSB (p=0 .08), number of procedures (p=0.56), need for an ICU bed (p=0.61) and days of hospitalization (p=0.36) (Table 3). However, when comparing the same variables between accidents involving acids and bases, we evidenced a difference in the number of patients admitted to the ICU, with eight patients with injuries involving bases and two with acids (p=0.04) (Table 4).
| Information | Work (n=20) | House (n=10) | P |
|---|---|---|---|
| Age | 34.9±11.3 | 38.4±4.5 | 0.24 |
| Sex | 0.56 | ||
| Feminine | 4 (20) | 3 (30) | |
| Male | 16 (80) | 7 (70) | |
| Etiology | 0.24 | ||
| Base | 9 (45) | 7 (70) | |
| Acid | 10 (50) | 3 (30) | |
| Unknown | 1 (5) | 0 | |
| % BSB | 10.4±11.4 | 5.1±4.3 | 0.08 |
| Procedure | 0.56 | ||
| Yes | 16 (80) | 7 (70) | |
| No | 4 (20) | 3 (30) | |
| ICU$ | 0.61 | ||
| Yes | 6 (30) | 3 (30) | |
| No | 14 (70) | 7 (70) | |
| Hospitalization Days | 19±12.3 | 22±29.8 | 0.36 |
BSB: Burned body surface
ICU: Intensive care unit
| Variables | Acid (n=18) | Basis (n=20) | P |
|---|---|---|---|
| Age | 34.0±12.8 | 36.8±12.4 | 0.49 |
| Sex | |||
| Feminine | 6 (33.3) | 4 (20.0) | 0.35 |
| Male | 12 (66.7) | 16 (80.0) | |
| % BSB | 7.1±7.8 | 8.0±11.1 | 0.76 |
| Procedure | |||
| Yes | 13 (72.2) | 15 (75.0) | 0.85 |
| No | 5 (27.8) | 5 (25.0) | |
| ICU$ | |||
| Yes | 2 (11.1) | 8 (40.0) | 0.04 |
| No | 16 (88.9) | 12 (60.0) | |
| Hospitalization Days | 12.4±8.2 | 21.6±22.9 | 0.12 |
| Complications | |||
| Yes | 2 (11.1) | 3 (15) | 0.47 |
| No | 16 (88.9) | 17 (85) |
BSB: Burned body surface
ICU: Intensive care unit
DISCUSSION
In the literature, only one Brazilian study exclusively assesses the epidemiology of chemical burns in Brazil. Cardoso et al.8 analyzed patients treated on an outpatient and inpatient basis at the Sorocaba Burn Unit between 2001 and 2011, finding 61 patients. Despite the smaller sample presented in this study, we analyzed only hospitalized individuals and showed the percentage of chemical burns relative to the total number of patients hospitalized for other causes of burns, totaling 1.7%. This number is in line with the findings of previous studies on the epidemiology of burns, in which chemical injuries represented 1.4 - 10.1% of total hospitalizations5,9-11.
In the gender assessment, 75% of the analyzed patients were male. The largest number of men with this type of burn was also reported in other articles on the subject4,12. Greater exposure due to work activities that cause exposure to chemical products is one of the possible explanations for this fact6. The average age found was 35 years, with 87.5% of patients between 18 and 60 years old, showing the impact of this type of injury on the economically active population.
Although some articles suggest increased burns in the home environment13,14, most accidents were at work in our sample, as evidenced by most articles on the subject. This data points to the need and importance of using Personal Protective Equipment (PPE) in chemical industries, such as masks, gloves and boots, and training and workplace safety programs to prevent these traumas15. Despite this difference, we found no statistical significance between the places where the accidents occurred regarding demographic data and the treatment of these patients.
Burns caused by basic agents accounted for the largest share of injuries, as shown by Ricketts & Kimble14 and Hardwicke et al.5. Caustic soda injuries occurred in 27.5% of cases. In addition to being present in the chemical industries, it is part of the composition of cleaning products, increasing the incidence of injuries with this substance in the domestic environment. Caustic soda has a high penetration power into tissues, and tissue destruction remains after the initial aggression16.
Lime was the second most common basic substance in 10% of cases. Often used by professionals and amateurs in civil construction, calcium oxide accounts for 65% of its component, and when it reacts with water, it forms calcium hydroxide, leading to burns. The characteristic presentation of these lesions is insidious, and it may take hours for the patient to notice the burn, and it mainly affects the lower limbs16.
Acid burns occurred in 45% of patients; the most common substance was sulfuric acid in 10% of cases. Widely used in the industrial field, in oil refineries, dyes, metal foundry, and fertilizer production, among others, its mechanism of action is through tissue dehydration and increased local heat, which leads to necrosis by coagulation and thrombosis in the microcirculation, causing painful and deep burns at the site17.
When comparing the groups of chemical burns caused by acids and bases, we found a statistically different number of patients who needed an ICU bed, greater among patients who suffered accidents with basic substances. These burns tend to be more severe due to the liquefaction mechanism, which allows the injury to go deeper16.
Ocular injuries are a common feature in this type of burn6,12,18, and in our series, they occurred in 27.5% of the cases. Even small volumes can damage the eyes, cornea and limbic region19. The erroneous attempt to remove the product through itching hands can increase tissue damage6. The immediate, exhaustive washing of the eyes after contact, even in pre-hospital care, can attenuate the evolution of the lesion19.
The mean BSB extent was 7.5%, with 29 (72.5%) patients having burned areas smaller than 10%. However, despite not having extensive burns, surgical procedures were required in 70% of the patients. This may result from inefficient initial care, in which the chemical agents were not properly removed, leading to further deepening of the lesion18.
The average length of hospital stay was 17 days, within what was previously published in the literature, 10 to 46.5 days6,7,12,18. Hospitalizations due to chemical burns have a longer hospitalization time due to the characteristics of the burn that lead to difficulty in managing the injury. The epithelial attachments of chemical wounds present a greater slowdown in the replication process and migration, which may cause a delay in tissue repair14.
This study is not free of limitations, as its retrospective nature, based on analysis of medical records, sample limited to only one institution and restricted to patients with chemical burns are among the limitations of this study. Future work may explore chemical burns in a multicenter way, dimensioning the impact of these injuries on the Brazilian population in a broader way.
CONCLUSION
This is the second Brazilian study to explore the epidemiology of chemical burns. With a relatively low incidence, this type of injury affects individuals in the economically active age group and frequently occurs in the workplace. Injuries with basic substance had a statistical difference in the need for an ICU bed. Although most burns are smaller than 10%, there was ocular involvement in 27.5% of cases and the need for a long period of hospitalization to treat these patients.
REFERENCES
1. Santos JV, Souza J, Amarante J, Freitas A. Burden of Burns in Brazil from 2000 to 2014: A Nationwide Hospital-Based Study. World J Surg. 2017;41(8):2006-12. DOI: 10.1007/s00268-017-3988-5
2. Citron I, Amundson J, Saluja S, Guilloux A, Jenny H, Scheffer M, et al. Assessing burn care in Brazil: An epidemiologic, cross-sectional, nationwide study. Surgery. 2018;163(5):1165-72. DOI: 10.1016/j.surg.2017.11.023
3. Papp A, Haythornthwaite J. Ethnicity and etiology in burn trauma. J Burn Care Res. 2014;35(2):e99-105. DOI: 10.1097/BCR.0b013e3182a223ec
4. Koh DH, Lee SG, Kim HC. Incidence and characteristics of chemical burns. Burns. 2017;43(3):654-64. DOI: 10.1016/j.burns.2016.08.037
5. Hardwicke J, Hunter T, Staruch R, Moiemen N. Chemical burns--an historical comparison and review of the literature. Burns. 2012;38(3):383-7. Burns. 2012;38(3):383-7. DOI: 10.1016/j.burns.2011.09.014
6. Maghsoudi H, Gabraely N. Epidemiology and outcome of 121 cases of chemical burn in East Azarbaijan province, Iran. Injury. 2008;39(9):1042-6. DOI: 10.1016/j.injury.2008.03.019
7. Ye C, Wang X, Zhang Y, Ni L, Jiang R, Liu L, et al. Ten-year epidemiology of chemical burns in western Zhejiang Province, China. Burns. 2016;42(3):668-74. DOI: 10.1016/j.burns.2015.12.004
8. Cardoso L, Orgaes FS, Gonella HA. Estudo epidemiológico das queimaduras químicas dos últimos 10 anos do CTQ-Sorocaba/SP. Rev Bras Queimaduras. 2012;11(2):74-9.
9. Gonçalves AJ, Cunha MTR, Santos JF. Epidemiological study of burns at the Hospital of Clinics, Federal University of the Triângulo Mineiro. Rev Bras Cir Plást. 2020;35(4):420-6.
10. Padua GAC, Nascimento JM, Quadrado ALD, Perrone RP, Silva Junior SC. Epidemiology of burn cases hospitalized at the Plastic Surgery and Burns Service of Santa Casa de Misericórdia de Santos, Brazil. Rev Bras Cir Plást. 2017;32(4):550-5.
11. Leitão EPC, Gomes HFC, Silva VAT, Santana RV. Epidemiological study of patients hospitalized in the burn care unit of the Vila Penteado General Hospital - São Paulo. Rev Bras Cir Plást. 2014;29(2):264-8.
12. Li W, Wu X, Gao C. Ten-year epidemiological study of chemical burns in Jinshan, Shanghai, PR China. Burns. 2013;39(7):1468-73. DOI: 10.1016/j.burns.2013.03.012
13. Wibbenmeyer LA, Morgan LJ, Robinson BK, Smith SK, Lewis RW 2nd, Kealey GP. Our chemical burn experience: exposing the dangers of anhydrous ammonia. J Burn Care Rehabil. 1999;20(3):226-31. DOI: 10.1097/00004630-199905000-00013
14. Ricketts S, Kimble FW. Chemical injuries: the Tasmanian Burns Unit experience. ANZ J Surg. 2003;73(1-2):45-8. DOI: 10.1046/j.1445-2197.2003.02617.x
15. Zhang YH, Han CM, Chen GX, Ye CJ, Jiang RM, Liu LP, et al. Factors associated with chemical burns in Zhejiang province, China: an epidemiological study. BMC Public Health. 2011;11:746.
16. Palao R, Monge I, Ruiz M, Barret JP. Chemical burns: pathophysiology and treatment. Burns. 2010;36(3):295-304. DOI: 10.1016/j.burns.2009.07.009
17. Wang Y, Yu X, Qian W, Zhou D, Yang T, Wang S, et al. Epidemiologic Investigation of Chemical Burns in Southwestern China from 2005 to 2016. J Burn Care Res. 2018;39(6):1006-16. DOI: 10.1093/jbcr/iry032
18. Xie Y, Tan Y, Tang S. Epidemiology of 377 patients with chemical burns in Guangdong province. Burns. 2004;30(6):569-72. DOI: 10.1016/j.burns.2004.01.028
19. Sharma N, Kaur M, Agarwal T, Sangwan VS, Vajpayee RB. Treatment of acute ocular chemical burns. Surv Ophthalmol. 2018;63(2):214-35.
1. Universidade Estadual Paulista, Faculdade de Medicina de Botucatu, Departamento
de Cirurgia e Ortopedia, Divisão de Cirurgia Plástica, Botucatu, São Paulo, Brazil
2. Universidade Estadual Paulista, Faculdade de Medicina de Botucatu, Botucatu, São
Paulo, Brazil
3. Hospital Estadual de Bauru, Bauru, São Paulo, Brazil
MSS Data analysis and/or interpretation, Statistical analysis, Data collection, Conception and design of the study, Project management, Investigation, Methodology, Writing - Preparation of the manuscript.
BFMN Statistical analysis, Data collection, Conception and design of the study, Writing - Preparation of the original.
AJCVS Analysis and/or interpretation of data, Data Collection, Methodology.
AAMF Analysis and/or interpretation of data, Data Collection, Methodology.
MMC Data collection, Conception and design of the study, Writing - Preparation of the original.
ABPMO Data Collection, Methodology, Writing - Preparation of the original.
CR Writing - Proofreading and Editing, Supervision, Visualization.
AAP Writing - Proofreading and Editing, Supervision, Visualization.
Corresponding author: Murilo Sgarbi Secanho Av. Professor Mário Rubens Guimarães Montenegro, Unesp - Campus de Botucatu, Botucatu, SP, Brazil. Zip code: 18618-687, E-mail: murilo_sgs@hotmail.com
Article received: October 25, 2021.
Article accepted: April 7, 2022.
Conflicts of interest: none.










 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter