

Original Article - Year 2022 - Volume 37 -
Analysis of complications from fat grafting performed at a public university hospital between 2015 and 2018: a cross-sectional retrospective study
Análise de complicações de lipoenxertias realizadas em hospital público universitário entre 2015 e 2018: estudo retrospectivo transversal
ABSTRACT
Introduction: Fat grafting consists of collecting fat from one fat donor area via liposuction, then reallocating this tissue into a receptor area through syringes and cannulas. According to the literature, it is a safe process used in aesthetic and reconstructive surgeries. The objective is to evaluate complication rates of fat grafting procedures performed in a public university hospital from 2015 to 2018 in comparison with data previously reported in the literature.
Methods: A retrospective observational study developed at a public university hospital in Campinas-SP based on the revision of medical records of patients who underwent the fat grafting procedure in this institution from 2015 to 2018.
Results: Regarding the complications, the vast majority corresponded to fat reabsorption (62%). Bruise corresponded to the second most common (38% of cases), followed by edema (19%). Pain and dyschromia followed next, with 10% and 7% of cases, respectively. Only one case of operative wound infection was described. Other less frequent complications included hyperemia (5%), asymmetries (5%), desquamation (2%), local paraesthesia (3%) and skin lesion (2%). No other larger complication was reported, such as fat embolism or severe surgical complications such as bleeding, sepsis, or anaphylaxis.
Conclusion: The procedures of liposuction for fat collection and fat grafting were proved to be safe, yielding low complication rates in the studied sample, which agrees with data reported in the literature.
Keywords: Postoperative complications; Adipose tissue; Reconstructive surgical procedures; Lipectomy; Elective surgical procedures
RESUMO
Introdução: A lipoenxertia consiste no processo de coleta de gordura de uma área doadora de gordura por meio de lipoaspiração seguida da realocação desse tecido em área receptora por meio de seringas e cânulas. É um processo seguro utilizado em cirurgias estéticas e reconstrutivas, de acordo com a literatura. O objetivo é avaliar as taxas de complicações dos procedimentos de lipoenxertia realizados em um hospital público universitário no período de 2015 a 2018, em comparação com dados previamente relatados na literatura.
Métodos: Estudo observacional retrospectivo desenvolvido em hospital universitário público de Campinas - SP a partir da revisão de prontuários de pacientes submetidos a lipoenxertia nesta instituição de 2015 a 2018.
Resultados: Em relação às complicações, a grande maioria correspondeu à reabsorção de gordura (62%). O hematoma correspondeu ao segundo mais comum (38% dos casos), seguido do edema (19%). Dor e discromia vieram em seguida, com 10% e 7% dos casos, respectivamente. Apenas um caso de infecção de ferida operatória foi descrito. Outras complicações menos frequentes foram hiperemia (5%), assimetrias (5%), descamação (2%), parestesia local (3%) e lesão cutânea (2%). Nenhuma outra complicação maior foi relatada, como embolia gordurosa ou complicações cirúrgicas graves como sangramento, sepse, anafilaxia, entre outras.
Conclusão: Os procedimentos de lipoaspiração para coleta de gordura e lipoenxertia mostraram-se seguros e com baixo índice de complicações na amostra estudada, concordando com dados da literatura.
Palavras-chave: Complicações pós-operatórias; Tecido adiposo; Procedimentos cirúrgicos reconstrutivos; Lipectomia; Procedimentos cirúrgicos eletivos
INTRODUCTION
Fat grafting is a surgical technique described in 1893 by Neuber1, which consists primarily of collecting fat through the liposuction process of a donor area, followed by the relocation of this fat in a recipient area using syringes and cannulas. It is a minimally invasive technique used worldwide and has several applications in reconstructive and aesthetic plastic surgery and other surgical specialties.
It is presented as an alternative to synthetic materials, such as hyaluronic acid for facial fillers2, in the moderate increase of breast and gluteus volume3 with silicone prostheses, in the correction of congenital and acquired deformities, scars4 and reconstructions after oncological surgeries such as mastectomies or quadrantectomies5.
In addition, it has the potential to be used in several other areas of medicine, such as ophthalmology, for the reconstruction of periorbital defects and post-enucleation ophthalmic cavity filling6; proctology, in the treatment of recurrent perianal fistulas7; and in rheumatology, as a potential local immunomodulator for autoimmune diseases8, among many others.
Fat grafting is a technique that uses autologous tissue; therefore, non-immunogenic, using the fat that can be collected through the liposuction process. In addition, it has a small percentage of complications, most of which are composed of local reactions, not threatening patients’ lives.
Such complications include local and systemic reactions, both those related to the liposuction process and the fat grafting process itself. Complications related to liposuction are usually smaller and less frequent than those observed in classic liposuction used to improve body contour since smaller volumes of liposuctioned fat are used9.
Among the most common local adverse effects are post-procedure irregularities and asymmetries, fat necrosis and formation of oily cysts (larger grafted amounts), local infection, hematomas, seromas, and hyperpigmentation, prolonged edema, ecchymosis, resorption or proliferation of fat tissue, among others10. Systemic complications include perforations of viscera or vessels during liposuction, fat embolism and fat embolism syndrome11, in addition to events that can be associated with any surgical procedure, such as hypersensitivity reactions to medications, infections, thromboembolism, etc.2,3, 12,13
Some studies considered the factors that reduce such risks, mainly concerning asymmetries, irregularities, fat reabsorption and liponecrosis. There is evidence that a delicate liposuction process, associated with the non-exposure of fat to ambient air (closed system), in addition to the previous tunneling of the graft site followed by slow application of the graft, helps in the process of fat adherence and reduces negative results both clinical and aesthetic2,3. In addition, fat grafting performed in areas of fibrosis, such as scars and areas exposed to radiotherapy, can reduce fat retention thanks to less vascularization of the tissue.
On the other hand, fat grafting itself seems to have a regenerative effect on fibrous and scar tissue thanks to its pro-angiogenic effect and possibly the differentiation and proliferation of adipocyte stem cells14,15. Some studies demonstrate that characteristics of the donor area do not seem to influence the rates of complications and fat retention in the recipient area16. Others, however, argue that the viability of fat is greater when collected from different areas according to the patient’s age17.
Despite the wide range of scientific articles published on fat grafting techniques worldwide, studies intending to evaluate this technique’s safety, efficacy and complications are mostly very heterogeneous and have low scientific evidence2.
OBJECTIVE
This study aims to evaluate the complication rates of fat grafting procedures in a public university hospital from 2015 to 2018 compared to existing data in the medical literature.
METHODS
This study consists of a retrospective observational study based on a review of the medical records of all patients undergoing the fat grafting procedure at a public university hospital in Campinas-SP, performed by the plastic surgery team from 2015 to 2018. The project was approved by the Research Ethics Committee (Protocol number [CAAE]: 08897619.6.0000.5404, Campinas - S P, Brazil, May 20, 2019).
Patients whose medical records were not located or with gaps in the medical record of the procedures that made the proposed analyses impossible, as well as patients who did not complete the treatment and maintained regular outpatient follow-up, were excluded from the analysis.
In the analysis, data were recorded regarding sex, age, the purpose of the procedure (for aesthetic or repair purposes as a way of correcting post-traumatic, surgical scars and deformities, etc.), donor area, recipient area, amount of grafted fat, the solution used for anesthesia and hemostasis, and postoperative complications for a period of up to 1 year after surgery, as well as patient satisfaction with the procedure and the need for new fat grafting.
RESULTS
Sixty-seven patients underwent fat grafting at the hospital within the stipulated period. Data were collected from 58 medical records, according to the inclusion and exclusion criteria approved by the Research Ethics Committee, totaling 145 fat grafting procedures analyzed. Of these, 87 procedures (60%) were revisional (secondary) procedures performed in 15 patients. Of the total number of patients analyzed, 39 (67%) are women, and 19 (33%) are men. Sixteen patients (28%) underwent fat grafting procedures for aesthetic purposes, all female. The mean age of patients at the first fat grafting procedure was 43 years (45 years for women and 40 for men).
Regarding the liposuction site for fat collection, in 76% (118) of the procedures, the material was collected from the abdomen, with 71% from the lower abdomen (110 procedures). The flank region was the second most used for liposuction with eight cases (5%), followed by the thigh region (seven cases) and the sacral region (four cases). The material was collected by liposuction from more than one region in four cases analyzed. Other collection regions included buttocks and back and trochanteric regions, each with one case.
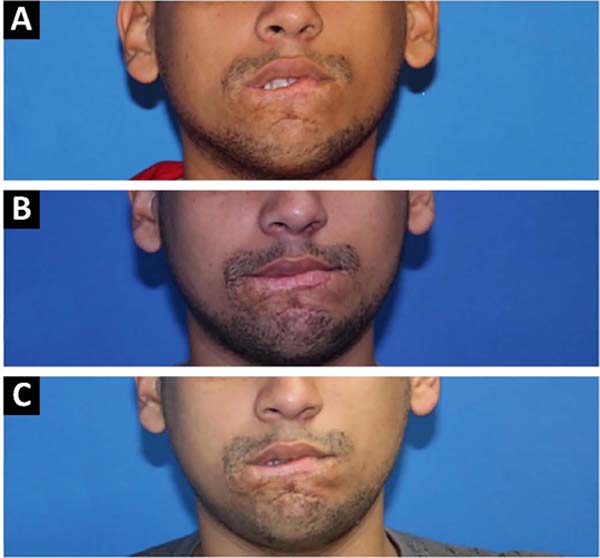
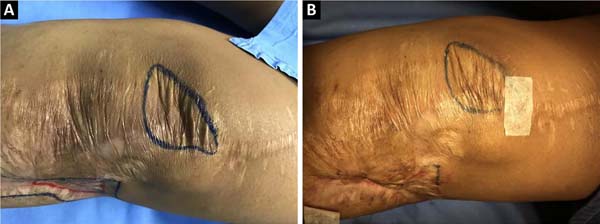
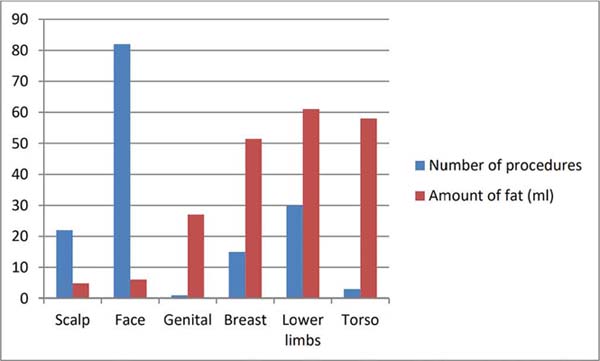
Regarding the grafting site, 82 of the procedures analyzed were performed in the face region, corresponding to 53% of the total procedures (Figure 1 shows an example of fat grafting on the face used to correct deformity after surgical resection of arteriovenous malformation in the face).
Scars and lower limb deformities were in second place, totaling 30 procedures (19%) (Figure 2 shows an example of scar depression in a post-traumatic lower limb scar treated with fat grafting). Skull and breast also corresponded to most grafting sites, with 14% and 10% of the total procedures performed. Other grafting sites included the trunk region (three cases) and the genital region (one case).
Regarding postoperative complications, the vast majority corresponded to fat resorption (62% of cases). Ecchymosis was the second most frequent complication (38% of cases), followed by edema (19%). Pain and dyschromia followed, with 10% and 7% of cases, respectively. Only one case of surgical wound infection evolving with ulceration after fat grafting in a scar on the right lower limb was described, resulting from a sequela of chronic osteomyelitis.
Other less frequent complications included hyperemia (5%), asymmetries (5%), desquamation (2%), local paresthesia (3%) and skin damage (2%) (Table 1). The insufficient repair was described in 5% of cases. No cases of major complications, such as fat embolism, or serious surgical complications, such as bleeding, infection with sepsis, or anaphylaxis, among others, were described. According to the Kruskal-Wallis test, the time between the procedure and the appearance of the complication was statistically relevant (p=0.003) (Table 2).
| Complication | Number of cases | % |
|---|---|---|
| Peeling | 1 | 2 |
| Infection | 1 | 2 |
| Skin lesion | 1 | 2 |
| Retraction | 1 | 2 |
| Ulceration | 1 | 2 |
| Paresthesia | 2 | 3 |
| Asymmetry | 3 | 5 |
| Erythema | 3 | 5 |
| Insufficient repair | 3 | 5 |
| Dyschromia | 4 | 7 |
| Prolonged pain | 6 | 10 |
| Edema | 11 | 18 |
| Ecchymosis | 23 | 38 |
| Resorption | 90 | 62 |
| Complication | Average | PD | Median | Total |
|---|---|---|---|---|
| Anesthesia | 75 | 64 | 75 | 2 |
| Resorption | 108 | 102 | 90 | 98 |
| Prolonged pain | 10 | 9 | 7 | 7 |
| Edema | 19 | 34 | 7 | 11 |
| Ecchymosis | 6 | 2 | 7 | 22 |
| Hyperchromia | 60 | 42 | 60 | 2 |
| Erythema | 34 | 37 | 34 | 2 |
| Hipocromia | 150 | 170 | 150 | 2 |
| Insufficient repair | 24 | 31 | 7 | 3 |
| Others | 14 | 11 | 10 | 4 |
The lower limbs were the grafting site with the greatest fat, averaging 61 ml. Trunk and breast also had higher mean amounts of grafted tissue, with 58ml and 51ml, respectively. In the face region, the average milliliter of grafted fat was 6ml, and, in the skull, 5ml. In cosmetic surgeries, the average amount of fat used was 11 ml, against an average of 25 ml used in reconstructive surgeries (Figure 3). According to the Mann-Whitney test, in this study, there was no significant difference between the amount of fat grafted and the complication rate (p=0.072). However, there was a trend towards a higher complication rate in larger amounts of fat grafted. (Table 3).
Fat resorption was reported in outpatient consultations in the postoperative period in 80% of breast fat grafting cases, the macro-region with the highest complaint of resorption. The region of the skull had 68% of cases with reports of resorption in consultations, followed by procedures in the trunk (67%), face (65%) and lower limbs (63%). The only procedure performed in the genital region had no report of resorption or need for re-approach. According to Fischer’s exact test, statistical analysis showed no significant difference in fat resorption from fat grafted in different sites (p=0.53) or fat removed from different donor areas (p=0.184).
DISCUSSION
Initially, it can be observed that most (67%) of the treatments performed were on female patients, and those with a purely aesthetic purpose were all on women.
However, the mean age at the first procedure was lower in male patients. We can relate this data to the fact that more than half of the men who underwent fat grafting underwent the procedure to correct post-traumatic scars and deformities (10 of 19 male patients), thus occurring in younger patients, compatible with the higher incidence of trauma.
The most frequently used sites for fat collection through liposuction were the lower abdomen (71%) and flanks (5%), in agreement with the study by Geissler et al.17 regarding the viability of fat, in which the lower abdomen and flanks were the two areas whose collected fat had lower rates of resorption and greater viability in the grafted region.
Fat resorption was the most reported complaint in postoperative medical consultations in fat grafting procedures (62% of cases). The amount reabsorbed, however, was not measured. In the literature, the difficulty in measuring fat reabsorption after the procedure is recurrently described, as well as the lack of a validated method for the same purpose.
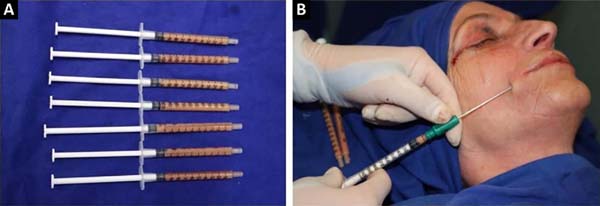
The fat survival rate can be optimized using established techniques following some predetermined principles, such as the previous tunneling of the grafted area, use of fewer caliber cannulas (Figure 4 - Fat removed with liposuction and injection with fewer caliber cannulas), and injection of small amounts of fat in order to to ensure cell imbibition, among others disseminated from the Coleman technique18, currently most used in most plastic surgery services.
In this study, there was no significant difference between the amount of fat grafted and complication rates (p=0.072). However, it showed a trend towards higher complication rates in higher amounts of fat grafted, as evidenced in most studies in the literature. A study with a larger sample of patients could show statistical relevance to this hypothesis.
However, the factors that can alter fat survival in the long term, such as changes in body mass index (BMI) and body composition, are not yet fully elucidated in the literature, as there are no validated methods for its measurement16.
In 1987, the American Society of Plastic Surgeons published a report criticizing the autologous fat transplantation method, with estimated fat survival rates of 30% after 1 year of procedure, showing concern regarding the method’s effectiveness19. Little is known about the mechanisms of fat survival, and, to date, there is no unified measurement method to measure its survival rate16.
Therefore, the study data were compatible with the literature data since resorption was reported in 62% of the analyzed cases, but there was no objective measurement method of its volume. In addition, there was a statistically significant difference between the time elapsed after the procedure and the complication rate (p=0.003).
There is a high probability that this result was directly affected by the resorption rate since fat tends to be reabsorbed over time17, and resorption was the most frequent complication. The mean time between the procedure and the report of the complication was 50 days, and 108 days for the report of resorption, indicating an adequate postoperative follow-up in our study (12 months).
If we consider fat resorption as part of the refinement process and the need for more than one procedure to achieve the final result, the complication rates become very low. Total postoperative complaints dropped from 150 to just 60 (60% drop).
Regarding the rates, only reports of minor complications such as ecchymosis, pain, edema, dyschromia, asymmetries, and under-correction, among others, were found. The most serious complication was graft site infection with tissue loss and ulceration, reported in only one case. There were no cases of major complications such as embolization, fat embolism syndrome, bleeding or death.
In a literature review, low rates of postoperative complications were found both in fat grafting procedures and liposuction procedures. In the study by Furlani & Saboia20 with 151 patients undergoing fat grafting for facial rejuvenation, only under-correction was reported, with no other complications. In the review article by Yu et al.16, only 10 cases of major complications were described in 10 years of review, the most severe being cerebral and ophthalmic artery embolization.
In the study by Maione et al.9, with 1000 patients undergoing fat grafting, only two hematomas were reported in the donor area, 83 post-liposuction deformities and four cases of infection in the recipient area. No reports of necrosis or systemic complications such as pulmonary thromboembolism or cardiorespiratory arrest. Another study, focusing on liposuction complications only, analyzed 25 years of procedure and 26,259 patients, with seroma findings in 5% of cases, irregularities and fibrosis in 2.3%, DVT and PTE with 0.03% incidence each and only 0.01% post-TEP21 mortality.
Despite the heterogeneity, the literature on fat grafting complications indicates a low incidence of adverse effects, the vast majority of which are minor complications that do not pose a risk to the lives of patients, similar to what was observed in the present study.
The degree of satisfaction with the procedure was high; however, in most cases (62%), more than one procedure was necessary for the patient to be satisfied with the result. This was also demonstrated in the study by Denadai et al.22, in which fat retention was greater after complementary procedures.
As there is no validated method to quantify fat resorption over time, patient and surgeon satisfaction, symmetry, volume, and aesthetic pleasingness, among other qualitative factors, are considered when assessing the need for a revision procedure. Because of this, it is pertinent to open a discussion on the possibility of validating the hypercorrection process in selected cases, which could reduce the number of interventions necessary to achieve the expected final result.
Resorption is still an important issue concerning the fat grafting method, and there is a need for studies that help in the quantification of resorption rates, as well as in the development of techniques that optimize the survival of fat in the medium and long term. In our study, statistical analysis showed no difference in fat resorption at different fat grafting sites or in fat from different donor areas. Liposuction performed for the collection of fat associated with fat grafting proved to be a safe technique in the analyzed sample, in agreement with the data obtained in the literature.
CONCLUSION
Liposuction procedures for fat collection and fat grafting proved safe and with enormous potential for use in plastic surgery and other areas of medicine. Considering that this technique has evidence of low serious complications and great potential for application, further research on fat grafting should be encouraged.
REFERENCES
1. Neuber F. Fettransplantation. Chir Kongr Verhandl Dsch Gesellch Chir. 1893;22:66.
2. Groen JW, Krastev TK, Hommes J, Wilschut JA, Ritt MJPF, Van Der Hulst RRJW. Autologous Fat Transfer for Facial Rejuvenation: A Systematic Review on Technique, Efficacy, and Satisfaction. Plast Reconstr Surg - Glob Open. 2017;5(12):e1606. DOI: 10.1097/ GOX.0000000000001606
3. Blumenschein A, Freitas-Junior R, Tuffanin A, Blumenschein D. Lipoenxertia nas mamas: procedimento consagrado ou experimental? Rev Bras Cir Plást. 2012;27(4):616-22.
4. Klinger M, Caviggioli F, Klinger FM, Giannasi S, Bandi V, Banzatti B, et al. Autologous fat graft in scar treatment. J Craniofac Surg. 2013;24(5):1610-5. DOI: 10.1097/SCS.0b013e3182a24548
5. Brenelli F, Rietjens M, De Lorenzi F, Pinto-Neto A, Rossetto F, Martella S, et al. Oncological safety of autologous fat grafting after breast conservative treatment: a prospective evaluation. Breast J. 2014;20(2):159-65. DOI: 10.1111/tbj.12225
6. Galindo-Ferreiro A, Khandekar R, Hassan SA, Al-Hammad F, Al-Subaie H, Artioli Schellini S. Dermis-fat graft for anophthalmic socket reconstruction: indications and outcomes. Arq Bras Oftalmol. 2018;81(5):366-70.
7. Stroumza N, Fuzco G, Laporte J, Nail Barthelemy R, Houry S, Atlan M. Surgical treatment of trans-sphincteric anal fistulas with the Fat GRAFT technique: a minimally invasive procedure. Colorectal Dis. 2017;19(8):e316-e319. DOI: 10.1111/codi.13782
8. Chen W, Xia ZK, Zhang MH, Ding GC, Zhang XY, Wang ZX, et al. Adipose tissue-derived stem cells ameliorates dermal fibrosis in a mouse model of scleroderma. Asian Pac J Trop Med. 2017;10(1):52-6. DOI: 10.1016/j.apjtm.2016.10.005
9. Maione L, Vinci V, Klinger M, Klinger FM, Caviggioli F. Autologous fat graft by needle: analysis of complications after 1000 patients. Ann Plast Surg. 2015;74(3):277-80. DOI: 10.1097/SAP.0000000000000050
10. Nakada H, Inoue M, Furuya K, Watanabe H, Ikegame K, Nakayama Y, et al. Fat necrosis after breast-conserving oncoplastic surgery. Breast Cancer. 2019;26(1):125-30. DOI: 10.1007/s12282-018-0901-5
11. Franco FF, Tincani AJ, Meirelles LR, Kharmandayan P, Guidi MC. Occurrence of fat embolism after liposuction surgery with or without lipografting: an experimental study. Ann Plast Surg. 2011;67(2):101-5. DOI: 10.1097/SAP.0b013e3181fe32b6
12. Franco FF, Basso RCF, Tincani AJ, Kharmandayan P. Complicações em lipoaspiração clássica para fins estéticos. Rev Bras Cir Plast. 2012;27(1):135-40.
13. Krastev TK, Beugels J, Hommes J, Piatkowski A, Mathijssen I, Van der Hulst R. Efficacy and Safety of Autologous Fat Transfer in Facial Reconstructive Surgery: A Systematic Review and Meta-analysis. JAMA Facial Plast Surg. 2018;20(5):351-60. DOI: 10.1001/jamafacial.2018.0102
14. Zielins ER, Brett EA, Longaker MT, Wan DC. Autologous Fat Grafting: The Science Behind the Surgery. Aesthetic Surg J. 2016;36(4):488-96. DOI: 10.1093/asj/sjw004
15. Scioli MG, Artuso S, D’Angelo C, Porru M, D’Amico F, Bielli A, et al. Adipose-derived stem cell-mediated paclitaxel delivery inhibits breast cancer growth. PLoS One. 2018;13(9):e0203426. DOI: 10.1371/j ournal.pone.0203426
16. Yu NZ, Huang JZ, Zhang H, Wang Y, Wang XJ, Zhao R, et al. A systemic review of autologous fat grafting survival rate and related severe complications. Chin Med J (Engl). 2015;128(9):1245-1251. DOI: 10.4103/0366-6999.156142
17. Geissler PJ, Davis K, Roostaeian J, Unger J, Huang J, Rohrich RJ. Improving fat transfer viability: the role of aging, body mass index, and harvest site. Plast Reconstr Surg. 2014;134(2):227-32. DOI: 10.1097/PRS.0000000000000398
18. Coleman SR. Facial recountouring with lipostructure. Clin Plast Surg. 1997;24(2):347-67. DOI: 10.1016/s0278-2391(97)90107-5
19. Report on autologous fat transplantation. ASPRS Ad-Hoc Committee on New Procedures, September 30, 1987. Plast Surg Nurs. 1987;7(4):140-1.
20. Furlani E, Saboia DB. Rejuvenescimento facial com lipoenxertia: sistematização e estudo de 151 casos consecutivos. Rev Bras Cir Plást. 2018;33(4):439-45. DOI: 10.5935/2177-1235.2018RBCP0163
21. Triana L, Triana C, Barbato C, Zambrano M. Liposuction: 25 years of experience in 26,259 patients using different devices. Aesthetic Surg J. 2009;29(6):509-12. DOI: 10.1016/j.asj.2009.09.008
22. Denadai R, Raposo-Amaral CA, da Silva SA, Buzzo CL, Raposo-Amaral CE. Complementary Fat Graft Retention Rates Are Superior to Initial Rates in Craniofacial Contour Reconstruction. Plast Reconstr Surg. 2019;143(3):823-35. DOI: 10.1097/PRS.0000000000005389
1. Universidade Estadual de Campinas, Campinas, SP, Brazil.
AS Analysis and/or interpretation of data, Statistical analysis, Final approval of the manuscript, Data Collection, Conceptualization, Conception and design of the study, Project Management, Research, Methodology, Writing - Preparation of the original, Writing - Review and Editing, Visualization.
LHZP Data analysis and/or interpretation, Final approval of the manuscript, Project Management, Writing - Preparation of the original, Writing -Review and Editing, Validation, Visualization.
JRA Data analysis and/or interpretation, Data Collection, Study conception and design, Project Management, Investigation, Methodology, Writing - Preparation of the original, Validation.
FFF Final approval of the manuscript, Conceptualization, Conception and design of the study, Project Management, Methodology, Writing - Preparation of the original, Writing - Review and Editing, Supervision, Visualization.
DRC Project Management, Writing - Review and Editing, Supervision, Validation, Visualization.
PK Project Management, Writing - Review and Editing, Supervision, Validation, Visualization
Corresponding author: Amanda Schroeder Universidade Estadual de Campinas, Cidade Universitária, Campinas, SP, Brazil Zip Code: 13083-872 E-mail: amandaschh@hotmail.com
Article received: April 07, 2021.
Article accepted: April 07, 2022.
Conflicts of interest: none.
Institution: Universidade Estadual de Campinas, Hospital de Clínicas, Departamento de Cirurgia Plástica, Campinas, SP, Brazil.










 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter