

Original Article - Year 2022 - Volume 37 - Issue 4
Estimation of implant volume in immediate breast reconstruction using mastectomy specimen weight
Estimativa do volume do implante na reconstrução mamária imediata utilizando o peso do espécime da mastectomia
ABSTRACT
Introduction: The choice of the appropriate volume of silicone implant to replace the mastectomy specimen is usually performed with the aid of provisional silicone molds which leads to a subjective evaluation and dependent on surgeons experience. The discovery of a simple mathematical predictive model allowed an objective, easy and reproducible evaluation by any plastic surgeon. This study aimed to identify the eficiency of a mathematical model in patients operated in Brazil, with ethnic characteristics difierent from other countries derived from the formulas had been founded (France and Taiwan).
Methods: A search was carried out in the PubMed and VHL databases in the last 10 years, using the keywords: "Breast Implants", "Mammoplasty"," Mastectomy", "Reconstruction" and "Methods in Plastic Surgery" and a prospective study with 20 patients (30 breasts) operated by authors.
Results: We used the Nice (France) formula because our patients mostly produced specimens larger than 450g and our technique, using synthetic mesh forming the pectoral submuscular pouch, allowed the reconstruction in a single time with silicone prostheses larger than 300cc.
Conclusion: There was eficiency in the use of the Nice Formula to identify the appropriate volume in immediate breast reconstruction to mastectomy using the weight of the specimen in grams and it had been produced satisfactory aesthetic results in the immediate and late postoperative period.
Keywords: Mastectomy; Mammaplasty; Breast implants; Reconstructive surgical procedures; Breast neoplasms.
RESUMO
Introdução: A escolha do volume adequado do implante de silicone à substituição do espécime da mastectomia é usualmente realizada com auxílio de moldes provisórios de silicone, levando a uma avaliação subjetiva e dependente da experiência do cirurgião. A descoberta de um modelo preditivo matemático simples permitiu uma avaliação objetiva, fácil e reprodutível por qualquer cirurgião plástico. Este estudo objetivou identificar a eficiência de um modelo matemático nos pacientes operados no Brasil, com características étnicas diferentes aos outros países de origem das fórmulas (França e Taiwan).
Métodos: Foi realizada uma pesquisa nos bancos de dados PubMed e BVS nos últimos 10 anos, utilizando as palavras-chave: Implantes de Mama, Mamoplastia, Mastectomia, Reconstrução e Métodos em Cirurgia Plástica, e estudo prospectivo com 20 pacientes (30 mamas) operadas pelo autor.
Resultados: Utilizamos a fórmula de Nice (França), pois nossas pacientes na sua grande maioria produziram espécimes maiores que 450g e a nossa técnica, com utilização de tela sintética formando a bolsa submuscular peitoral maior, permitiu a reconstrução em tempo único com próteses de silicone maiores que 300cc.
Conclusão: Houve eficiência na utilização da Fórmula de Nice em identificar o volume adequado na reconstrução mamária imediata à mastectomia utilizando o peso do espécime em gramas e obtivemos resultados estéticos satisfatórios no pós-operatório imediato e tardio.
Palavras-chave: Mastectomia; Mamoplastia; Implantes de mama; Procedimentos cirúrgicos reconstrutivos; Neoplasias da mama.
INTRODUCTION
Theoretically, the breast volume resected in a skin-sparing mastectomy (SPM) needs to be replaced by a similar volume in immediate breast reconstruction with a silicone implant (IBRSI) when there is symmetry between the breasts.
Empirical intraoperative decisions based on visualization of the volume of the opposite breast after multiple attempts to use silicone molds or simple replacement using the weight of the mastectomy specimen for a similar volume of the prosthesis to be implanted are routinely performed by us. However, decisions are subjective and dependent on the surgeon’s experience.
The discovery and use of a simple mathematical predictive model, transforming the weight in grams of the specimen to the volume in cc of the implant, allowed an objective, easy and reproducible evaluation by any plastic surgeon.
In bibliographic research of the last 10 years, we identified two mathematical formulas, one from Nice, France (Georgiou, 2012), and another from Taiwan (Shia, 2018), and we indicate the Nice model as the ideal for Brazilian mastectomized women, even using the authors’ modified technique.
OBJECTIVE
The objective of this study was to identify, through a literature review, whether there is surgical efficiency at RMIP after mastectomy using a mathematical formula based on the weight of the mastectomy specimen, despite some modifications in the surgical technique described by the authors mentioned above.
METHODS
Five articles were found in the medical literature (PubMed) in the last 10 years, reporting the estimation of adequate implant volume in immediate breast reconstruction (IBRSI) using mastectomy specimen weight or preoperative 3D imaging assessments.
The authors have used the surgical technique since February 2019 in a private clinic and a public health institution, using a pectoralis major muscle flap and meshUltrapro, in Fortaleza, Ceará, Brazil1.
A pectoralis major submuscular pocket was dissected in patients undergoing mastectomy who had an adequate skin flap, at least 1 cm thick and good quality. The inferomedial edge of the pectoral muscle (up to the second intercostal space) was elevated to place a silicone mold. The fabric (mesh) synthetic was sutured to this edge of the pectoralis muscle along its entire inferior course to the inframammary fold.
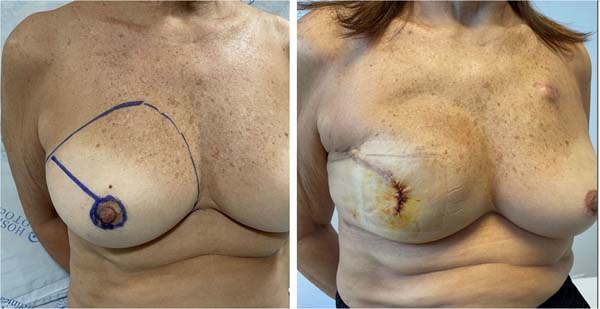
After choosing the implant, it was introduced under the synthetic mesh. This material was fixed with Vicryl suture® 2-0 laterally at the level of the anterior axillary line to the dissected fascia of the serratus anterior muscle and even the inframammary fold in the desired position. A suction drain was placed in the submuscular pocket and the subcutaneous tissue of the mastectomy flap through separate cutaneous access, followed by the closure of the surgical wound by tissue planes (Figure 1).
The following were included in this series: 20 female patients with a total of 30 breasts, aged between 33 and 63 years old, with a mean Body Mass Index (BMI) of 27.2 kg/m2, with a follow-up of up to one year of postoperative.
The number of Opinion in the Ethics and Research Committee was: 4,844,482. There are no conflicts of interest with the companies mentioned.
RESULTS
The average volume of the implanted prostheses was 390cc, and the maximum weight of the specimens was 670g. Depending on the patient’s health plan release, implants from different suppliers were used with a high or moderate profile (previous assessment of the base of the operated breast, sagging, breast hypertrophy).
There was extrusion of two silicone prostheses (6.6% of the sample) due to necrosis of the mastectomy skin flap in one diabetic patient and another patient (submitted to axillary lymphadenectomy) with persistent seroma after removal of the suction drain on the 16th day of surgery postoperative.
DISCUSSION
Shia et al.2 performed a retrospective study with 182 patients, from January 2009 to December 2015, who underwent skin-sparing mastectomy (PPM) and immediate breast reconstruction with silicone implant (IBRSI) and used different types of implants after placement provisional of a silicone mold to choose the ideal implant, in addition to visualization and personal experience of the surgeon.
Age, BMI and present comorbidities were related, and the mastectomy specimen weight was used as a coefficient of a mathematical predictive model (formula):
where x is the volume, in cc, of the silicone implant, and y is the weight of the specimen (mastectomy product), in grams, after PPM.
There was no use of the Acellular Dermal Matrix (ADM) prohibited in Taiwan. The implant was partially covered by pectoralis major and serratus anterior muscle flaps, with the inferolateral quadrant of the mastectomy flap lacking muscle coverage and being covered only by subcutaneous tissue when using a larger prosthesis.
In 107 patients (58.1%), the Mentor® implant was used with a moderately increased profile and in 34 patients (18.8%), Mentor® was used with a classic moderate profile, corresponding to 76.9% of cases.
About 70% of the patients were between 40 and 59 years old, with a mean BMI of 23.7kg/m2. The mean implant volume was reported to be 264.31cc, and the mean specimen weight was 314.06g, which may contraindicate the formula for Western women, although 64 patients (35%) used an implant larger than 300cc, with concluded that the formula was suitable for use on specimens up to 700g.
Georgiou et al.3 reported breast reconstruction after skin-sparing mastectomy in 79 patients with a mean age of 52 years, with 62 therapeutic surgeries and 48 prophylactic surgeries. Anatomical gel implants were used and positioned in the subcutaneous space. There was no specific method for choosing the implant, and the decision on the appropriate implant was based on the surgeon’s experience regarding the observed visual aspect.
A simple mathematical equation was used:
Formula 4
It was concluded that a smaller implant produced a desirable and less artificial esthetic result for breasts with specimen weights greater than 300g due to the natural phenomenon of less skin retraction in the postoperative period.
Parmar et al.4 used the physical law of buoyancy, called “Archimedes Principle,” which says that any body totally immersed or partially immersed in any liquid is subject to a vertical force from the bottom up equal to the weight of the portion of fluid displaced by the body.
It is known that the breast parenchyma has a density of 1.06 g/cm3. The gravitational density of water is 1.0 g/cm3, and that of fat is 0.92 g/cm3, and breast tissue is made up of a heterogeneous mixture of fibrous and fatty tissues, despite menopause, with normal variations between women. and even between the breasts of the same patient (Figure 2).
In the study, the mean age was 42.4 years. Fifty-two specimens were from premenopausal women, and 17 were from postmenopausal women. Twenty-six patients underwent bilateral breast reduction, two had a bilateral mastectomy, nine had a unilateral mastectomy, and four underwent unilateral breast reduction. The mean weight of the specimens was 545.4g, while the mean volume of the implants was 509cc, with a difference of 36.4 units (7%) (Figure 3).
It was concluded that there was no statistical significance in this sample.
Yip et al.5 and Kim et al.6 proposed a 3D radiological assessment of the body as a non-invasive method, with the patient being examined standing and creating a virtual 3D model, providing an assessment of symmetry, volume, contour, surface and distance between the breasts.
Unfortunately, the various methods for measuring breast volume described in the literature are of variable reliability, and many are used in preoperative assessment. These methods present technical details that are difficult to perform and reproduce, have a high financial cost and low acceptance by patients, and are not used by surgeons in daily practice.
Using a simple mathematical formula in the operating room, we could indicate an easy and reproducible method for choosing the ideal volume for breast reconstruction after skin-sparing mastectomy (SPM).
We used the Nice formula (Georgiou et al.3), as most of our patients produced specimens larger than 450g, and our technique, using a synthetic mesh forming the pectoralis major submuscular pocket, allowing for a one-time reconstruction with silicone prostheses larger than 300cc (Figures 4 and 5).
There was no preference for the manufacturer of silicone implants, only the profile chosen was a high or moderate plus, depending on the base of the breast, degree of sagging and breast hypertrophy.
Currently, we do not use a silicone expander, and we contraindicate breast reconstruction in patients with a BMI greater than 30 kg/m2 or who will undergo immediate radiotherapy for mastectomy, in addition to associated comorbidities: anemia: hemoglobin (Hb) less than 11g/dl, uncontrolled diabetes and/or systemic arterial hypertension (SAH), smoking or gigantomastia.
Our series revealed a mutual satisfaction between the patient and the surgeon regarding the visual and aesthetic evaluation (volume under the garments, symmetrization, correction of breast ptosis) in the immediate and late postoperative period, avoiding frequent visits to the assistant physician for expansion sessions and additional surgical procedures and consequent reduction in surgical morbidity.
There was a need for a second surgical procedure for contour fat grafting of the upper and medial pole of the reconstructed breast in six patients, mainly in breasts undergoing adjuvant treatment with radiotherapy.
CONCLUSION
There was efficiency in the use of the Nice Formula in identifying the appropriate volume in breast reconstruction immediately after mastectomy (using the weight of the specimen in grams), making this mathematical formula an important tool in the therapeutic arsenal of the plastic surgeon and avoiding the use of reusable surgical molds and potentially contaminated.
REFERENCES
1. Bezerra FJF, Moura RMG. Synthetic mesh as a potential low-cost alternative to dermal matrix in mammary reconstructions. Rev Bras Cir Plást. 2021;36(2):122-8. DOI: 10.5935/2177-1235.2019RBCP0000
2. Shia WC, Yang HJ, Wu HK, Lin SL, Lai HW, Huang YL, et al. Implant volume estimation in direct-to-implant breast reconstruction after nipple-sparing mastectomy. J Surg Res. 2018;231:290-6. DOI: 10.1016/j.jss.2018.05.024
3. Georgiou CA, Ihrai T, Chamorey E, Flipo B, Chignon-Sicard B. A formula for implant volume choice in breast reconstruction after nipple sparing mastectomy. Breast. 2012;21(6):781-2.
4. Parmar C, West M, Pathak S, Nelson J, Martin L. Weight versus volume in breast surgery: an observational study. JRSM Short Rep. 2011;2(11):87. DOI: 10.1258/shorts.2011.011070
5. Yip JM, Mouratova N, Jeffery RM, Veitch DE, Woodman RJ, Dean NR. Accurate assessment of breast volume: a study comparing the volumetric gold standard (direct water displacement measurement of mastectomy specimen) with a 3D laser scanning technique. Ann Plast Surg. 2012;68(2):135-41.
6. Kim JH, Park JW, Woo KJ. Prediction of the Ideal Implant Size Using 3- Prediction of the Ideal Implant Size Using 3-Dimensional Healthy Breast Volume in Unilateral Direct-to-Implant Breast Reconstruction. Medicina (Kaunas). 2020;56(10):498. DOI: 10.3390/medicina56100498
1. Plasticorp Clinica de Cirurgia Plástica, Cirurgia Plástica, Fortaleza, CE, Brazil
2. Hospital Geral de Fortaleza, Cirurgia Plástica, Fortaleza, CE, Brazil
FJFB Analysis and/or data interpretation, Conception and design study, Conceptualization, Final manuscript approval, Methodology, Realization of operations and/or trials, Writing - Original Draft Preparation, Writing - Review & Editing.
RMGM Analysis and/or data interpretation, Conception and design study, Conceptualization, Formal Analysis, Realization of operations and/or trials.
Corresponding author: Francisco José Fontenele Bezerra Rua Barbosa de Freitas,1911, Fortaleza, CE, Brazil. Zip Code: 60170-021, E-mail: fco.fontenele@yahoo.com.br
Article received: July 21, 2021.
Article accepted: July 11, 2022.
Conflicts of interest: none.












 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter