

Articles - Year 2004 - Volume 19 -
Loco-regional Fasciocutaneous Flaps for Prompt Repair of Type I Neurofibromatosis *
Retalhos Fasciocutâneos Loco-regionais na Reparação Imediata da Neurofibromatose Tipo I*
ABSTRACT
This paper aims to study surgical techniques, whether associated or isolated, which provide less stigmatizing and deforming results for patients with type I neurofibromatosis (NF I), in an attempt to ensure a quality of life with more dignity and better social integration. Thirty patients with NF I were studied for a period of six years. Different surgical techniques were used to remove lesions ranging from 3 to 51 cm, located in different anatomical regions, and their results were analyzed. Twenty-one patients benefited from excisions and repairs
with flaps, and the remaining, from procedures of excision and suture or z-plasty. Loco-regional fasciocutaneous flaps provided the best results both functionally and esthetically, with fewer sequelae. Even in the cases with residual sequelae in the skin used for the cutaneous flaps, the disease did not evolve and there was no malignization. Loco-regional fasciocutaneous flaps enabled the repair of wide bleeding areas and the resection of larger tumors. Medium-sized lesions are satisfactorily removed using the s-plasty ou z-plasty techniques for coverage. Small lesions are appropriately repaired using excision and suture, with no need for flaps, especially those located on the face and nose.
Keywords: Neurofibromatosis I; plexiform neurofibromatosis; neurocutaneous syndromes.
RESUMO
Objetivou-se no presente trabalho estudar técnicas cirúrgicas associadas ou isoladas, buscando resultados menos estigmatizantes e deformantes aos portadores da neurofibromatose tipo 1 (NF I) na tentativa de assegurar-lhes uma qualidade de vida mais digna e melhor integração social. Trinta pacientes portadores de NF I foram estudados por um período de seis anos. Diferentes técnicas cirúrgicas foram empregadas para a remoção de lesões que variaram de 3 a 51 cm, localizadas em diversas regiões anatômicas, com análise dos resultados. Vinte e um pacientes se beneficiaram de excisões e reparações com retalhos, e os demais, com procedimentos de excisão e sutura ou "Z" plastia. Os retalhos fasciocutâneos loco-regionais proporcionaram os melhores resultados funcionais e estéticos, com menor número de seqüelas. Mesmo nos casos de comprometimento residual da pele usada nos retalhos cutâneos não houve evolução da doença nem malignização. Os retalhos fasciocutâneos loco-regionais possibilitaram o reparo de grandes áreas cruentas e a ressecção dos tumores mais volumosos. Lesões de médio porte são satisfatoriamente removidas utilizando-se o "S" itálico ou "Z" plástico para cobertura. Pequenas lesões são reparadas adequadamente mediante excisão e sutura, sem necessidade de retalhos, principalmente as localizadas na face e no nariz.
Palavras-chave: Neurofibromatose; neurofibromatose plexiforme; síndromes neurocutâneas
Neurofibromatosis or phakomatosis, a word of Greek origin meaning a spot, was introduced in the medical literature in 1768. The study of neurofibromatosis goes back to the seventeenth century when the surgeon Mark Akenside described, in a 60 yearold man, multiple cutaneous and subcutaneous twnors that he attributed to paternal heritage(l). Toselius (1793) and Smith (1849) reported findings in two similar cases by using anatomical and histopathological necropsy studies(1). However, half of NF I cases are sporadic, and parents are not affected, with the disease appearing spontaneously, as a conseguence of genetic alterations or mutations(l).
It was Friedrick von Recklinghausen, in 1882, also based on necropsy findings, who best described this pathology and clarified its origin in the Nervous System with cutaneous, visceral and neurological conseguences. For that reason, it was called neurofibromatosis or Von Recklinghausen's disease(l).
NF I is a family genetic abnormality characterized by the growth of tissues derived from neural crests; its changes manifest themselves before the thirtieth day of intra-uterine life, when visceral differentiation starts(2) .
The gene that causes NF I is located next to the centromer of the long arm of chromosome 17. The disease represents a new mutation in fifty percent of the patients affected.(3). The proteins that cause these changes were identified and named neurofibromin for NF I, and Merlin protein or schwannomin for NF II, respectively(4).
Other factors account for tumor growth, including androgen and estrogen factors in the passage into pubert); and the increase in hormone loads during pregnancy, facts which have not been proven so far(5).
The growth of tumors in NF I is unpredictable, with periods of rapid growth and others of slower growth; many remain static indefinitely after a quick development. This irregular behavior makes it difficult to document the effectiveness of a potentially healing treatment(3).
Therapy is limited to surgical eXCISIons that are often unsatisfactory; because in many cases the full resection of large lesions is rarely possible and tumors emerge continuously over the lifetime(6). The existing literature is generally limited to isolated reports, which are disseminated to the medical community only because they attract attention due to the deformities(l,5,7-15).
From the surgical standpoint, there are few current publications seeking to improve the deformation and disfigurement of patients who suffer from this genetic abnormality.
The goal of this study was to present associated or isolated surgical techniques, in an attempt, through less trawllatic and more effective surgeries, to achieve less stigmatizing and deforming results and a quality of life with more digruty and more rapid social reintegration.
METHODS
Thirty patients (17 men, 13 women), with ages ranging from 08 to 60 years of age were selected for this study.
All patients were previously assessed, so as to ensure that all of them could lmdergo the proposed surgeries. Surgical incisions were previously marked using methylene blue, with which the surgeon also drew flaps, z-plasties, and s-plasties, the zig-zag incisions that were meant to guide surgical closing, as well as to assess the extension of resections and the technique that was being used.
Considering the rich vascularization, in the cases of head and neck tumors, previous infiltration was petformed with 0.5% lidocaine hydrochloride in association with 1 :400,000 epinephrine, as well as preventive cerclage with separated stitches, with the aim of reducing bleeding. For upper and lower limb tumors, it was imperative to use a pneumatic tourniquet.
In all patients with encapsulated and well-individualized tumors that could be easily enucleated, the cutaneous lining was dissected in its entire thickness with a digital dissection. For tumors affecting the skin, 0.5 cm of its thickness were preserved for making the flap that served to repair the bloody zone left by the resection. When lesions were located in a plane between the fascia and muscles, they did not offer difficulty for exeresis, which ensured stitches would not leave motor or sensory sequelae. After tumor removal, hemostasia was reviewed, and the muscular fascia was sutured, if it had been lacerated or incised, with a 3-0 nylon monofilanlent suture. Next, excesses of the fasciocutaneous flap were excised, vessels were clotted, the pneumatic tourniquet was removed, in the case of lower and upper limbs, or the cerclage, when the procedure had been on the cephalic segment. The following phases consisted of closing the subcutaneous cellular tissue with 3-0 absorbable monoftlanlent suture and the skin was sutured with separate stitches, interspersed with continuous 4-0 nylon monofilament sutures. As operated areas left a bleeding zone and a virtual dead space, a continuous suction drain was placed and removed when drainage stopped or reached 20 and 50 ml in 24 hours.
Dressings were made with padded gauze, simple gauze, crepe bandages, tailor-made elastic meshes or masks with moderate compression, which were removed every two days.
All patients were observed and followed up for 6 years (1995 to 2001). Revisions were made on a monthly basis, in the first 6 months and, from then on, biannually. The quality of scars, evolution and emergence of new tumors, pain and signs of relapse were assessed.
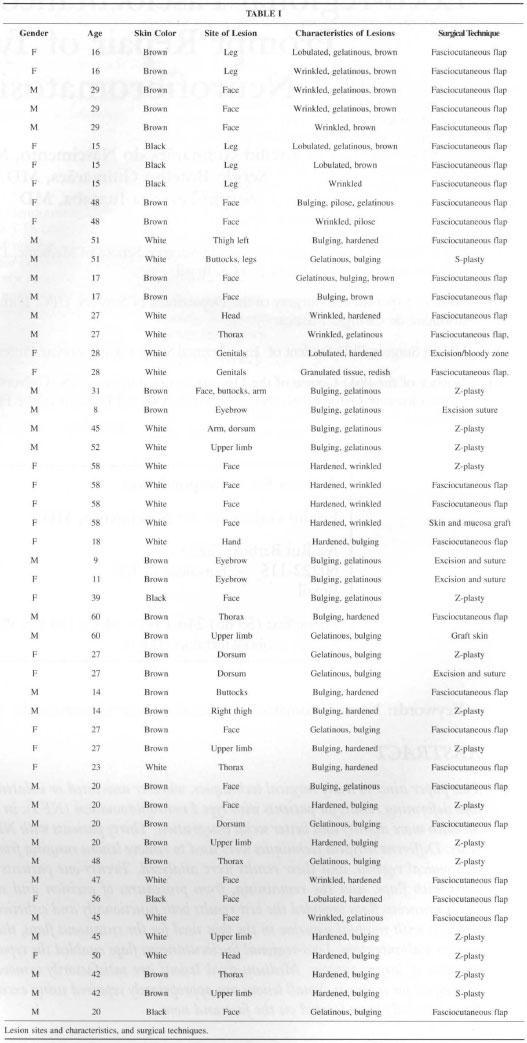
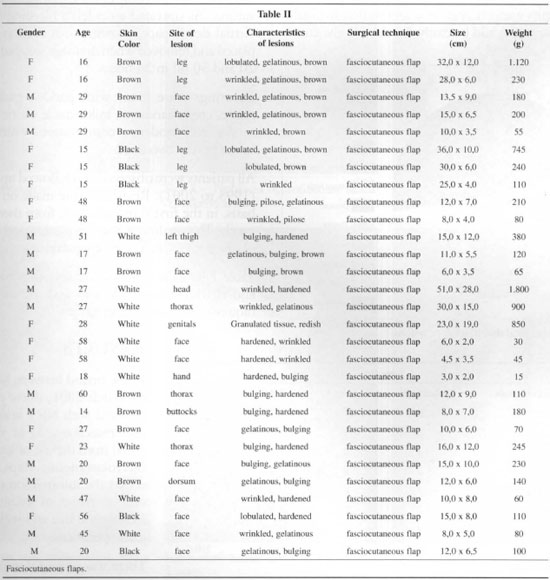
Table I lists dle information about all patients, site and characteristics of lesions and the surgical techniques used in dle 52 resections.
RESULTS
In the period between March 1996 to March 2001, durty patients diagnosed widl NF I underwent tumor resections, 21 of which benefited from dle use of loco-regional fasciocutaneous flaps. Table II shows the information of patients, characteristics of lesions, surgical techniques, size and weight of surgical specimens.
There was universal impairment in 10 cases; upper limbs accounted for 05: 04 of the forearm and arm and 01 on the hand; the cephalic segment accounted for 10: 06 on the face, 01 on the head and 03 on the eyebrow; there were 03 in lower limbs, of which 01 was on the thigh and 02 on the leg; 01 on the buttocks; 04 on the thorax, dorsum 02 and genitals 01. Percentages and their sites are shown in Figure 1.
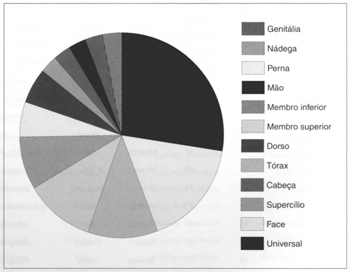
Fig. 1 - Anatomical distribution of lesions.
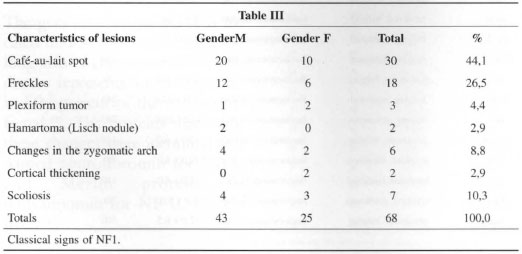
The classical signs of NF I, as well as other lesions that may comprise the picture, are presented in Table III, where it is possible to see the incidence and the percentages fOW1d in the research.
There were plexiform neurofibromas in four cases and in all of them results were considered very good, esthetically, physiologically, and functionally (Figs. 2 to 6).
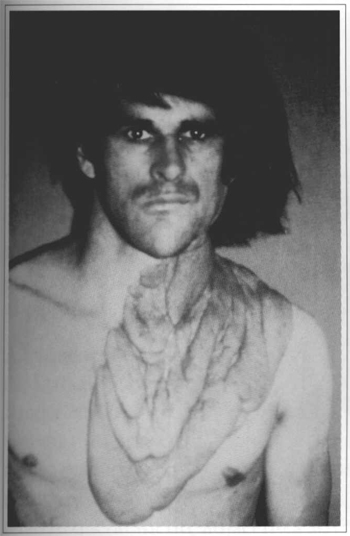
Fig. 2 - Plexiform neurofibroma on the thorax.
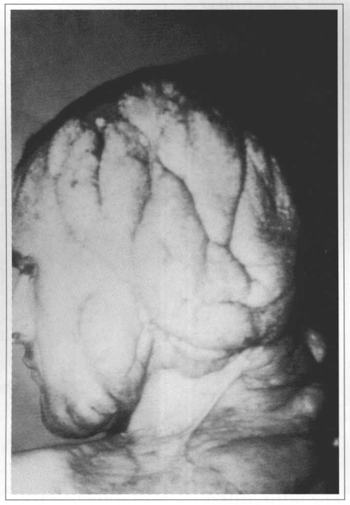
Fig. 3 - Plexiform neurofibroma in the craniocervical area.
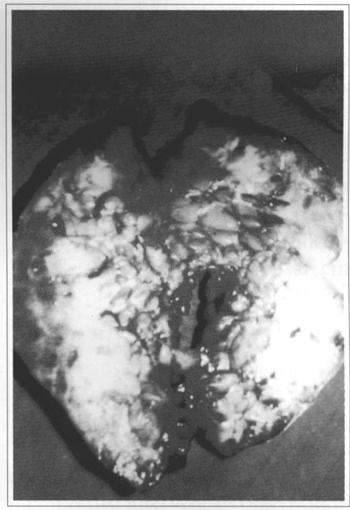
Fig. 4 - Extirpated neurofibromas in the craniocervical region.
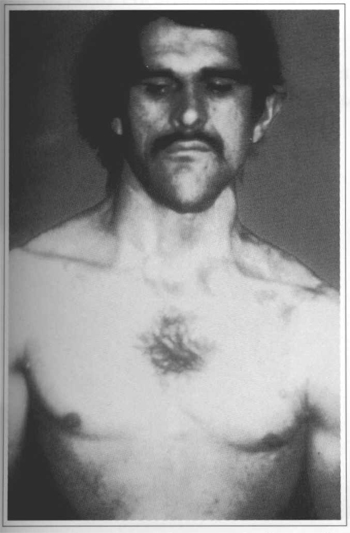
Fig. 5 - Frontal view of fial result after 2 years.
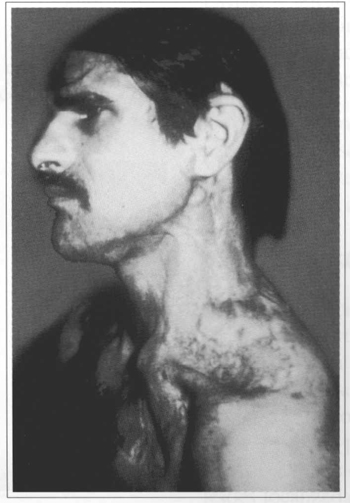
Fig. 6 - Left lateral view of final result after 2 years.
There were three cases in the lower limbs, 1 on the thigh and 2 on the leg, one of them can be assessed in figures 7 to 9. One rare case, affecting the genital area, is shown in figures 10 to 13, in which the tumor affected the suprapubic, pubian and perineal regions.
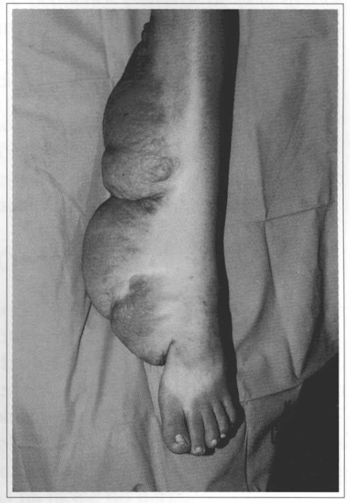
Fig. 7 - Leg left with plexiform neurofibroma; view of tumor.
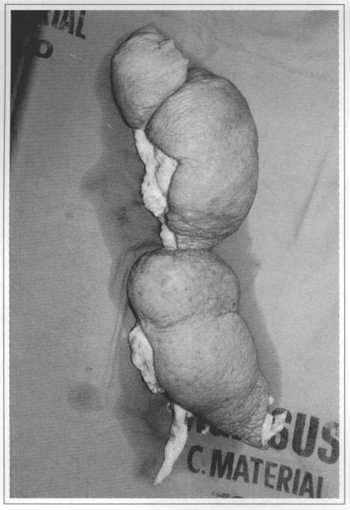
Fig. 8 - Leg left with plexiform neurofibroma; tumor excised.
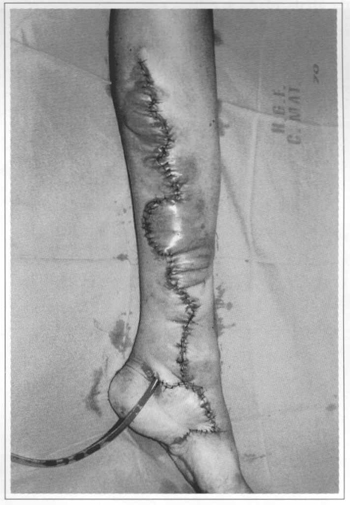
Fig. 9 - Leg left with plexiform neurofibroma; transoperative result.
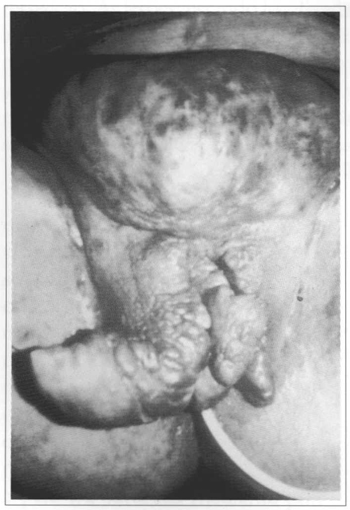
Fig. 10 - Pubian and genitocrural plexiform neurofibroma.
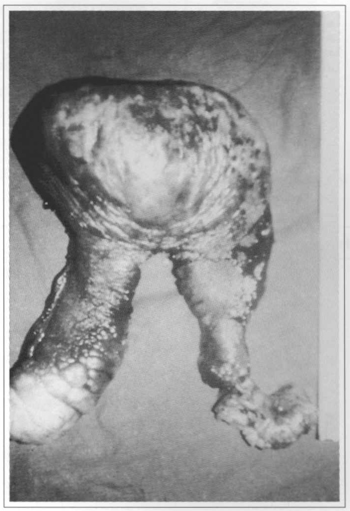
Fig. 11 - Pubian plexiform neurofibroma; extirpated tumor.
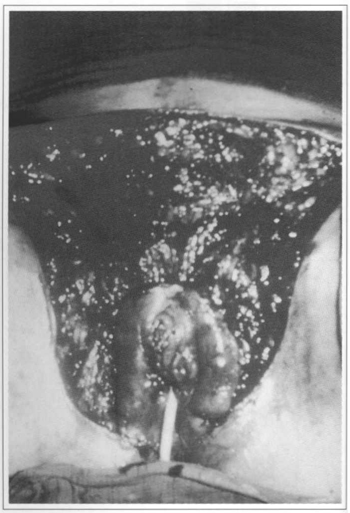
Fig. 12 - Pubian plexiform neurofibroma; bloody rone with transoperative result.
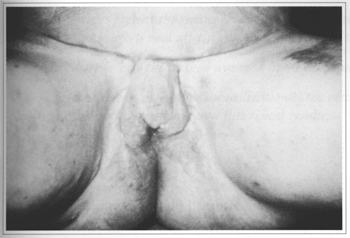
Fig. 13 - Pubian plexiform neurofibroma; result after 18 months.
In the 30 patients the evaluation of scars showed: 18 very good, 9 good, and 3 satisfactory. Pain disappeared in the operated regions in all cases. There was no dehiscence, tissue suffering, infection or necrosis in any of the cases. Scars formed, on average, in 21 days. New tumors were not noticed and there were no relapses.
Of the school age patients, 9 went back to educational activities; an10ng adults, 12 men and 6 women went back to work, and 28 reintegrated into social life.
DISCUSSION
The existence of multiple nemofibromas is one of the defined hallmarks of NF I. Von Recklinghausen's classical description, in 1882, associating NF I to peripheral nerves prevailed for two centuries, and clinical observations provided many indications for the understanding of this pathology.
Papers published by H. Roger (1901), on nervous rumors, and Hosoi (1901), about the malignant degeneration enhanced research.
The frequency of malignization is difficult to be calculated. Daniel, Steward and Capelland (1882), cited by Baudet et al. (1976), believed that surgical intervention would serve as an accelerating factor for malignancy(6); d'Agostinho, Soule and Miller (1963), cited by the same author, claim that sarcomas are often adjacent to nemofibromas(6).
This research did not detect malignization in any of the 52 specimens sent to the laboratory for histopathological examination.
Pitanguy et al. (1983) quote 23 cases about which they say: "Treatment consists of resecting lesions that affect function and/or aesthetics, using smgical techniques so as to correct the deformity", without, however, describing the details of the techniques used, or any postoperative result, merely showing preoperative photos(9).
The present study demonstrated that it is possible to repair large bleeding areas (largest 51.0 x 28.0 cm), with an average of 16.4 x 8.1 cm, resulting from the exeresis of large tLUnors (largest 1,800 g and average 300 g), using loco-regional fasciocutaneous flaps, thus providing adequate cutaneous coverage, given that simple excision, without cutaneous flaps, would make their smgical excision impossible.
The treatment suggested by many authors is linUted to resecting tumors, especially those that affect mental and aesthetic functions, or when they cause pain, discomfort, functional incapacity, or present accelerated growth leading to suspicion of malignant transformation (5,8,9,12,13,15).
Considering that most NF I tumors are benign lesions, it is not justifiable to surgically extirpate noble tissues, like motor and sensory nerves, eyelids and conjunctiva, orbital exenteration or facial bones{l4). Multiple subtotal resections are recommended, so as to avoid futile, hasty interventions aimed at removing lesions totally(15).
Excision and suture and small skin grafts used on smaller lesions and on special sites, like face and nose, permitted complete cutaneous coverage.
S-plasty (average 8.5 x 5.5 cm and 135 g) and z-plasty (for lesions up to 8.5 x 4.8 cm and 82.6 g) proved to be effective in the repair of medium-sized lesions, for which they are one of the choices.
CONCLUSIONS
Loco-regional fasciocutaneous flaps make it possible to resect larger tumors and to adequately repair large bloody areas. Medium-sized lesions can be satisfactorily removed with perfect cutaneous coverage, using either s-plasty or 0 z-plasty. Small lesions can be prompdy resected widl no need of flaps, except for lesions on the face and nose.
REFERENCES
1. Reis CA. Neurology - Neurofibromatosis. 1999. Capturado em 07/12/2002. Disponlvel em http://www.medstudents.com.br/neuro/neuro7.htm.
2. 0ttini L, Esposito DL, Richetta A, Carlesimo M, Palmirotta R, Veri MC, Battista P, Frati L, Caramia FG, Calvieri S. Alterations of microsatellites in neurofibromas of von Recklinghausen's disease. Cancer Res. 1995; 55 (23):5677-80.
3. Baskin KM, Caang J. (1995). Peripheral neurofibromato is. 2000. Capturado em 23/10/2000. Disponlvel em: http://www.vh.org/ProvidersTeachingFiles/RCW/080495/NemoFibroHome.html.
4. Vasguez VL, Lopes A. (1998). Neurofibromatoses e tumores. Acta Oncol Bras. 1998;.18:33-7.
5. Castro CC, Coelho RS, Aboudib Jr JH, Calixto CA, Cupello AMB, Gattorno M. Nemofibromatose - Relato de caso clínico. Rev Soc Bras Cir Plast. 1987; 1(2):55-8.
6. Baudet J, Lemaire JM, Nascimento EG. Les indications chirurgicales dans les neurofibromatoses cutanees.In: XXI Congrés de la Societé Française de Chirurgie Plastique; 1976); Biarritz, França.
7. Dreyfuss U, Ben-Arieth JY, Hirsshowitz B. Liposarcoma: a rare complication in neurofibromatosis. Case report. Plast Reconstr Surg. 1978; 61 (2):287-90.
8. Trevisani TP, Pohl AL, Matloub HS. Neurofibroma of the ear: function and aesthetics. Plast Reconstr Surg. 1982; 70(2):217-9.
9. Pitanguy I, Araujo MTM. Neurofibromatose: Doença de von Recklinghausen. Rev Bras Cir. 1983; (73)1:55-72.
10. Sawada S, Honda M, Kamide R, Niimura M. Three cases of subungual glomus mmors willi von Recklinghausen. J Am Acad Dermatol. 1995; 277:277-8.
11. Fisher DA, Chu P, McCalmont T. Solitary plexiform nemofibroma is not pathognomonic of von Recklinghausen's nemofibromatosis: a report of a case. Int J Dermatol. 1997; 36(6):439-42.
12. Carneiro FRO, Miranda MFR. Nemofibromatose segmentar: apresentação de dois casos. An Bras Dermatol. 1997;.72(3):269-71.
13. Cardoso Filho AF, Lima ALP, Meneses DB. Neurofibrossarcoma de parede tonicica em paciente com neurofibromatose tipo 1. Ceará Med. 2000; 9(1):41-3.
14. Grabb WC, Dingman RO, Oneal RM, Dempsey PD. Facial hematomas in children: nemofibroma, lymphangioma and hemangioma. Plast Reconstr Smg. 1980; 66(4):509-27.
15. Minossi JG, Anefalos A, Spadella CT, Mendes EF, Gonçalves Jr I. Neurofibromatose - Relato de caso. Acta Cir Bras. 2000; 15(3):174-6.
I. MSc in Experimental Surgery of the Department of Surgery, UFC, Fortaleza, CE. Specialist of the Sociedade Brasileira de Cirurgia Plástica. II. MSc in Surgery, PhD Student of Experimental Surgery and Associate Professor of the Depanment of Surgery, UFC.
III. Teacher of the PhD Course of the Department of Surgery of the Universidade Federal do Ceará. PhD in Cancerology by Oxford University (England). General Director of the Hospital do Câncer (Instituto do Câncer do Ceará).
Address for correspondence:
Ercílio Guimarães do Nascimento, MD
Av. Rui Barbosa, 2223
60222-115 - Fortaleza - CE Brazil
Phone/fax: (5585) 246-1541- Mob.: (5585) 9969.0483
e-mail: ercilio@fortalnet.com.br
Stricto Sensu Post-Graduation Program in Surgery, School of Medicine, Department of Surgery of the Universidade Federal do Ceará (UFC), Brasil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter