

Original Article - Year 2022 - Volume 37 - Issue 3
Innovation in liposuction cannula to harvest fat graft to use in breast reconstruction
Inovação em cânula de lipoaspiração para coleta de enxerto de gordura para uso em reconstrução mamária
ABSTRACT
Introduction: The evolution of liposuction and fat graft technique with the oncologic safety allowed to use the fat as autologous filler in patients with breast cancer and submitted to breast reconstruction. The objective is to to introduce an innovation in the instrument used to harvest fat grafts for breast reconstruction.
Methods: Search of anteriority and trademarks were performed at international and national databases, and a prototype was built as a fat harvest instrument with 35cm in length, 4cm in diameter, with 10 holes at the distal extremity, with 2mm diameter each. It was experimented with a harvest of a viscous substance, comparing the prototype with two regular industry cannulas types: three holes Mercedes' type and five roles Pitanguy's type.
Results: Four high-relevance patents and one medium-relevance patent were found, which differ from the proposed utility model when comparing the type of design of the distal end of the studied cannulas and the function of the instruments identified. When the prototype's efficiency was compared with the other cannulas, the cannula with five holes in Pitanguy's type was the most efficient, and it was no statistical difference between the prototype and the cannula with three roles in Mercedes' type.
Conclusion: The innovation presented to harvest fat graft for breast reconstruction had the same efficiency in harvesting the viscose substance as the cannula Mercedes type with three holes in this experimental model.
Keywords: Subcutaneous fat; Breast; Breast neoplasms; Cannula; Graft survival; Adipocytes.
RESUMO
Introdução: A evolução da técnica de lipoaspiração e da enxertia de gordura associada a segurança oncológica permitiram utilizar a gordura como preenchedor autólogo em pacientes com neoplasia de mama que eram submetidas a reconstrução mamária. O objetivo é apresentar uma inovação no instrumento de coleta de gordura que será utilizada como enxerto, para uso em reconstrução mamária.
Métodos: Foi realizada a busca de anterioridade nos bancos de dados internacionais e nacional e a confecção de um protótipo de cânula de coleta de gordura de 35cm de comprimento, com diâmetro do tubo de 4mm, com 10 furos redondos na sua extremidade distal com 2mm de diâmetro. Foi realizado um experimento de aspiração de substância viscosa comparando o protótipo com dois modelos de cânulas com desenho padrão da indústria, de três furos tipo Mercedes e de cinco furos tipo Pitanguy.
Resultados: Foram encontrados quatro patentes de alta relevância e uma patente de média relevância, que diferem do modelo de utilidade proposto quando se comparam o tipo de desenho da extremidade distal das cânulas estudadas e a função dos instrumentos identificados. Quando comparou-se a eficiência do protótipo, a cânula de cinco furos foi a mais eficiente na aspiração da substância viscosa, e não houve diferença estatística na velocidade de aspiração entre o protótipo e a cânula de três furos tipo Mercedes.
Conclusão: A inovação apresentada para a coleta de enxerto de gordura para uso em reconstrução mamária apresentou a mesma eficiência que a cânula Mercedes de três furos neste modelo experimental.
Palavras-chave: Gordura subcutânea; Mama; Neoplasias da mama; Cânula; Sobrevivência de enxerto; Adipócitos
INTRODUCTION
The use of fat as an autologous filler in breast reconstruction began in 1895 with Czerny, who used a patient’s lipoma to reconstruct the breast1. Its use has fallen into disuse due to morbidity in the donor area when large tissue volumes are used. However, with the description of the fat extraction technique with cannulas, called liposuction, plastic surgeons were offered an important tool for fat collection as an autologous filler with low morbidity2.
However, due to the technical limitations of the time, a high number of complications such as graft loss and steatonecrosis that led to breast calcifications, and the available diagnostic imaging technology resources that were unable to differentiate between steatonecrosis calcifications and breast microcalcifications, the new procedures by the American Society of Plastic Surgery in 1987 contraindicated breast fat grafting due to the possibility that steatonecrosis calcifications could compromise the diagnosis of early breast neoplasms on mammography.
From 2005 onwards, with the evolution of the liposuction and fat grafting technique, associated with the technological evolution of diagnostic imaging methods, new studies showed the evolution of the technique of fat grafting in the breasts, with a lower incidence of complications locally3,4,5,6.
In 2011, the first studies were published showing the oncological safety of fat grafting in patients with breast cancer and undergoing breast reconstruction, increasing its use in patients with breast cancer7,8,9,10,11,12,13.
Despite the ease of collecting fat grafts, the main obstacle to its use is the high absorption rate, which varies from 20 to 90%14,15,16,17. In order to improve fat graft integration rates, with a smaller number of surgical interventions in patients, innovations in each step of the fat tissue preparation method were proposed18.
The most important characteristics for the success of fat grafting are patient age, choice of the donor area, the technique of fat collection, the instrument for fat collection, fat processing, the injection technique and the preparation of the recipient area.19,20
The use of liposuction cannulas with a larger diameter alone has higher collection rates of viable adipocytes in experimental models14,21.
In addition to the diameter of the cannula tube, the size and number of holes are important for the collection22. 2-mm-diameter cannulas with four 600-μm holes and multi-perforated cannulas with 1-mm holes were proposed for micrografts on the face23.
Apart from the 3mm diameter Coleman™ fat graft collection cannula with two holes, which is not designed for breast fat grafting, there are few proposals for innovation in the fat collection instrument to reduce trauma in adipocytes and improve the rates of viability and integration of fat grafts when it is desired to collect larger volumes of fat graft for use other than the face24,25.
OBJECTIVE
To present an innovation for liposuction cannula to collect fat micrografts for use in patients undergoing mastectomy who wish to reconstruct their breasts and optimize their final aesthetic result.
METHODS
This is a primary, experimental, prospective, comparative and controlled study, carried out from March 2016 to March 2017 at the Universidade Federal do Estado de São Paulo (UNIFESP), presented to the Ethics and Research Committee of UNIFESP, having received the number 6331150116. A search for prior patents was carried out in international databases: Espacenet, The United States Patent and Trademark Office (USPTO), World Intellectual Property Organization (WIPO), China National Intellectual Property (CNIPA) and Japan Patent Office (JPO), the National Institute of Intellectual Property (INPI) database, the PatBase software and Google Patents, with the keywords and classifications: cannula, liposuction, orifice, neoplasia, A61B, A61M.
For the experimental study, a prototype of a surgical steel cannula for the fat collection was developed and made with 10 holes at the distal end of 2 mm in diameter each, in a hollow tube with a luminal diameter of 4 mm and 35 cm in length, with a coupler at its proximal end for a 60ml syringe with a catheter tip and for an adapter for a suction device for storing the fat to be used, to collect fat grafts in blocks of fat tissue up to 2mm in diameter (micrografts) (Figure 1).
The experiment was carried out by comparing the aspiration efficiency of the prototype with two models of liposuction cannula with a luminal diameter of 4 mm and a length of 35 cm, with an industry-standard design and of the same brand (three holes with a Mercedes-type design, and five holes with a design type PitanguyTM) all made by the same company (Richter®, São Paulo, Brazil), considering the same material and the same resistance of the tubes (Figure 2).
A pilot was carried out with a model of water aspiration under continuous pressure of 30mmHg, 20mmHg, 10mmHg, and the aspirated weight of four measurements of the three cannulas at 30”, 60” and 90” were compared. The Aspirotec III surgical aspirator (Sismatec company, Curitiba, Brazil) was used, with a digital scale model EHA251 of 0.1gr accuracy and 500gr capacity (Camry electronic, Guangdong, China). As there was no statistical difference in the volume of water aspirated between the different pressures in the different types of the cannula, the aspiration pressure was defined at 10 mmHg in 10 measurements of the three cannulas in 30”, 60” and 90”.
The experiment of aspiration of viscous substance (soybean oil, density 0.891gr/cm3) under continuous pressure of 10mmHg was then performed, and the aspirated weight of 10 measurements of the three cannulas at 30”, 60” and 90” was compared. The Aspirotec III surgical aspirator (Sismatec company, Curitiba, Brazil) was used with a digital scale model EHA251 with 0.1gr accuracy and 500gr capacity (Camry electronic, Guangdong, China)26.
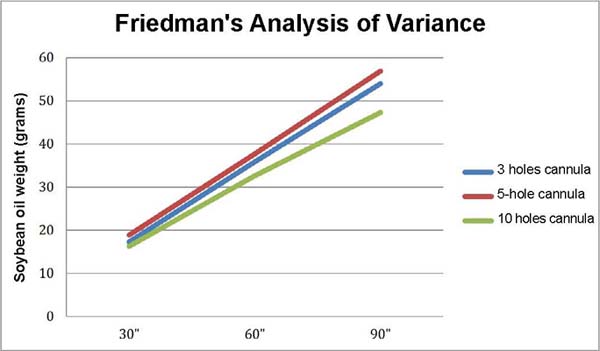
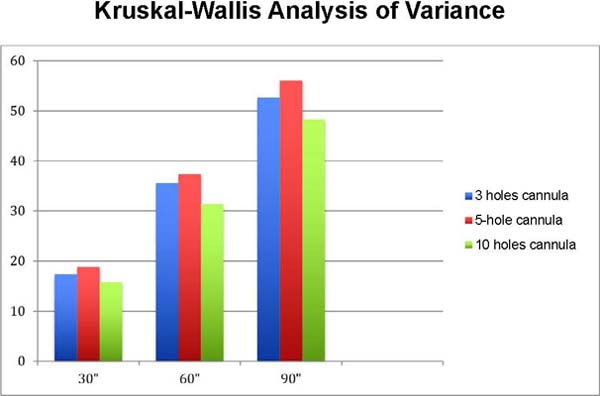
To analyze the results, Friedman’s analysis of variance was applied to each of the cannula designs, studying the aspiration speed of grams of soybean oil/ second at times 30”, 60”, and 90”; and the Kruskal-Wallis analysis of variance to compare the three types of cannula designs, at 30”, 60”, and 90” times separately27.
In all tests, the significance level was set at 0.05 or 5%.
RESULTS
Four highly relevant patents were found (product catalog of the company Tulip Medical - “Sorensen Harvested’ and “Sforza Harvester” cannula; WO 2014074606 (A1) - adjustable liposuction cannula; US 8333740 B2 - tissue transfer cannula; and US 2008/0167613 - closed system and method for atraumatic, low pressure, continuous harvesting, processing, and grafting of lipoaspirate) and a patent of medium relevance (US 5817050 A - liposuction cannula), which differ from the proposed utility model when comparing the type of design of the distal end of the studied cannulas and the function of the instruments identified.
The weight in grams of soybean oil aspirated per second was higher in the five-hole cannula group (Table 1), followed by the three-hole cannula group, and the 10-hole cannula group at times 30”, 60” and 90” when performing Friedman’s analysis of variance (30” x 60” x 90”) (Figure 3).
| Cannula 3 holes | Cannula 5 holes | Cannula 10 holes | ||||||
|---|---|---|---|---|---|---|---|---|
| 30” | 60” | 90” | 30” | 60” | 90” | 30” | 60” | 90” |
| 17.2 | 52.5 | 70.1 | 20 | 39.5 | 62.3 | 15.9 | 31.4 | 47 |
| 17.9 | 36.1 | 54.9 | 18 | 37.5 | 58.8 | 16.1 | 31.9 | 47.5 |
| 19.4 | 37.6 | 57 | 17.3 | 36.4 | 55.7 | 16.1 | 31.7 | 47.7 |
| 19.1 | 37.6 | 56.5 | 19 | 37 | 55.6 | 16 | 31.9 | 47.4 |
| 17.4 | 34.4 | 51.1 | 18.6 | 37.1 | 55.4 | 15.7 | 31.4 | 48.3 |
| 17.4 | 32.9 | 50 | 18.8 | 38 | 55 | 15.7 | 31.4 | 47.2 |
| 16.7 | 32.9 | 49.3 | 19 | 37 | 54.6 | 15.7 | 31.3 | 46.9 |
| 18.5 | 35.9 | 53.9 | 20 | 39 | 57.4 | 15.4 | 30.6 | 46.6 |
| 17.3 | 35.3 | 51.4 | 18.8 | 37.4 | 56.5 | 15.4 | 31.5 | 47.1 |
| 12.1 | 23.4 | 45.9 | 19.1 | 37.7 | 57.5 | 21.4 | 42.9 | 57.4 |
| Average 17.3 | 35.9 | 54.0 | 18.9 | 37.7 | 56.9 | 16.3 | 32.6 | 48.3 |
| Median 17.4 | 35.6 | 52.7 | 18.9 | 37.4 | 56.1 | 15.8 | 31.4 | 47.3 |
| Friedman’s analysis of variance (30”x60”x90”) | ||||||||
| Cannula 3 holes | Cannula 5 holes | Cannula 10 holes | ||||||
| X2r= 20.00 | X2r= 20.00 | X2r= 20.00 | ||||||
| (p<0.0001) | (p<0.0001) | (p<0.0001) | ||||||
| 90”>30” | 90”>30” | 90”>30” | ||||||
| Kruskal-Wallis analysis of variance (30”x60”x90”) | ||||||||
| 30” | 60” | 90” | ||||||
| H= 12.69 | H= 12.70 | H= 13.89 | ||||||
| p=0.0018 | p=0.0017 | p=0.0010 | ||||||
| Cannula de 5 holes >10 holes | Cannula de 5 holes >10 holes | Cannula de 5 holes >10 holes | ||||||
| Cannula de 5 holes > 3 holes | Cannula de 5 holes > 3 holes | Cannula de 5 holes > 3 holes | ||||||
When comparing the aspirated weight of soybean oil per second between the five-hole cannula X three-hole cannula X 10-hole cannula groups, the five-hole cannula aspirated a greater amount of soybean oil per second. However, there was no statistical difference between the weight of soybean oil aspirated per second between the three-hole cannula and 10-hole cannula groups by the Kruskal-Wallis test (Figure 4).
DISCUSSION
Breast cancer is the second most common type worldwide after non-melanoma skin cancer. It is the most common among women, accounting for 25% of new cases yearly. In men, it represents 1% of all cases of the disease. In Brazil, the estimate was 66,280 new cases for the year 2020. In 2019, the number of deaths from breast cancer was 18,285, with 227 men and 18,068 women28.
Mastectomized patients undergoing breast reconstruction have a better quality of life, self-esteem, and improved sexuality compared to non-reconstructed patients29,30.
Fat grafting alone or associated with the reconstruction technique with autologous or alloplastic tissue aims to improve reconstruction quality, especially in irradiated skin13.
In 2015, a systematic review on fat grafting was published, which concluded that although there is a difference in the survival of adipocytes according to the collection with liposuction cannulas of different types and diameters in experimental models, when performed in humans, this difference is not significant18.
In 2016, a new systematic review did not identify differences between the different types of cannula diameter for the same design in the viability of fat grafts31.
The development of new cannulas for fat graft collection is necessary to reduce the incidence of local complications such as volume reduction and the need for new surgical interventions to volumize the breasts.
The definition of the collection of more symmetrical blocks of fat up to 2.0 mm in diameter for use as a fat graft, which would be collected and stored in syringes or a larger reservoir with the use of a vacuum cleaner, in a less traumatic way and with low morbidity in the donor area, with the possibility of fewer surgical interventions in this group of patients to achieve the planned result, and that did not significantly prolong the surgical time with increased morbidity of the procedure in patients, were the main motivations that led to the elaboration of a utility model proposal for the INPI patent MU 6602563-0 U2.
It features a new design at its distal end, with 10 holes with a fixed diameter of 2.0mm, an internal diameter of the cannula of 4.0mm and a length of 35cm, with the sole objective of less traumatic and more efficient collection of fat, possibly with a greater number of viable adipocytes and an increased possibility of integration into the recipient bed, for use in breast reconstruction.
The thickness of the graft and its geometric shape are inversely proportional to the survival of the fat graft if the graft diameter exceeds 3.0 mm in diameter (radius of 1.5 + 5 mm). Therefore, the size of the chosen block of fat of up to 2.0 mm in diameter has a greater chance of being integrated into the recipient bed when this criterion is analyzed separately in the collection, defined by the type of cannula to be used32,33,34,35,36,37.
The dimension of the fat block of micrografts up to 2.0mm is determined by the diameter of the 2.0mm hole at the distal end through which the fat enters the collection cannula in a smooth and less traumatic tube and, in addition to promoting a greater possibility of survival of the adipocyte in the recipient bed and greater possibility of integration of this fat, the dimensions of the cannula (length, diameter, number and positioning of the holes) allow to collect a greater amount of fat in a shorter surgical time, and, therefore, a smaller number of surgical interventions required for volumization of the reconstructed breast with autologous fat graft. There was no difference in the speed of aspiration of soybean oil between the three-hole Mercedes cannula and the 10-hole prototype cannula.
CONCLUSION
The innovation presented with the making of a prototype with 10 holes of 2mm in diameter at its distal end was developed for the efficient collection of fat blocks up to 2mm for use in breast reconstruction and presented the same aspiration efficiency of the viscous substance oil of soybean when compared to the industry standard three-hole Mercedes design cannula design.
REFERENCES
1. Delay E, Guerid S. The Role of Fat Grafting in Breast Reconstruction. Clin Plast Surg. 2015;42(3):315-23.
2. Illouz YG. Body contouring by lipolysis: a 5-year experience with over 3000 cases. Plast Reconstr Surg. 1983;72(5):591-7.
3. Spear SL, Wilson HB, Lockwood MD. Fat injection to correct contour deformities in the reconstructed breast. Plast Reconstr Surg. 2005;116(5):1300-5.
4. Coleman SR, Saboeiro A P. Fat grafting to the breast revisited: safety and efficacy. Plast Reconstr Surg. 2007;119(3):775-85; discussion 786-7.
5. Millet E, Haik J, Ofir E, Mardor Y, Winkler E, Harats M, et al. The Impact of Autologous Fat Grafting on Breast Cancer: An Experimental Model Using Magnetic Resonance Imaging. Isr Med Assoc J. 2016;18(5):283-5.
6. Pinell-White XA, Etra J, Newell M, Tuscano D, Shin K, Losken A. Radiographic Implications of Fat Grafting to the Reconstructed Breast. Breast J. 2015;21(5):520-5.
7. Petit JY, Lohsiriwat V, Clough KB, Sarfati I, Ihrai T, Rietjens M, et al. The oncologic outcome and immediate surgical complications of lipofilling in breast cancer patients: a multicenter study--Milan-Paris-Lyon experience of 646 lipofilling procedures. Plast Reconstr Surg. 2011;128(2):341-6.
8. Largo RD, Tchang LA, Mele V, Scherberich A, Harder Y, Wettstein R, et al. Efficacy, safety and complications of autologous fat grafting to healthy breast tissue: a systematic review. J Plast Reconstr Aesthet Surg. 2014;67(4):437-48.
9. Kronowitz SJ, Mandujano CC, Liu J, Kuerer HM, Smith B, Garvey P, et al. Lipofilling of the Breast Does Not Increase the Risk of Recurrence of Breast Cancer: A Matched Controlled Study. Plast Reconstr Surg. 2016;137(2):385-93.
10. Silva-Vergara C, Fontdevila J, Descarrega J, Burdio F, Yoon TS, Grande L. Oncological outcomes of lipofilling breast reconstruction: 195 consecutive cases and literature review. J Plast Reconstr Aesthet Surg. 2016;69(4):475-81.
11. Simonacci F, Bertozzi N, Grieco M P, Grignaffini E, Raposio E. Autologous fat transplantation for breast reconstruction: A literature review. Ann Med Surg (Lond). 2016;12:94-100.
12. Petit JY, Rietjens M, Botteri E, Rotmensz N, Bertolini F, Curigliano G, et al. Evaluation of fat grafting safety in patients with intraepithelial neoplasia: a matched-cohort study. Ann Oncol. 2013;24(6):1479-84.
13. Petit JY, Maisonneuve P, Rotmensz N, Bertolini F, Clough KB, Sarfati I, et al. Safety of Lipofilling in Patients with Breast Cancer. Clin Plast Surg. 2015;42(3):339-44.
14. Erdim M, Tezel E, Numanoglu A, Sav A. The effects of the size of liposuction cannula on adipocyte survival and the optimum temperature for fat graft storage: an experimental study. J Plast Reconstr Aesthet Surg. 2009;62(9):1210-4.
15. Sommer B, Sattler G. Current concepts of fat graft survival: histology of aspirated adipose tissue and review of the literature. Dermatol Surg. 2000;26(12):1159-66.
16. Kim HY, Jung BK, Lew DH, Lee DW. Autologous Fat Graft in the Reconstructed Breast: Fat Absorption Rate and Safety based on Sonographic Identification. Arch Plast Surg. 2014;41(6):740-7.
17. Seaman SA, Tannan SC, Cao Y, Peirce SM, Lin KY. Differential Effects of Processing Time and Duration of Collagenase Digestion on Human and Murine Fat Grafts. Plast Reconstr Surg. 2015;136(2):189e-99e.
18. Strong AL, Cederna PS, Rubin J P, Coleman SR, Levi B. The Current State of Fat Grafting: A Review of Harvesting, Processing, and Injection Techniques. Plast Reconstr Surg. 2015;136(4):897-912.
19. Khouri R, Del Vecchio D. Breast reconstruction and augmentation using pre-expansion and autologous fat transplantation. Clin Plast Surg. 2009;36(2):269-80.
20. Coleman SR. Structural fat grafts: the ideal filler? Clin Plast Surg. 2001;28(1):111-9.
21. Kirkham JC, Lee JH, Medina MA 3rd, McCormack MC, Randolph MA, Austen WG Jr. The impact of liposuction cannula size on adipocyte viability. Ann Plast Surg. 2012;69(4):479-81.
22. Nguyen PS, Desouches C, Gay AM, Hautier A, Magalon G. Development of micro-injection as an innovative autologous fat graft technique: The use of adipose tissue as dermal filler. J Plast Reconstr Aesthet Surg. 2012;65(12):1692-9.
23. Alharbi Z, Opländer C, Almakadi S, Fritz A, Vogt M, Pallua N. Conventional vs. micro-fat harvesting: how fat harvesting technique affects tissue-engineering approaches using adipose tissue-derived stem/stromal cells. J Plast Reconstr Aesthet Surg. 2013;66(9):1271-8.
24. Kakagia D, Pallua N. Autologous fat grafting: in search of the optimal technique. Surg Innov. 2014;21(3):327-36.
25. Mentor - The Coleman™ Microinjection System [acesso 2021 Jul 11]. Disponível em: http://www.melon.fi/esitteet/Coleman-esite.pdf
26. Beck DO, Davis K, Rohrich RJ. Enhancing lipoaspirate efficiency by altering liposuction cannula design. Plast Reconstr Surg Glob Open. 2014;2(10):e222.
27. Siegel S, Castellan Junior NJ. Estatística não-paramétrica para ciências do comportamento. 2ª ed. Porto Alegre: Artmed; 2006. 448 p.
28. Brasil. Ministério da Saúde. Instituto Nacional do Câncer (INCA). Portal de informações sobre câncer de mama. Brasília: Ministério da Saúde; 2021 [acesso 2021 jul 11]. Disponível em: https://www.inca.gov.br/tipos-de-cancer/cancer-de-mama
29. Weichman KE, Broer PN, Thanik VD, Wilson SC, Tanna N, Levine J P, et al. Patient-Reported Satisfaction and Quality of Life following Breast Reconstruction in Thin Patients: A Comparison between Microsurgical and Prosthetic Implant Recipients. Plast Reconstr Surg. 2015;136(2):213-20.
30. Zhong T, Hu J, Bagher S, Vo A, O’Neill AC, Butler K, et al. A Comparison of Psychological Response, Body Image, Sexuality, and Quality of Life between Immediate and Delayed Autologous Tissue Breast Reconstruction: A Prospective Long-Term Outcome Study. Plast Reconstr Surg. 2016;138(4):772-80.
31. Sinno S, Wilson S, Brownstone N, Levine SM. Current Thoughts on Fat Grafting: Using the Evidence to Determine Fact or Fiction. Plast Reconstr Surg. 2016;137(3):818-24.
32. Carpaneda CA. Study of aspirated adipose tissue. Aesthetic Plast Surg. 1996;20(5):399-402.
33. Carpaneda CA, Ribeiro MT. Study of the histologic alterations and viability of the adipose graft in humans. Aesthetic Plast Surg. 1993;17(1):43-7.
34. Eto H, Kato H, Suga H, Aoi N, Doi K, Kuno S, et al. The fate of adipocytes after nonvascularized fat grafting: evidence of early death and replacement of adipocytes. Plast Reconstr Surg. 2012;129(5):1081-92.
35. Kato H, Mineda K, Eto H, Doi K, Kuno S, Kinoshita K, et al. Degeneration, regeneration, and cicatrization after fat grafting: dynamic total tissue remodeling during the first 3 months. Plast Reconstr Surg. 2014;133(3):303e-13e.
36. Vazquez OA, Markowitz MI, Becker H. Fat Graft Size: Relationship Between Cannula and Needle Diameters. Cureus. 2020;12(4):e7598.
37. James IB, Bourne DA, DiBernardo G, Wang SS, Gusenoff JA, Marra K, et al. The Architecture of Fat Grafting II: Impact of Cannula Diameter. Plast Reconstr Surg. 2018;142(5):1219-25.
1. Universidade Federal de São Paulo, São Paulo, SP, Brazil.
2. Hospital do Servidor Público Estadual de São Paulo, Instituto de Assistência Médica
ao Servidor Público Estadual, São Paulo, SP, Brazil.
MSLO Analysis and/or interpretation of data, Statistical analysis, Acquisition of funding, Data collection, Conceptualization, Conception and design of the study, Resource Management, Project Management, Investigation, Methodology, Conducting operations and/or experiments, Writing - Preparation of the original, Writing -Proofing and Editing.
EBG Final Manuscript Approval, Project Management, Methodology, Supervision.
Corresponding author: Maurício da Silva Lorena de Oliveira Rua Botucatu, 740, 2º andar, São Paulo, SP, Brazil Zip Code: 04023-061 E-mail: drmauriciolorena@gmail.com
Article received: July 11, 2021.
Article accepted: April 07, 2022.
Conflicts of interest: none.
Institution: Universidade Federal de São Paulo, São Paulo, SP, Brazil.









 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter