

Original Article - Year 2022 - Volume 37 -
The mastopexy technique without preoperative markings idealized by Dr. Millan: description of the technique and patient satisfaction evaluation
Técnica de mastopexia sem demarcação prévia idealizada pelo Dr. Millan: descrição da técnica e avaliação do nível de satisfação
ABSTRACT
Introduction: Different surgical techniques were developed to reduce glandular volume and correct breast ptosis, with the objective of efficient and quality results for the patients and with the fewest possible complications. This study describes the treatment technique standardized by Dr. Roberto Millan and the level of women's satisfaction after performing the procedure.
Methods: This is a cross-sectional, observational and analytical study carried out from the analysis of the breast treatment technique standardized by Dr. Millan performed at the Plastic Surgery Sector of Centro Universitário Saúde ABC. The study included 20 women with grade II and III breast ptosis, according to Regnault's classification, or breast hypertrophy, defined by the criteria of Sacchini et al. and by Franco & Rebello; and 20 women previously submitted to mastopexy or reduction mammoplasty using the Millan technique, aged between 18 and 60 years. The BREAST-Q® questionnaire was applied to analyze the level of satisfaction after the procedure.
Results: It is observed that there were no significant differences between women who underwent the surgery Mass group (post-surgical group) when compared to those who did not undergo surgery (control group) concerning age (p=357), (p=0.695), degree of hypertrophy (p=0.799) and degree of breast ptosis (p=0.391). Regarding breast satisfaction, psychosocial, sexual, and physical variables all presented higher values in women with surgery than those without surgery (p<0.009).
Conclusion: The breast treatment technique standardized by Dr. Millan presents results that led to patient satisfaction.
Keywords: Mammoplasty; Reconstructive surgical procedures; Patient satisfaction; Breast; Surveys and questionnaires.
RESUMO
Introdução: Diferentes técnicas cirúrgicas foram desenvolvidas para a redução do volume glandular e para a correção da ptose mamária com o objetivo de obter resultados eficientes e de qualidade com o menor número de complicações possível. Este artigo descreve a técnica de mastopexia idealizada pelo Dr. Roberto Antonio Barjaz Millan e a avaliação do nível de satisfação das mulheres após o procedimento.
Métodos: Trata-se de um estudo transversal, observacional e analítico desenvolvido a partir da análise da técnica de mastopexia na redução mamária e na correção de ptose mamária padronizada pelo Dr. Millan, realizado no Setor de Cirurgia Plástica do Centro Universitário Saúde ABC. Participaram do estudo 20 mulheres com ptose mamária grau II e III, segundo classificação de Regnault, ou hipertrofia mamária, definida pelos critérios de Sacchini et al. e de Franco & Rebello, ainda não submetidas a cirurgia e 20 mulheres previamente submetidas a mastopexia pela técnica de Millan, com idades entre 18 e 60 anos. Para análise do nível de satisfação após o procedimento, foi aplicado o questionário BREAST-Q®.
Resultados: Não houve diferenças significantes das mulheres que fizeram a cirurgia (grupo pós-cirúrgico) quando comparadas às que não fizeram cirurgia (grupo controle) em relação às variáveis idade (p=0,357), Índice de Massa Corporal (p=0,695), grau de hipertrofia (p=0,799) e grau de ptose mamária (p=0,391). Em relação às variáveis de satisfação com mamas, psicossocial, sexual, físico, todas as pacientes submetidas a cirurgia apresentaram valores maiores comparados aos valores obtidos nas pacientes do grupo sem cirurgia (p<0,009).
Conclusão: A técnica de mastopexia idealizada pelo Dr. Millan apresenta resultados que foram considerados satisfatórios pelas pacientes avaliadas.
Palavras-chave: Mamoplastia; Procedimentos cirúrgicos reconstrutivos; Satisfação do paciente; Mama; Inquéritos e questionários
INTRODUCTION
The rates of breast volume reduction surgery or ptosis correction have increased in Brazil. In 2019, 202,029 surgeries were performed, representing 13.38% of aesthetic plastic surgeries. Several surgical techniques have been developed to correct these breast deformities. The objective is always to achieve increasingly efficient results and offer a better quality of life for patients with fewer complications. The resulting scars have been the object of special attention, especially their extent and location.
All breast surgery that requires a change in the spatial situation of the nipple-areolar plate involves tissue remodeling and skin incisions, which defines the term mastopexy. Mastopexy is indicated in breast hypertrophy and the correction of breast ptosis. The history of mastopexy is full of very different techniques. From the description by Wise in 1956, who introduced the previous demarcation and the ending in an inverted T, this has been a constant in this type of procedure1. With the description by Pitanguy, 1960, the use of pedicles spread with different variations2.
However, there is a technique that does not use the previous demarcation, nor is it based on pre-established pedicles, widely used in our country, devised by Dr. Roberto Antônio Barjas Millan, a physician of extraordinary importance in the history of the development of plastic surgery in Brazil and, in particular, in São Paulo, being co-founder of the Regional of the Sociedade Brasileira de Cirurgia Plástica in 1966 and responsible for the formation of care and teaching services in this specialty.
Dr. Millan, as he is known in our specialty, has admittedly developed and improved several surgical techniques. However, for reasons of an intimate nature, he never set out to transform them into scientific documents, being enough for him to teach and, above all, to obtain a result, the best possible, to the wishes of the patients.
The mastopexy technique he developed differs essentially from the others in that it is not pre-marked and allows for a change in the shape of the breasts until almost the end of the surgery, when the necessary tissue resection takes place, especially skin flaps3.
OBJECTIVE
This research aims to describe the treatment technique standardized by Dr. Millan without prior marking and assess the level of patient satisfaction after the procedure.
METHODS
This is a primary, cross-sectional, comparative, observational, analytical study developed at Faculdade de Medicina do ABC, in Santo André-SP, between May 1 and October 1, 2019. The determinations of Resolution 466/12 of the National Health Council, which provides guidelines and standards that regulate research involving human beings, were followed to conduct this project.
The project was analyzed and approved by the Ethics and Research Committee of Faculdade de Medicina do ABC under protocol CAAE 09088918.8.0000.0082, Opinion number: 3,315,883.
Forty consecutive female patients were selected, 20 of whom were about to undergo surgery (Control Group) and 20 already operated using the Millan technique (Operated Group) for at least 6 months and at most 12 months. The patients had grade II and III breast ptosis according to the Regnauld4 classification, or breast hypertrophy, defined by the criteria of Sacchini5 and Franco & Rebello6. The indications were all primary surgery aged between 18 and 60 years.
All patients were clinically evaluated and were in good health, with no comorbidities. Body Mass Index (BMI) values ranged from 20 to 29.9 kg/m2. Patients with pregnancy or delivery for less than one year, those undergoing investigation or diagnosis of breast pathologies and those with other clinical comorbidities were excluded.
The same surgeon performed the surgeries.
To analyze the women’s level of satisfaction after the procedure, the Breast-Q®7 questionnaire was applied. The following four subscales were used to compare the two groups: breast satisfaction, psychosocial well-being, sexual well-being, and physical well-being. The satisfaction with the overall result (postoperative version) subscale was applied to the mammoplasty group using the Millan technique.
The answers to the items of each subscale were transformed, using the Q-Score® scoring software, into a total score that ranges from zero to 100. The higher the score, the greater the satisfaction, or the better the quality of life.
Measures of central tendency and dispersion, as well as absolute and relative frequencies, were used to describe the variables. Because of the non-normality of some of the study variables (Shapiro-Wilk test, p<0.05), it was decided to compare them with the second group (control versus postoperative) through the test of MannWhitney. The association of the group with qualitative variables was performed using the chi-square. The statistical package STATA 11.0 was used.
Technique
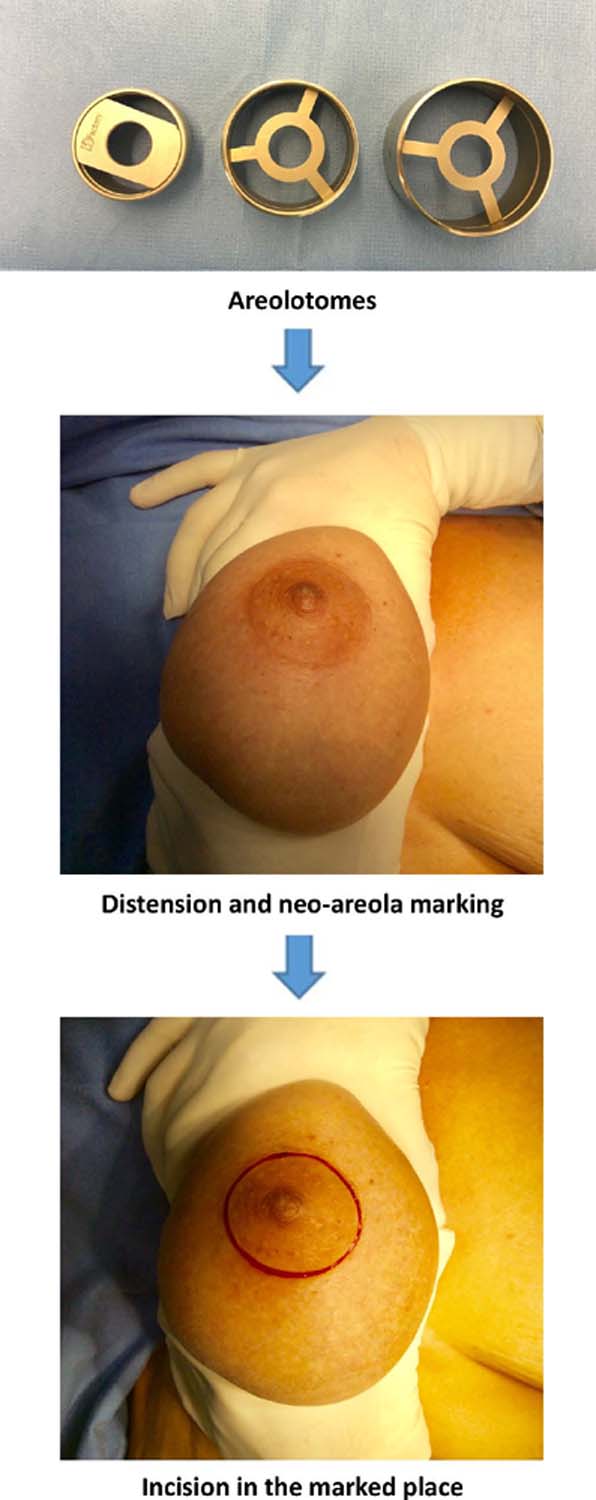
Patients were placed in dorsal decubitus, in a supine position, with the trunk maintaining an angle of 45° with the pelvis and the hands kept under the gluteal region, with the arms in a semiflexed position (Figure 1).
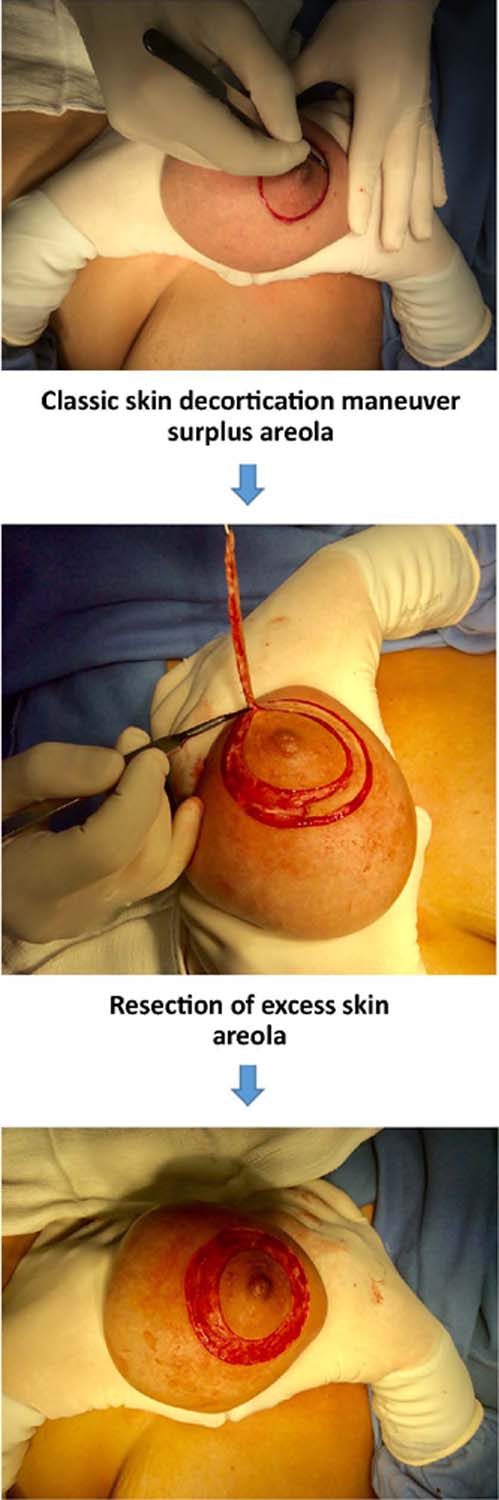
The size of the neo-areola was chosen with the aid of areolotomes that varied in three sizes (Figure 2). Next, the excess areola skin was decorticated (Figure 3).
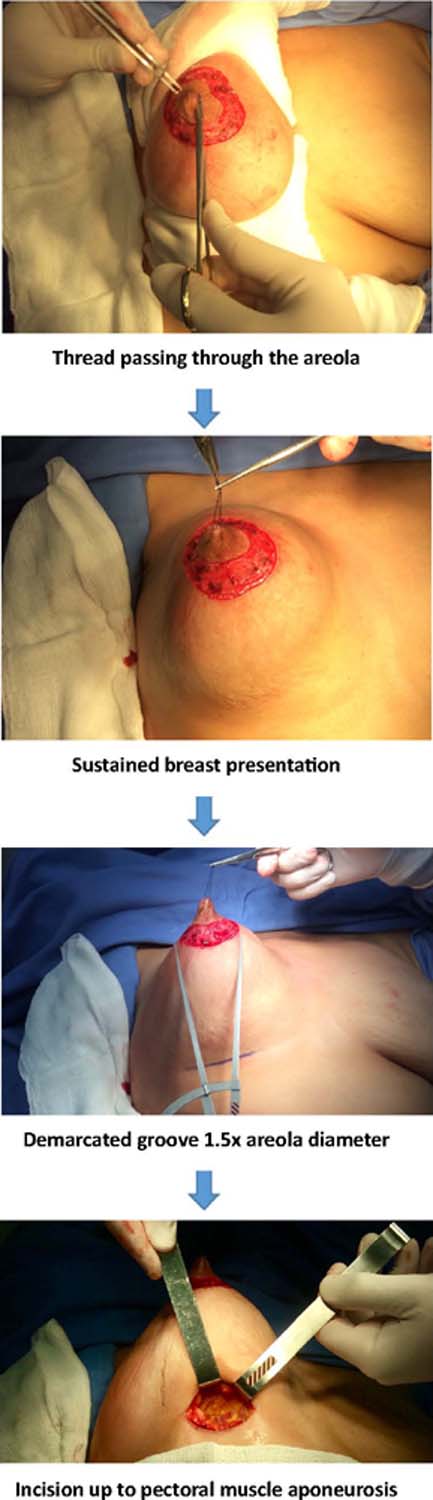
A 3-0 nylon monofilament thread was passed through the areola to keep the breast under gentle traction, and the projection of the areola was marked in the submammary groove. The length of the horizontal incision in the sulcus was 5 to 7 cm and the midpoint projected by the nipple. The incision was made, and the skin and subcutaneous tissue were sectioned until reaching the supra-aponeurotic plane of the pectoralis major muscle (Figure 4). The dissection progressed, in this plane, in a superior direction until the projection of the areola.
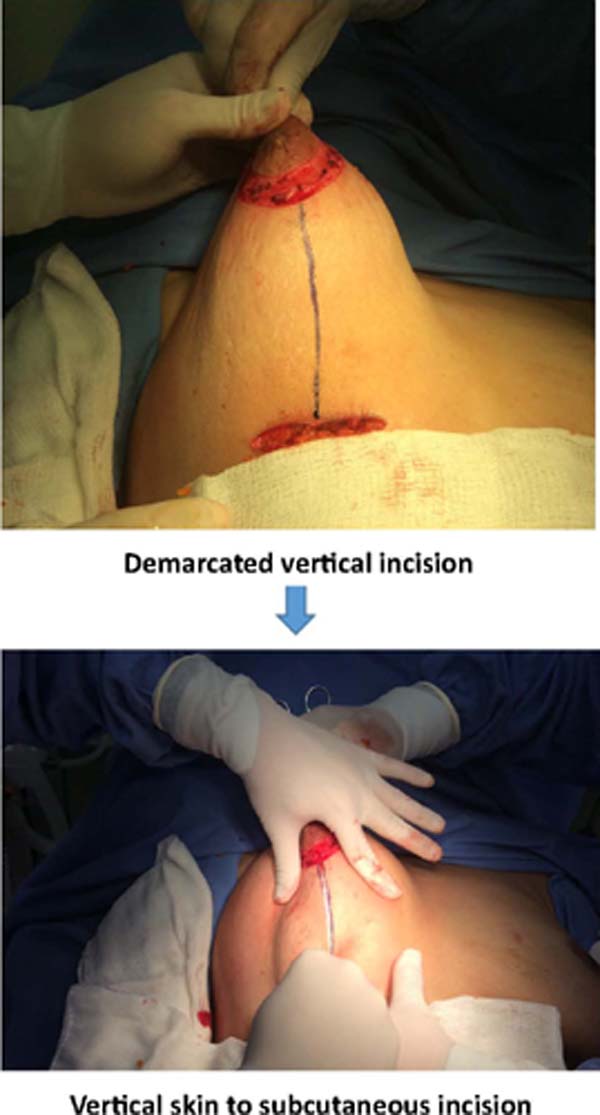
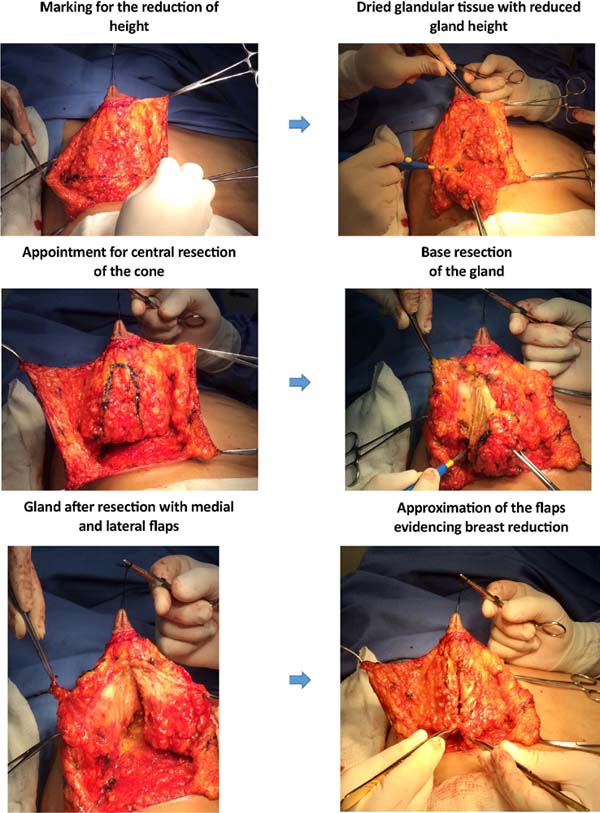
The vertical incision site was marked from the lower limit of the decorticated area of the areola to the midpoint of the incision in the submammary groove, reaching the mammary gland tissue (Figure 5). From this depth, two flaps, medial and lateral, skin and subcutaneous, were dissected with sufficient thickness to maintain vitality, which provided ample exposure to the mammary gland. The dissection did not exceed the median limit of the breast (Figure 6).
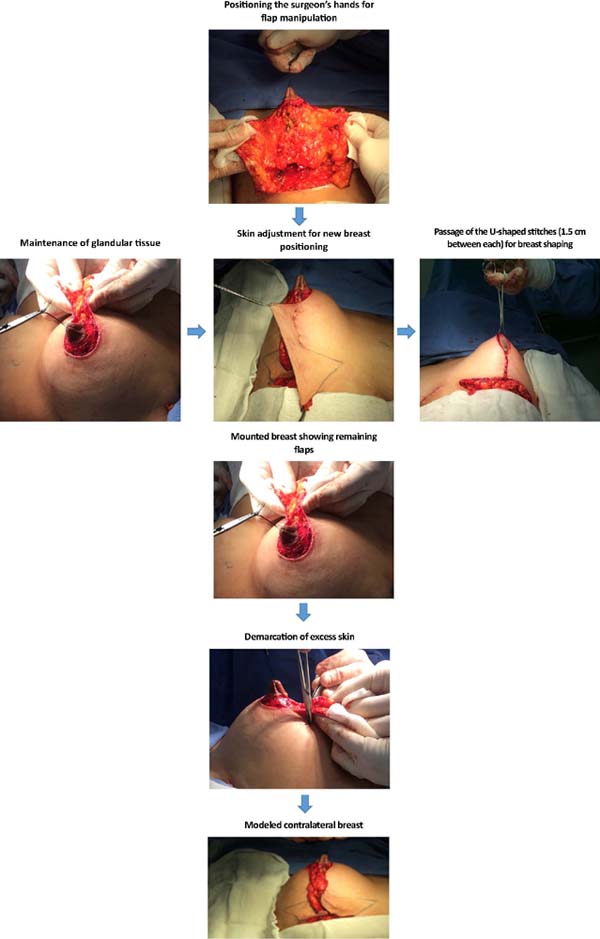
After demarcation, the glandular tissue segment corresponding to the reduction in breast height was resected. Next, the area of central tissue considered to be excess of the gland was demarcated and removed. After this resection, two flaps, medial and lateral, of glandular tissue resulted. The actual reduction was evaluated when approaching the flaps mentioned above (Figure 7). The medial and lateral flaps were brought together with a 2-0 nylon monofilament thread to contain the glandular tissue. The breast was positioned in a new situation and adjusted to the skin tension by bidigital manipulation. This position was maintained, and the skin and subcutaneous flaps were transfixed by five U-shaped stitches, with a distance of approximately 1.5 cm between them. The new position of the breast in the thorax concerning the contralateral one not yet operated on was observed.
The same demarcation and resection procedures were used in the contralateral gland. After modeling the flaps of the other breast, the symmetry was adjusted (Figure 8).
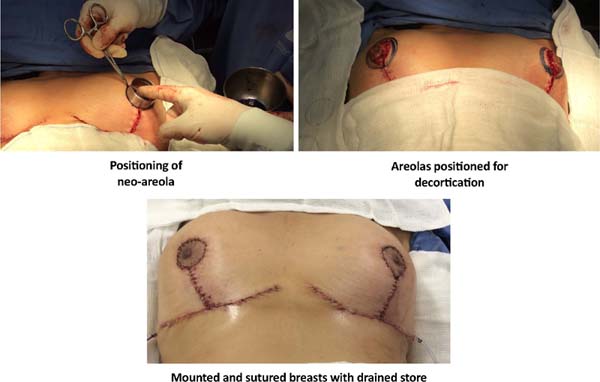
Excess skin and subcutaneous tissue were demarcated and resected with a #22 scalpel blade. Tubular suction drains with a diameter of 4.8 mm were placed, with internal access at the level of the horizontal incision, exteriorization in the anterior axillary line bordering the chest, and fixed with 3-0 cotton threads transfixed into the skin and then tied to the tube. The horizontal and vertical incision was approximated in planes with absorbable synthetic monofilament thread. The subcutaneous tissue is approximated by simple stitches separated with 4-0 thread. The skin was initially sutured with juxtadermal stitches, inverted knots, with 4-0 thread, and, finally, the skin was sutured with an intradermal stitch with 4-0 absorbable monofilament thread.
To make the neo-areola, the same molds used at the beginning of the operation were positioned symmetrically at the apex of the breasts. After demarcation, this area was resected, and the areola was exteriorized. For the approximation of the edges, they were distributed with four cardinal points, kept for presentation. A juxtadermal approximation was performed, with 5-0 stitches inverted, followed by a classic Allgower suture (Figure 9).
The sutured incisions were covered with cut gauze and fixed with Micropore® tape. Then, the area was covered with layers of hydrophilic cotton, bandaging and placement of the drains.
The patients returned in the first and second postoperative periods with the removal of the drain in the second postoperative period, oriented regarding the dressing, and the returns were performed at one week, 15 days, 30 days, 3 months, 6 months and 1 year.
RESULTS
Satisfaction level
It is observed that there were no significant differences between the women who underwent surgery (post-surgical group) when compared to those who did not undergo surgery (control group) concerning the variables age (p=0.357), BMI (p=0.695), degree of hypertrophy (p=0.799) and degree of breast ptosis (p=0.391). Regarding the variables of satisfaction with the breasts, psychosocial, sexual and physical all showed higher values in women with surgery than in the group without surgery (p<0.009) (Table 1).
| Variables | Control group | Post-Surgical Group | p |
|---|---|---|---|
| Mean (SD) | |||
| Median (P25-P75) | |||
| Age (years) |
33.5 (10.7) 33.5 (23.5 - 40.5) |
36.4 (10.5) 37.0 (26.0 - 45.0) |
0.357 |
| BMI (Kg/m2) |
26.4 (2.4) 26.6 (24.2 - 28.5) |
26.2 (1.7) 26.0 (25.1 - 27.7) |
0.695 |
| Satisfaction with the breasts |
25.6 (12.6) 27.5 (18.0 - 36.0) |
83.7 (14.9) 84.5 (71.0 - 100.0) |
<0.001 |
| Psychosocial well-being |
30.4 (17.7) 29.0 (18.5 - 43.0) |
89.7 (11.5) 89.5 (78.5 - 100.0) |
<0.001 |
| Sexual well-being |
31.8 (15.6) 30.5 (23.5 - 39.0) |
86.9 (15.0) 91.0 (73.0 - 100.0) |
<0.001 |
| Physical well-being |
63.5 (18.7) 70.0 (49.0 - 79.0) |
79.9 (10.0) 78.0 (72.5 - 89.5) |
0.009 |
| Degree of Hypertrophy (n=27) | n (%) | ||
| 1 | 3 (23.1) | 2 (14.3) | 0.799 |
| 2 | 6 (46.2) | 8 (57.1) | |
| 3 | 4 (30.8) | 4 (28.6) | |
| Degree of Breast Ptosis (n=13) | |||
| 2 | 4 (57.1) | 2 (33.3) | 0.391 |
| 3 | 3 (42.9) | 4 (66.7) | |
DISCUSSION
Although mastopexy is a highly satisfactory surgery, complications and unfavorable results can occur, such as wound dehiscence, hypertrophic scars, infections, fatty necrosis, hematomas and partial or total necrosis of the nipple-areolar complex, in addition to asymmetries and position abnormalities8. The multiplicity of techniques described reveals the intense search for the best technique to reduce complications and improve women’s quality of life. In addition, it has to be easier to be instructed in learning services such as medical residency and passed on to new generations of already trained professionals.
For these reasons, the great advantage of the technique developed by Dr. Millan is to be able to evaluate the result of the assembly of the breast cone even before the skin resection, which allows adaptations, especially in cases of breast asymmetry avoiding unfavorable outcomes.
The detachment of the lateral and medial skin flaps is always the minimum necessary, and the horizontal scar is always the smallest possible, which makes it very appropriate for those patients in which the risk of circulatory compromise is expected, such as patients who are smokers, elderly or with controlled chronic pathologies, or also that they can be carriers of damage to the microcirculation, such as diabetes, hypertension and inflammatory diseases involving collagen.
In cases where the distribution of breast parenchyma and adipose tissue is very heterogeneous, this technique offers the visibility and freedom to promote changes in the shape and size of both breasts until the final moments of the surgery, ensuring the best possible symmetry.
The positioning of the lateral and medial skin flaps, leading to the compensation of the skin resection towards the apex of the mammary cone, generates a greater resection of the periareolar skin, which reduces the compensation in the access route in the inframammary fold, reducing its length. As the skin resection is performed based on the definitive coneshaped assembly of the breast tissues, there is no resulting tension, which avoids the flattening of the breast shape as reported in periareolar techniques9, 10, 11.
The techniques that follow demarcations and the making of pedicles can serve as a guide and are based on previous personal experiences. However, there are situations in which predictability is difficult, such as accentuated asymmetries or when the skin conditions of the breasts are uneven, as in the presence of numerous stretch marks or scars from previous burns, factors that change the malleability of the tissues unpredictably. In these cases, a technique that allows adaptations during the surgical procedure can be much more efficient and safer.
However, it is worth considering that in breast surgeries that involve large reductions, in which the horizontal scar in the groove will be extensive, techniques with prior marking optimize the surgical time since they are faster and the difference in scar size may not be significant.
The technique is ideal for ptosis, asymmetries and augmentation mammaplasties associated with the resection of a large excess of skin because it takes into account, in addition to the quality of the skin, also the consistency of the breast tissue. This is different from previous demarcation techniques that often follow inflexible patterns that may not be suitable for all cases and, in particular, may not accurately calculate the amount of skin that will be resected.
Body image represents a person’s physical appearance, resulting from a combination of perceptualneural processes, environmental, social and psychological factors and can manifest through the degree of care and satisfaction with the body12. Thus, concerning women’s level of satisfaction with the procedure performed, the results showed that mastopexy standardized by Millan’s technique brought a significant improvement in satisfaction with the breasts: in psychosocial well-being, sexual well-being and physical well-being. These results converge with similar studies that evaluated the level of satisfaction with another mastopexy techniques13,14.
When comparing the results of the Breast-Q® questionnaire from the Operated Group to those from the Control Group, it becomes more evident that the request for breast correction goes beyond the physical aspects. Women who perform such procedures are looking to improve their quality of life, which may represent an ingroove in self-esteem, an improvement in appearance and social acceptance, and an improvement in the context of sexual relationships.
CONCLUSION
The mastopexy technique standardized by Dr. Roberto Antônio Barjas Millan has a high level of satisfaction and seems to fulfill patients’ expectations once confronted with the evaluations of women who have not yet undergone surgery. It is a technique that does not use the previous demarcation and provides greater flexibility in surgical times, allowing adjustments until the final moments of the surgery, which can favor the result, especially in asymmetrical breasts and with large excesses of skin.
REFERENCES
1. Wise RJ. A preliminary report of a method of planning the mammaplasty. Plast Reconstr Surg (1946). 1956;17(5):367-75.
2. Pitanguy I. Surgical treatment of breast hypertrophy. Br J Plast Surg. 1967;20(1):78-85.
3. Pereira Filho G V, Nunes JMC, Costa RL. Mamoplastia redutora na Faculdade de Medicina do ABC - 25 anos de evolução. Arq Méd ABC. 1999;22(1/2):21-32.
4. Regnault P. Breast ptosis. Definition and treatment. Clin Plast Surg. 1976;3(2):193-203.
5. Sacchini V, Luini A, Tana S, Lozza L, Galimberti V, Merson M, et al. Quantitative and qualitative cosmetic evaluation after conservative treatment for breast cancer. Eur J Cancer. 1991;27(11):1395-400.
6. Franco T, Rebello C. Mamaplastias. In: Franco T, Rebello C, eds. Cirurgia Estética. Rio de Janeiro: Atheneu; 1977. p. 203-71.
7. Pusic AL, Klassen A F, Scott AM, Klok JA, Cordeiro PG, Cano SJ. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg. 2009;124(2):345-53.
8. Pinsolle V, Tierny C, Héron A, Reynaud P, Pélissier P. Résultats défavorables des plasties mammaires de réduction. Causes, préventions et traitements. Ann Chir Plast Esthet. 2019;64(5/6):575-82.
9. Benelli LA. A new periareolar mammaplasty: the “round block” technique. Aesthetic Plast Surg. 1990;14(2):93-100.
10. Góes JC. Periareolar mammaplasty: double skin technique with application of polyglactine or mixed mesh. Plast Reconstr Surg. 1996;97(5):959-68.
11. Bozola AR. Periareolar breast reduction. Aesthetic Plast Surg. 2009;33(2):228-34.
12. Sarwer DB, Polonsky HM. Body Image and Body Contouring Procedures. Aesthet Surg J. 2016;36(9):1039-47.
13. Pitanguy I. Mamaplastias: estudo de 245 casos consecutivos e apresentação de técnica pessoal. Rev Bras Cir. 1961;42(4):201-20.
14. Santos GR, De-Araújo DC, Vasconcelos C, Chagas RA, Lopes GG, Setton L, et al. Impacto da mamoplastia estética na autoestima de mulheres de uma capital nordestina. Rev Bras Cir Plást. 2019;34(1):58-64.
1. Centro Universitário Saúde ABC, Faculdade de Medicina do ABC, Santo André, S P,
Brazil.
2. Hospital Israelita Albert Einstein, São Paulo, SP, Brazil.
PEE Analysis and/or interpretation of data, Statistical analysis, Conception and design of the study, Resource Management, Project Management, Investigation, Methodology, Conducting operations and/or experiments, Writing - Preparation of the original, Writing - Review and Editing.
LCA Final Manuscript Approval, Supervision, Preview.
BJMO Statistical analysis, Study conception and design, Resource Management, Writing - Review and Editing, Visualization.
Corresponding author: Pablo Eduardo Elias Rua Elvira Ferraz 250, CJ 309, Vila Olímpia, São Paulo, S P, Brazil Zip Code: 04552-040 E-mail: contato@drpabloelias.com.br
Article received: February 25, 2021.
Article accepted: December 13, 2021.
Conflicts of interest: none.
Institution: Centro Universitário Saúde ABC, Faculdade de Medicina do ABC, Departamento de Cirurgia Plástica, Santo André, S P, Brazil.















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter