

Original Article - Year 2022 - Volume 37 -
Non-melanoma skin tumors: a retrospective study of the epidemiological profile and outcome from compromised margins
Tumores de pele não melanoma: estudo retrospectivo do perfil epidemiológico e desfecho a partir de margens comprometidas
ABSTRACT
Introduction: Non-melanoma skin neoplasms are responsible for 30% of all malignant tumors in Brazil. The main objective of this article was to evaluate the epidemiological profile and the approach taken from the histopathological diagnosis of compromised margins in patients with non-melanoma skin neoplasms treated primarily with surgery.
Methods: This is an observational retrospective cohort. Data were collected from electronic medical records of 1495 patients, resulting in 2457 non-melanoma skin neoplasms, from January 2015 to December 2019.
Results: There was a higher prevalence in men (52.4%) and between the sixth and seventh decades of life ( 41.4%). Basal cell carcinoma was the most common histological type (75%). Those over the age of 61 are 57.2% more likely to develop basal cell carcinoma (relative risk=1,572 (95% CI: 1,316-1,878; p<0. 0001). Compromised margins were reported in 15.8% of cases, being more common on the face (19.5%) and in patients with basal cell carcinoma (p<0.05), with relative risk=1,382 (95%CI: 1,135-1,683; p=0.0013). Additional treatment was indicated in 74.6% of cases, with the most common approaches being margin expansion (55.6%) and radiotherapy (42.4%). The choice between intervention or observation was related to the histological type (p<0.05), but it was not possible to affirm its relationship with the age group (p>0.05).
Conclusion: The study allowed a better understanding of the profile of patients with non-melanoma skin neoplasms and the percentage of compromised margins after initial surgical excision and the treatment performed.
Keywords: Skin neoplasms; Carcinoma, basal cell; Carcinoma, basosquamous; Epidemiology; Margins of excision.
RESUMO
Introdução: Os carcinomas de pele do tipo não melanoma são responsáveis por 30% dos tumores malignos no Brasil. O objetivo deste artigo foi avaliar o perfil epidemiológico e a conduta tomada a partir do diagnóstico histopatológico de margens comprometidas em pacientes com carcinomas de pele do tipo não melanoma tratados primariamente com cirurgia.
Métodos: Estudo tipo coorte retrospectivo observacional. Os dados foram coletados de prontuário eletrônico de 1495 pacientes, apresentando 2457 carcinomas de pele do tipo não melanoma, operados entre janeiro de 2015 a dezembro de 2019.
Resultados: Houve maior prevalência em homens (52,4%) e entre a sexta e a sétima décadas de vida (41,1%). O carcinoma basocelular foi o tipo histológico mais comum (75%). O risco de desenvolver carcinoma espinocelular foi 57,2% maior em pacientes com idade acima de 61 anos (risco relativo=1,572 (IC 95%: 1,316-1,878; p<0,0001)). Margens comprometidas foram reportadas em 15,8% dos casos, sendo mais comuns na face (19,5%) e nos pacientes com carcinoma espinocelular (p<0,05), com risco relativo=1,382 (IC95%:1,135-1,683; p=0,0013). Tratamento adicional foi indicado em 74,6% dos casos, sendo as condutas mais comuns a ampliação de margens (55,6%) e radioterapia (42,4%). A escolha entre intervenção ou observação apresentou relação com o tipo histológico (p<0,05), porém não foi possível afirmar sua relação com a faixa etária (p>0,05).
Conclusão: O estudo possibilitou melhor compreensão do perfil dos pacientes com carcinomas de pele do tipo não melanoma, bem como o percentual de margens comprometidas após excisão cirúrgica inicial e o tratamento realizado.
Palavras-chave: Neoplasias cutâneas; Carcinoma basocelular; Carcinoma basoescamoso; Epidemiologia; Margens de excisão
INTRODUCTION
Non-melanoma skin carcinomas (NMSC) are responsible for 30% of malignant tumors registered in Brazil1. Basal cell carcinoma (BCC) is the most common subtype, accounting for 70% to 80% of cases. Squamous cell carcinoma (SCC) is the second most prevalent subtype and has a more aggressive behavior when compared to BCC2, 3.
Lesions arise preferably in segments with greater exposure to solar radiation, such as the head, neck, trunk and upper limbs. Phototype, family history, immunosuppression and exposure to chemicals and radiotherapy are risk factors for the development of these tumors, which demonstrates their multifactorial etiology resulting from genetic alterations, environmental factors and lifestyle4.
The ideal treatment for NMSC consists of surgical excision with free margins. Cases with compromised margins are associated with greater morbidity and may require additional management, such as margin expansion or radiotherapy, depending on the characteristics of the lesion and the individual5.
OBJECTIVE
This study aims to evaluate the management of the anatomopathological finding of compromised margins, in addition to describing the epidemiological profile of patients undergoing surgical excision of NMSC in the surgery service of Hospital Municipal São José de Joinville - SC.
METHODS
Study design
This is an observational, retrospective cohort study of a descriptive nature about the approaches adopted in the face of compromised margins in the anatomopathological study of non-melanoma skin tumors at Hospital Municipal São José, Joinville-SC. The present study was evaluated by the Research Ethics Committee (CEP) of Hospital Municipal São José and approved under opinion 4,388,189, and carried out according to the guidelines established in Resolution 466/2012 of the National Health Council.
Study population
All patients who underwent primary excision of non-melanoma skin neoplasms, aged over 18 years, from January 2015 to December 2019 were included. The study did not include patients with incomplete medical records for the variables analyzed.
Variables analyzed
Data were collected through the electronic medical record, and the following information was analyzed: epidemiological profile (sex, age and color), location of the lesion, anatomopathological analysis (histological type and surgical margins) and additional management after anatomopathological evaluation.
Statistical analysis
Categorical variables were reported through absolute, relative and percentage. Bivariate analysis was performed using Pearson’s chi-square test to certify the association between categorical variables. The significance level was set at 5% (p<0.05). Data analysis was performed using IBM SPSS statistics version 23. Such analyzes are presented through tables and graphs.
RESULTS
We analyzed 2457 non-melanoma skin tumors submitted to surgical excision between January 2015 and December 2019, resulting in a sample of 1459 patients. Among the patients, there was a slight predominance of males (52.4%) and a prevalence of white color/ethnicity (99.5%). Regarding age, 70% were over 61, predominating the age group from 61 to 75 (41.1%) (Table 1).
| Patient profile analysis (n=1459) | |
|---|---|
| Sex | |
| Male | 52.4% (765) |
| Color | |
| White | 99.5% (1452) |
| Brown | 0.5% (07) |
| Age range (years) | |
| 18 to 30 | 0.5% (7) |
| 31 to 45 | 5.2% (76) |
| 46 to 60 | 24.3% (354) |
| 61 to 75 | 41.1% (600) |
| 76 to 90 | 26.8% (391) |
| 91 to 105 | 2.1% (31) |
Basal cell carcinoma was more prevalent, with 75.0% of cases (n=1845), followed by squamous cell carcinoma, with 23.7% (n=582), and basal squamous carcinoma, with 1.2% (n=582) (n=30).
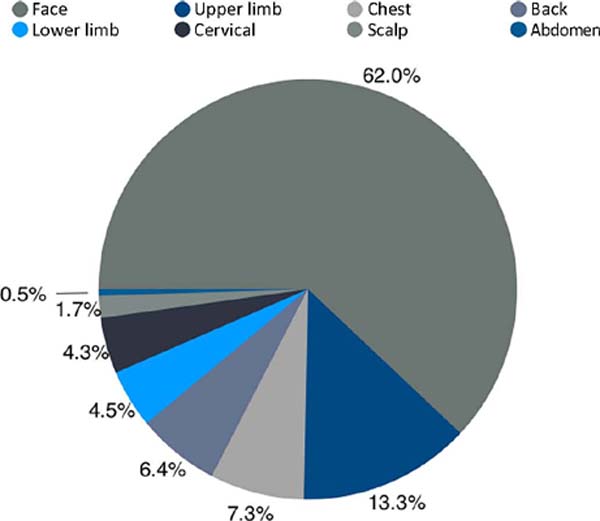
The face was the most affected location (62%, n=1525), followed by the upper limbs (13.3%, n=328), accounting for more than 75% of the lesions (Figure 1).
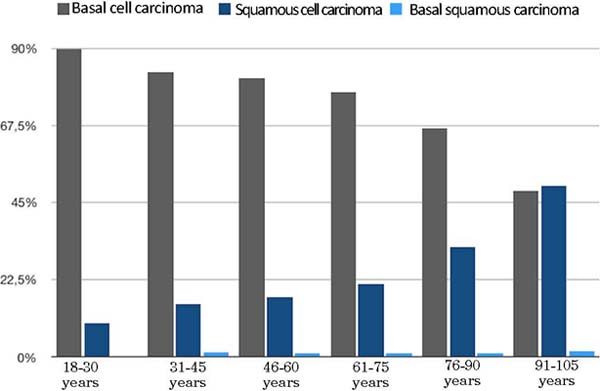
When analyzing the distribution of the histological type by age group, as shown in Figure 2, it is possible to see that basal cell carcinoma was the most common subtype in all age groups up to 90 years. Only between 91-105 years of age did squamous cell carcinoma present a higher prevalence.
The anatomopathological study showed free surgical margins in 84.2% of the cases. In the analysis of surgical margins by age group, it can be seen that there was a higher percentage of free margins among individuals aged 18 to 30 years (90%) and a lower proportion among those aged 91 to 105 years (75.8%) (Table 2).
| Age group | Free margins | Compromised margins | Total |
|---|---|---|---|
| 18 to 30 years | 9 (90%) | 1 (10%) | 10 |
| 31 to 45 years | 113 (86.9%) | 17 (13.1%) | 130 |
| 46 to 60 years | 509 (85%) | 90 (15%) | 599 |
| 61 to 75 years | 822 (84.5%) | 151 (15.5%) | 973 |
| 76 to 90 years | 568 (83.2%) | 115 (16.8%) | 683 |
| 91 to 105 years | 47 (75.8%) | 15 (24.2%) | 62 |
| Total | 2068 (84.2%) | 389 (15.8%) | 2457 (100%) |
When analyzing the surgical margins between the two main histological types, a greater number of free margins is identified in basal cell carcinoma (85.6%) compared to squamous cell carcinoma (80%).
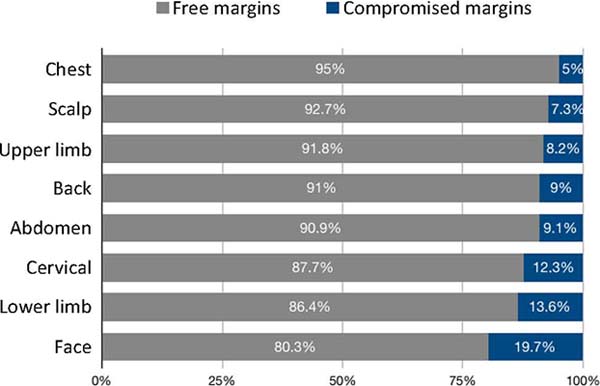
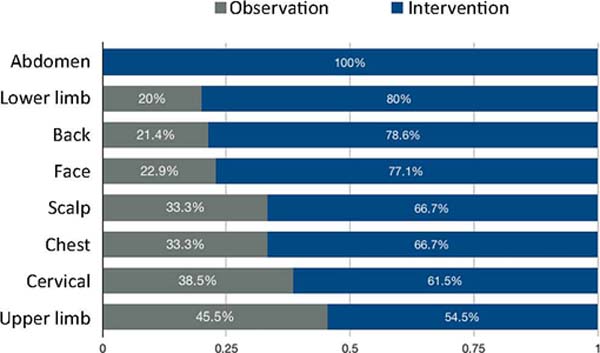
Relating compromised margins and the location of the lesion, we noticed that the site with the highest incidence was the face (19.7%), followed by the lower limbs (13.6%), with the chest being the site with the lowest incidence (5%). (Figure 3).
Regarding the conduct adopted after evidence of compromised margins, observation was chosen in 21.8% of the cases, and in 74.6%, a new intervention was indicated. There was a loss to follow-up in 3.5% of patients with compromised margins. When these patients are not counted, we have a rate of 77.3% of intervention and 22.7% of observation. Individuals with basal cell carcinoma were the ones who underwent intervention the most (79.4%), followed by squamous cell carcinoma (65.5%) (Table 3).
| Carcinoma basal cell | Histological type Carcinoma spinocellular | Carcinoma Basosquamous | Total | |
|---|---|---|---|---|
| Observation | 49 (18.3%) | 34 (29.3%) | 2 (33.3%) | 85 (21.8%) |
| Intervention | 212 (79.4%) | 76 (65.5%) | 2 (33.3%) | 290 (74.6%) |
| Tracking loss | 6 (2.3%) | 6 (5.2%) | 2 (33.3%) | 14 (3.6%) |
| Total | 267 | 267 | 6 | 389 (100%) |
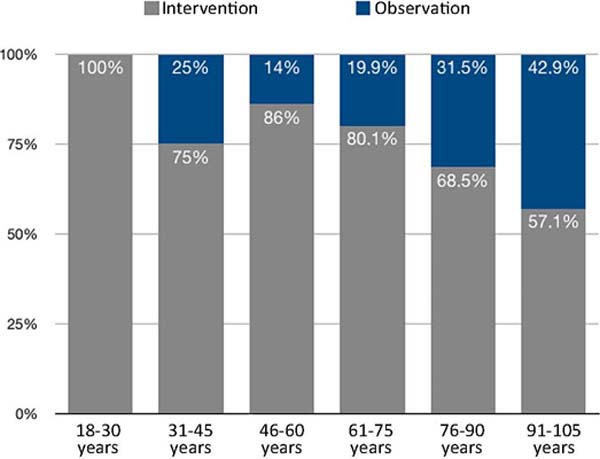
Figure 4 analyzes only the observational versus interventional conduct at different ages. From the age of 46, there is a decrease in intervention rates, with an increase in observation rates, and among individuals aged 18 to 30 years, there is a 100% intervention rate. The oldest, between 91 and 105 years, had the highest percentage of observation among age groups (42.9%).
The main interventions performed were widening the margins (55.6%) and radiotherapy (42.4%). Analyzing the interventions by age group, it appears that widening the margins was the intervention of choice for most individuals in almost all age groups, except between 76 and 90 years, in which radiotherapy was more prevalent (Table 4).
| Age group | Total | ||||||
|---|---|---|---|---|---|---|---|
| 18 to 30 years | 31 to 45 years | 46 to 60 years | 61 to 75 years | 76 to 90 years | 91 to 105 years | ||
| Magnification | 1 (100%) | 7 (58.3%) | 45 (60.8%) | 69 (57%) | 34 (46%) | 5 (62.5%) | 161 (55.6%) |
| Radiotherapy | 0 | 5 (41.7%) | 26 (35.2%) | 51 (42.2%) | 38 (51.4%) | 3 (37.5%) | 123 (42.4%) |
| Magnification + radiotherapy | 0 | 0 | 1 (1.3%) | 1 (0.8%) | 1 (1.3%) | 0 | 3 (1%) |
| Cryotherapy | 0 | 0 | 2 (2.7%) | 0 | 1 (1.3%) | 0 | 3 (1%) |
| Total | 1 | 12 | 74 | 121 | 74 | 8 | 290 (100%) |
When relating the conduct in the face of the finding of compromised margins according to the location of the lesion, we observed that the option to intervene was always more prevalent. In the case of abdominal injuries, this option occurred in 100% of the cases (Figure 5).
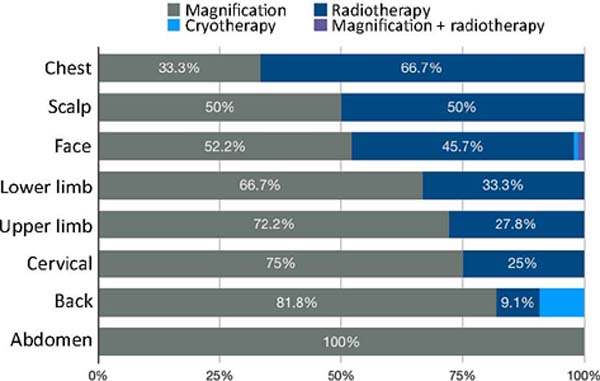
The most prevalent type of intervention in the abdomen, back, neck and limbs was margin enlargement, while the face and scalp showed similar rates between enlargement and radiotherapy. The chest was the only topography where radiotherapy was the most frequent intervention (Figure 6).
Of the 161 patients who underwent a new surgical approach to widen the margins, it was possible to analyze the anatomopathological results of 157, with 49.7% of these individuals having a tumor-free sample and 38.2% free margins and 12.1% with compromised margins. Of the latter who maintained compromised margins, 47.4% were kept under observation, 36.8% were referred for radiotherapy, 10.5% were indicated for further enlargement, and 5.3% were lost to follow-up.
Pearson’s chi-square test was performed to identify whether there was a statistically relevant relationship between the variables of age, surgical margins, management and the histological type of the neoplasm. It was found that age above 61 years is related to the histological type of squamous cells (p<0.05), with a relative risk (RR) of 1.572 (95%CI: 1.316-1.878; p<0.0001), but not with the presence of compromised margins (p=0.4). Squamous cell carcinoma is more related to the presence of compromised margins (p<0.05), with a relative risk of 1.382 (95%CI: 1.135-1.683; p=0.0013). The choice between intervention or observation was related to the histological type (p<0.05), but it was not possible to affirm its relationship with the age group (p>0.05).
DISCUSSION
Non-melanoma skin carcinomas are considered a public health problem in Brazil due to their high prevalence and incidence. The South region has the highest number of cases due to the predominance of Fitzpatrick skin phototypes I, II and III, which are more vulnerable to sun exposure6, 7. In the present study, this fact was confirmed due to the majority presence of these phototypes, corresponding to 99.5% of the patients in the evaluated sample.
We observed a higher prevalence of BCC (75%) concerning SCC (23.7%), which agrees with the literature2, 8. Unlike the distribution between sexes, in which most studies present it as more prevalent in women, in our study, it was more prevalent in males (52.4%)3, 7, 9. We hypothesize that men in this region have greater exposure to UV rays, mainly rural workers since this is the main risk factor for developing NMSC3, 4, 7, 9. This risk factor is also related to the lesions located mainly in photoexposed areas3, 7. This study proved that to be true, with more than 75% of injuries to the face (62.0%) and upper limbs (13.3%).
Regarding the age group with the highest overall prevalence of CNPM, our study revealed a predominance of the number of cases between the sixth and seventh decades of life8. In this group, there was also a higher incidence of SCC, and in the age group of 91-105 years, the incidence of SCC surpassed that of BCC. Overall, our study showed that the population aged 61 years and over is 57.2% (RR=1.572 (95% CI: 1.316-1.878; p<0.0001)) more likely to develop SCC than younger individuals. This can be explained by the fact that the main risk factor for the development of SCC is cumulative sun exposure, which is proportional to the age of the individual7.
When evaluating free and compromised margins after surgical excision of the lesions, 84.2% of the samples in our study resulted in free margins without the need for additional management. In 15.8% of the cases, the margins were compromised. These results were similar to those found in other studies3, 10, 11. The highest rate of compromised margins was in the age group from 91 to 105 years old. We believe the higher incidence of SCC can explain this in this population. Studies by Gutjahr et al.10 and Quintas & Coutinho11 point to greater invasiveness of the SCC when compared to the SCC as a factor that leads to higher rates of compromised margins. This was also clear in our study, in which the relative risk of SCC with compromised margins was RR=1.382 (95% CI: 1.135¬1.683; p=0.0013), that is, 38.2% more than the probability that the CBC.
Regarding the conduct performed after evidence of compromised margins, 74.6% of the studied sample had a new approach, among which the expansion of margins (55.6%) and referral to radiotherapy (42.4%) were the main, which goes against the results of the study by Fidelis et al.5, in which clinical follow-up was the therapy of choice in 60.8% of the cases. Enlargement was the preferred approach for patients aged 18-30, performed in 100% of those with compromised margins. This rate was lower in patients aged 91-105 years, with only 62.5% of them undergoing enlargement. In those patients aged 76-90 years, radiotherapy was the most indicated therapy, reaching 51.4% of the population.
The observational approach was adopted in 21.8% of the sample, which was also seen in other studies, such as those by Fidelis et al.5 and Ocanha et al.12. The expectant management adopted in our service could be explained by increasing the age of the patients, as evidenced by Fidelis et al.5, in which elderly patients make clinical follow-up acceptable in cases of compromised surgical margins. Despite this, our study showed that the choice of conduct in the population evaluated was not related to age (p=1.177) or the histological type of tumor (p=0.285).
When evaluating the intervention chosen due to compromised margins according to the location of the lesion, we observed that the face and scalp were the locations where radiotherapy and surgical enlargement had similar rates (52.2% x 45.7% and 50% x 50%). The chest was the only location where radiotherapy was more indicated (66.7%); in the others, surgical excision was preferred (66.7% - 100%). In this study, it was possible to assess that lesions on the face had a high intervention rate (77.1%), which can be explained by the higher photoexposure and high risk of recurrence. Concern about the possible growth of the lesion and greater difficulty for future resections and reconstructions may explain the higher rates of intervention on the face3, 5, 7, 8, 12.
CONCLUSION
With the present study, data were found that allow a better understanding of the profile of patients with NMSC, as well as the percentage of compromised margins after initial surgical excision and the measures taken based on the histopathological result. The location of the lesion and the histological type are relevant factors in defining the subsequent treatment; however, more studies are needed to elucidate the risk factors related to the presence of compromised margins.
REFERENCES
1. Brasil. Ministério da Saúde. Instituto Nacional do Câncer José Alencar Gomes da Silva (INCA). Estimativa 2020: Incidência de Câncer no Brasil. Rio de Janeiro: INCA; 2020. Disponível em: https://www.inca.gov.br/sites/ufu.sti.inca.local/files/media/document/estimativa-2020-incidencia-de-cancer-no-brasil.pdf
2. Leiter U, Eigentler T, Garbe C. Epidemiology of skin cancer. Adv Exp Med Biol. 2014;810:120-40.
3. Benedet L, Bastos MF, Teixeira JF, Miranda L F, Bolan R. Avaliação clínica e histopatológica dos pacientes portadores de carcinoma basocelular diagnosticados no instituto de diagnóstico anátomopatológico em Florianópolis - SC de janeiro a fevereiro de 2004. ACM Arq Catarin Med. 2007;36(1):37-44.
4. Barucci FMP, Vetorasso GH, Cardoso CA, Priante AVM. Perfil e características anatomopatológicas em 100 pacientes com câncer de pele não melanoma. Rev Bras Cir Cabeça Pescoço. 2015;44(3):124-9.
5. Fidelis MC, Stelini RF, Staffa LP, Moraes AM, Magalhães RF. Basal cell carcinoma with compromised margins: retrospective study of management, evolution, and prognosis. An Bras Dermatol. 2021;96(1):17-26.
6. Imanichi D, Gasparello Filho JL, Moraes C F, Sotero RC, Gomes LO. Fatores de risco do câncer não melanoma em idosos no Brasil. Diagn Tratamento. 2017;22(1):3-7.
7. Pessoa DL, Ferreira LP, Silva RS, Teixeira FFN, Abreu CB, Silva EHO, et al. Análise epidemiológica do câncer de pele não melanoma no estado de Roraima no período de 2008 a 2014. Braz J Heath Rev (Curitiba). 2020;3(6):18577-90.
8. Chinem VP, Miot HA. Epidemiologia do carcinoma basocelular. An Bras Dermatol. 2011;86(2):292-305.
9. Gamonal ACC, Silva AR, Laureth A, Rêgo CM, Andrade Junior DD, Barbosa HR, et al. Câncer de pele: Prevalência e epidemiologia em um hospital de ensino da cidade de Juiz de Fora-MG. Braz J Heath Rev (Curitiba). 2020;3(6):15766-73.
10. Gutjahr GM, Almeida TS, Bastiani ES, Tejada VFS, Rodrigues O. Câncer de pele não melanoma - análise de 293 casos diagnosticados em um hospital universitário no extremo sul do Brasil. Vittalle. 2010;22(2):63-72.
11. Quintas RCS, Coutinho ALF. Fatores de risco para o comprometimento de margens cirúrgicas nas ressecções de carcinomas basocelular. Rev Bras Cir Plást. 2008;23(2):116-9.
12. Ocanha J P, Miot HA, Marques MEA, Dias JT, Stolf HO, Abbade LPF. Recidivas e recorrências de carcinomas basocelulares da face. An Bras Dermatol. 2011;86(2):386-8.
1. Hospital Municipal São José, Cirurgia Plástica, Joinville, SC, Brazil.
2. Hospital Municipal São José, Residência de Cirurgia Geral, Joinville, SC, Brazil.
3. Univille, Curso de Medicina, Joinville, SC, Brazil.
4. Dermatologia, Joinville, SC, Brazil.
GAB Final approval of the manuscript, Project Management, Writing - Review and Editing, Supervision.
CSW Final approval of the manuscript, Data Collection, Conception and design of the study, Writing -Preparation of the original, Writing - Review and Editing.
DAF Data Collection, Conception and design of the study, Writing - Preparation of the original, Writing - Review and Editing.
CMC Data Collection, Conception and design of the study, Writing - Preparation of the original, Writing - Review and Editing.
HF Data Collection, Writing - Preparation of the original, Writing - Review and Editing.
RP Final Manuscript Approval, Project Management, Writing - Review and Editing, Supervision
Corresponding author: Guilherme Augusto Bachtold R. Vinte e Cinco de Julho, 43 - América, Joinville, SC, Brazil Zip Code: 89204-080 E-mail: guilhermebachtold@yahoo.com.br
Article received: August 09, 2021.
Article accepted: December 13, 2021.
Conflicts of interest: none.
Institution: Hospital Municipal São José, Joinville, SC, Brazil.











 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter