

Case Report - Year 2022 - Volume 37 -
Propeller flap for reconstruction of sequelae in lower limbs
Retalho em hélice para reconstrução de sequelas em membros inferiores
ABSTRACT
Introduction: The propeller flap is a type of local flap based on perforating vessels. It has several advantages, such as the reconstruction of tissues similar to the original, less morbidity of the donor area, maintenance of the main vessels of the region and the possibility of a wide rotation arc (up to 180º). However, it is subject to complications, the most worrisome being partial or total necrosis of the flap.
Methods: A retrospective study of a series of three cases of lower limb trauma sequelae treated with helix flaps.
Results: Helical flaps reduce surgical time, hospitalization days, and costs. However, they are not free of complications, with partial necrosis occurring in 10.5 to 11% and total necrosis in 1 to 5%. Other complications described are epidermolysis (3.5%) and transient venous congestion (3%). In the cases described, they evolved without complications. Classically, lower limb defects, especially in the distal third, are indicated for reconstruction with microsurgical flaps.
Conclusion: Propeller flaps may be an alternative in these cases, especially in small and moderate defects. There are still no studies directly comparing these two techniques, but some valuable information is already available, such as the similarity between the percentages of total necrosis between the techniques.
Keywords: Flap perforator; lower extremity; Wounds and injuries; Reconstructive surgical procedures; Scar.
RESUMO
Introdução: O retalho em hélice, ou propeller flap, é um tipo de retalho local baseado em vasos perfurantes. Apresenta diversas vantagens, como a reconstrução de tecidos semelhantes ao original, menor morbidade da área doadora, manutenção dos principais vasos da região e a possibilidade de amplo arco de rotação (até 180º). Entretanto, está sujeito a complicações, sendo a mais preocupante a necrose parcial ou total do retalho.
Métodos: Estudo retrospectivo de uma série de três casos de sequelas de trauma em membros inferiores tratados com retalho em hélice.
Resultados: Retalhos em hélice reduzem o tempo cirúrgico, dias de internação e custos. Todavia, não são isentos de complicações, encontra-se a ocorrência de necrose parcial de 10,5 a 11% e total de 1 a 5%. Outras complicações descritas são epidermólise (3,5%) e congestão venosa transitória (3%). Nos casos descritos, evoluíram sem complicações. Classicamente, os defeitos de membro inferior, principalmente no terço distal, têm indicação de reconstrução com retalhos microcirúrgicos.
Conclusão: Os retalhos propeller podem ser uma alternativa nestes casos, principalmente em defeitos pequenos e moderados. Ainda não existem trabalhos comparando diretamente estas duas técnicas, mas algumas informações importantes já estão disponíveis, como a semelhança entre os percentuais de necrose total entre as técnicas.
Palavras-chave: Retalho perfurante; Extremidade inferior; Ferimentos e lesões; Procedimentos cirúrgicos reconstrutivos; Cicatriz
INTRODUCTION
The helical flap, or propeller flap, is a type of local flap based on perforating vessels, defined by the Tokyo Consensus (2011) as “a perforating flap with an island of skin composed of two parts, one larger and one smaller, separated by a nourishing perforating vessel that corresponds to its axis of rotation”1.
It was first described in 1991 by Hyakusoku et al.2, who used an island flap vascularized by perforating vessels with a rotation axis in the vascular pedicle to treat burn sequelae.
This was only possible due to a better understanding of the anatomy and the importance of myocutaneous or septocutaneous perforators. Authors like Donski & Fogdestam3 described that fasciocutaneous flaps that maintained vascularization through perforators could be larger than previously used randomized local flaps. Over time, flaps started to be made with increasingly smaller skin bridges (also known as Keystone flaps) until some surgeons chose to perform island flaps without the skin connection of the pedicle and with rotation arcs each times bigger4.
Since then, propeller-type flaps have become increasingly popular and have several advantages. They are reconstructed with tissues similar to the original defect using neighboring tissues. In general, they present less morbidity in the donor area, often allowing the primary closure of the same. They also allow a large arc of rotation (up to 180o) 5,6. Another advantage is that, especially in reconstructing defects in the distal third of the leg, they can be alternatives to microsurgical flaps, with lower cost, shorter surgical time and without the need for vascular anastomosis7. Despite these advantages, there are still no large clinical trials comparing the two techniques.
Propeller-type flaps are also subject to complications, the most worrisome being partial or total flap necrosis. Other complications described are epidermolysis, transient venous congestion, infection, hematoma, and dehiscence. Risk factors for complications have not yet been fully defined5,6,8.
OBJECTIVE
To present a series of three cases in which the helix flap was used to treat trauma sequelae in the lower limbs.
METHODS
This is a retrospective and descriptive study of patients undergoing reconstruction of lower limb sequelae using a helix flap. The cases were operated on between September 2016 and September 2018 and were subsequently monitored by the Plastic Surgery Department of Escola Paulista de Medicina. Approval was issued by the Research Ethics Committee of the Federal University of São Paulo, under number 0675/2019, and written consent was obtained from all patients.
RESULTS
Case 1
Male patient, 35 years old, a victim of a run-over in 2002, associated with the exposed left tibia and fibula fracture. Initially treated at another service and submitted to external fixation to stabilize the fractures. He underwent a change of fixator for plate and screw in 2003. He evolved in the postoperative period with chronic osteomyelitis, requiring debridement in 2004. After resolving the infectious process, he was also submitted to bone lengthening.
He was referred in 2016 for evaluation by the Plastic Surgery Service of UNIFESP due to an ulcerated lesion in the transition from the middle to the distal third of the anterior face of the left leg, which was difficult to heal (Figure 1). The lesion had granulation tissue, and there were no phlogistic signs. An incisional lesion biopsy was performed, with a negative result for malignancy. He denied smoking, was treated for hypothyroidism and had no other comorbidities.
It was then decided to resect the ulcer and scar area and cover it with a propeller flap. The surgery was performed on 07/06/2016, with the previous mapping of the perforating vessels close to the lesion with a portable Doppler (Figure 1). Planned helical flap based on perforator vessels of the posterior tibial artery, measuring 16x6cm. The flap dissection was in the subfascial plane until the identification of the most caliber perforator close to the lesion.
After careful dissection of the artery, the flap was rotated 180° to cover the defect. The donor area was closed primarily after a negative pressure suction drain was placed. The patient had a good postoperative evolution and was discharged the day after the surgery (Figure 2). There were no complications during follow-up (Figure 2).
Case 2
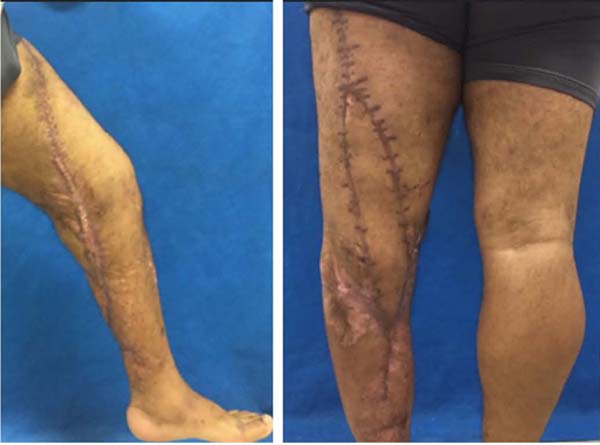
Male patient, 36 years old, without previous comorbidities, non-smoker, a victim of a hit-and-run in 2010. He was attended at another service with severe traumatic brain injury, thoracic trauma, comminuted fracture of the left femur, tibia fracture and extensive soft tissue injury from upper thigh to ankle. He underwent external fixation and two surgical debridements during the same hospital stay. No grafting or flaps were performed to cover the defect, which healed by the second intention.
He was referred in 2016 to the outpatient clinic of the Plastic Surgery Service of UNIFESP. On initial examination, he had extensive scars on the anterior and medial aspect of the thigh, popliteal fossa and medial aspect of the leg. There was also shortening of the left lower limb with genu varum deformity, and restriction in knee movement, in addition to an area of difficult healing in the popliteal fossa (Figure 3).
It was decided to resect the ulcerated area and cover it with a propeller flap, in addition to correcting an unsightly scar on the thigh. The surgery was performed on 07/22/2016, with a portable Doppler device mapping the perforators close to the lesion (Figure 3). Two perforators of the deep femoral artery were chosen, with a planned flap measuring 27x6cm. Surgery started with an incision on the lateral face of the flap and subfascial dissection until the two previously mapped vessels were identified. It was decided to keep the larger caliber closer to the defect. After carefully dissecting the pedicle, the remainder of the flap was released and rotated 180° to cover the defect. The donor area was closed primarily after a negative pressure suction drain was placed.
The patient presented partial dehiscence of the operative wound (Figure 4). Debridement and resuture were performed on 08/02/2016. There was a good evolution, with no other complications during follow-up (Figure 5).
Case 3
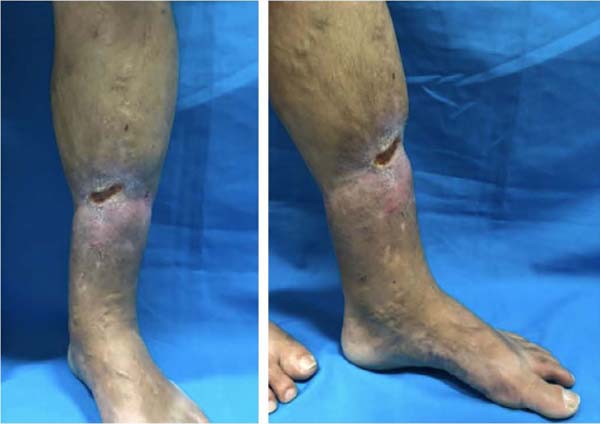
Male patient, 47 years old, with arterial hypertension, smoker, a victim of a car-motorcycle collision in 2017. He was attended at another service with an exposed fracture of the tibia and fibula and degloving of the anterior region of the middle third of the left leg. He underwent external fixation and, during the same hospitalization, surgical debridement and primary synthesis of the skin defect by the orthopedic team. He evolved with a chronic ulcer.
He was referred in 2018 to the outpatient clinic of the Plastic Surgery Service of UNIFESP. On initial examination, he had a chronic ulcerated lesion on the middle third of the anterior face of the left leg (Figure 6). The lesion had granulation tissue, and there were no phlogistic signs. An incisional lesion biopsy was performed, with a negative result for malignancy.
It was decided to resect the ulcerated area and cover it with a propeller flap. The surgery was performed on 09/28/2018, with the previous mapping of the posterior tibial perforators close to the lesion using a portable Doppler device (Figure 7). After carefully dissecting the pedicle, the helical flap was released and rotated 90° to cover the defect (Figure 7). The donor area was closed primarily after the placement of a negative pressure suction drain (Figure 7).
The patient evolved without complications during follow-up (Figure 8).
DISCUSSION
Helix flaps are a relatively recent and very promising concept, especially in challenging areas such as lower limb reconstruction, as demonstrated in the cases described here. These are flaps capable of reconstructing defects with similar tissues and low morbidity in the donor area, preserving the region’s main vessels and reducing surgical and hospitalization time.
Despite these advantages, they are not without complications. In a literature review performed by Gir et al.5, the occurrence of partial necrosis was 11%, and total necrosis was 1%. Nelson et al.6 found 11% partial and 5% total necrosis. In this same study, 82.9% of the flaps had no complications. A meta-analysis and systematic review, published in 2016 by Bekara et al.8, also reached similar results: 10.5% for partial and 3.5% for total necrosis. Other complications described were epidermolysis (3.5%) and transient venous congestion (3%).
In these studies, the flap rotation arc and the dissection plane (sub or suprafascial) were not associated with the occurrence of complications. In the cases reported here, there was no partial or total necrosis of the flaps, but one of them evolved with partial dehiscence of the surgical wound. Nevertheless, the case evolved very well in the postoperative period, allowing the patient to undergo femoral bone stretching by the orthopedic team without compromising the skin island of the flap.
Classically, lower limb defects, especially in the distal third, are indicated for reconstruction with microsurgical flaps. Propeller flaps can be a less complex alternative in these cases, especially in minor and moderate defects. There are still no works directly comparing these two techniques, but some important information is already available. Wu et al.9 reported a series of 2019 free flaps, with 3.8% of total necrosis and 10% of cases requiring revision procedures or major surgeries. These rates are very similar to those found in the large studies on helix flaps described to date.
One of this surgical technique’s main pillars concerns the pedicle’s rotation up to 180° without compromising its patency. Some experimental studies were conducted to investigate this fact, with contradictory results. Wong et al.10 studied the factors that affect vessel patency in a virtual model. It was observed that the angle of rotation should be a maximum of 180°, the blood pressure should be kept constant during the surgery, and the pedicle diameter should be approximately 1 mm and its length greater than 30 mm. Demir et al.11 and Izquierdo et al.12 also reported that torsion of up to 180° in the pedicle does not affect its patency. On the other hand, Tos et al.13, in an experimental study, demonstrated that rotations of up to 90° could compromise the flow of vessels with microsurgical anastomoses.
Another point still under discussion is the maximum size of the flap. Saint-Cyr et al.14 described the “perforasome” theory, suggesting that perforating flaps may increase their vascularization area by opening communicating vessels with adjacent territories. According to this study, it is not easy to define the safe size for a flap in cadaveric studies, as this compensatory mechanism would only occur in vivo14. In the meta-analysis and systematic review of Bekara et al.8, flap size >100cm2 was not a risk factor for complications. Innocenti et al.15 analyzed 74 cases and found no difference in the number of complications between 5-14cm and 15-25cm flaps.
In the reported series, two cases had the maximum possible rotation of the pedicle (180°) without impairment of vascularization or venous congestion, and one with 90° rotation without vascular damage. The largest flap, measuring 27x6cm, may have evolved with partial dehiscence due to tension in the region and because it was a flexor area in the popliteal region.
As a diagnostic method, most studies use portable acoustic Doppler to map the perforators8. This method successfully identifies vessels in up to 80% of cases16. Its main advantages are practicality, low cost and the possibility of intraoperative use. As a limitation, we can mention the impossibility of mapping perforators at depths greater than 20 mm, not determining the caliber of vessels and their flow, and confusing the perforators with other vessels.
Another available imaging test is color Doppler ultrasound, whose main convenience is obtaining vessel diameter and flow information. However, it depends on an experienced examiner and takes longer than other alternatives.
Computed tomography angiography is a method that has advanced a lot in recent years, which makes it possible to identify perforators from 0.3 to 0.5 mm, in addition to evaluating their size, location and three-dimensional path with high sensitivity and specificity. The main disadvantages are contrast, ionizing radiation and higher cost. Magnetic resonance imaging can also be used, although some studies point to reduced accuracy in diagnosing perforators with a diameter smaller than 1 mm17. This study used only portable acoustic Doppler without difficulty identifying the perforators.
In addition to factors related to technique and surgical planning, the patient’s clinical factors can influence the final result. In the study published by Bekara et al.8, age over 60 years (RR=1.61; p=0.03), arteriopathy (RR=3.12; p=0.01) and diabetes (RR=2, 0; p=0.02) were associated with a higher risk of adverse events. On the other hand, smoking did not reach statistical significance as a risk factor, with a relative risk of 1.96 (0.99 to 3.90 in the 95% confidence interval) and p=0.068. The patients in this study were non-smokers, and two had comorbidities (hypothyroidism and arterial hypertension).
CONCLUSION
Helix flaps are a good option for covering defects in the lower limbs. The cases described here had good postoperative results without serious complications.
REFERENCES
1. Pignatti M, Ogawa R, Hallock GG, Mateev M, Georgescu AV, Balakrishnan G, et al. The “Tokyo” consensus on propeller flaps. Plast Reconstr Surg. 2011;127(2):716-22. PMID: 21285776 DOI: https://doi.org/10.1097/PRS.0b013e3181fed6b2
2. Hyakusoku H, Yamamoto T, Fumiiri M. The propeller flap method. Br J Plast Surg. 1991;44(1):53-4. PMID: 1993239 DOI: https://doi.org/10.1016/0007-1226(91)90179-N
3. Donski PK, Fogdestam I. Distally based fasciocutaneous flap from the sural region. A preliminary report. Scand J Plast Reconstr Surg. 1983;17(3):191-6. PMID: 6673085
4. el-Saadi MM, Khashaba AA. Three anteromedial fasciocutaneous leg island flaps for covering defects of the lower two-thirds of the leg. Br J Plast Surg. 1990;43(5):536-40. PMID: 2224347 DOI: https://doi.org/10.1016/0007-1226(90)90116-H
5. Gir P, Cheng A, Oni G, Mojallal A, Saint-Cyr M. Pedicled-perforator (propeller) flaps in lower extremity defects: a systematic review. J Reconstr Microsurg. 2012;28:595-601. PMID: 22715046 DOI: https://doi.org/10.1055/s-0032-1315786
6. Nelson JA, Fischer J P, Brazio PS, Kovach SJ, Rosson GD, Rad AN. A review of propeller flaps for distal lower extremity soft tissue reconstruction: Is flap loss too high? Microsurgery. 2013;33:578-86. PMID: 23861186 DOI: https://doi.org/10.1002/micr.22134
7. Rad AN, Singh NK, Rosson GD. Peroneal artery perforator-based propeller flap reconstruction of the lateral distal lower extremity after tumor extirpation: case report and literature review. Microsurgery. 2008;28(8):663-70. PMID: 18846577 DOI: https://doi.org/10.1002/micr.20557
8. Bekara F, Herlin C, Mojallal A, Sinna R, Ayestaray B, Letois F, et al. A Systematic Review and Meta-Analysis of Perforator-Pedicled Propeller Flaps in Lower Extremity Defects: Identification of Risk Factors for Complications. Plast Reconstr Surg. 2016;137(1):314-31. PMID: 26371391 DOI: https://doi.org/10.1097/PRS.0000000000001891
9. Wu CC, Lin PY, Chew KY, Kuo YR. Free tissue transfers in head and neck reconstruction: complications, outcomes and strategies for management of flap failure: analysis of 2019 flaps in single institute. Microsurgery. 2014;34(5):339-44. PMID: 24318866 DOI: https://doi.org/10.1002/micr.22212
10. Wong CH, Cui F, Tan BK, Liu Z, Lee H P, Lu C, et al. Nonlinear finite element simulations to elucidate the determinants of perforator patency in propeller flaps. Ann Plast Surg. 2007;59(6):672-8. PMID: 18046151 DOI: https://doi.org/10.1097/SAP.0b013e31803df4e9
11. Demir A, Acar M, Yldz L, Karacalar A. The effect of twisting on perforator flap viability: An experimental study in rats. Ann Plast Surg. 2006;56(2):186-9. PMID: 16432329 DOI: https://doi.org/10.1097/01.sap.0000196561.92828.d7
12. Izquierdo R, Dobrin PB, Fu K, Park F, Galante G. The effect of twist on microvascular anastomotic patency and angiographic luminal dimensions. J Surg Res. 1998;78(1):60-3. PMID: 9733619 DOI: https://doi.org/10.1006/jsre.1997.5228
13. Tos P, Innocenti M, Artiaco S, Antonini A, Delcroix L, Geuna S, et al. Perforator-based propeller flaps treating loss of substance in the lower limb. J Orthop Traumatol. 2011;12(2):93-9. PMID: 21544548 DOI: https://doi.org/10.1007/s10195-011-0136-0
14. Saint-Cyr M, Schaverien M, Arbique G, Hatef D, Brown SA, Rohrich RJ. Three- and four-dimensional computed tomographic angiography and venography for the investigation of the vascular anatomy and perfusion of perforator flaps. Plast Reconstr Surg. 2008;121(3):772-80. PMID: 18317127 DOI: https://doi.org/10.1097/01.prs.0000299338.97612.90
15. Innocenti M, Menichini G, Baldrighi C, Delcroix L, Vignini L, Tos P. Are there risk factors for complications of perforator-based propeller flaps for lower-extremity reconstruction? Clin Orthop Relat Res. 2014;472(7):2276-86. PMID: 24706021 DOI: https://doi.org/10.1007/s11999-014-3537-6
16. Rand R P, Cramer MM, Strandness DE Jr. Color-flow duplex scanning in the preoperative assessment of TRAM flap perforators: a report of 32 consecutive patients. Plast Reconstr Surg. 1994;93(3):453-9. PMID: 8115499 DOI: https://doi.org/10.1097/00006534-199493030-00001
17. Ono S, Hayashi H, Ohi H, Ogawa R. Imaging Studies for Preoperative Planning of Perforator Flaps: An Overview. Clin Plast Surg. 2017;44(1):21-30. PMID: 27894580 DOI: https://doi.org/10.1016/j.cps.2016.09.004
1. Universidade Federal de São Paulo, São Paulo, SP, Brazil.
Corresponding author: Roney Gonçalves Fechine Feitosa Rua Botucatu, 740, 2º andar, São Paulo, S P, Brazil Zip Code: 04023-900 E-mail: roneyfechine@gmail.com
Article received: May 20, 2021.
Article accepted: July 14, 2021.
Conflicts of interest: none.
Institution: Universidade Federal de São Paulo, Escola Paulista de Medicina, São Paulo, SP, Brazil.

















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter