

Case Report - Year 2022 - Volume 37 -
Surgical correction of buried penis with a skin graft: case report
Correção cirúrgica de pênis embutido com utilização de enxertia: relato de caso
ABSTRACT
Introduction: Buried penis is a rare pathology related to the reduction of penile length. It is described with a higher incidence in children, but it also affects adults. This population is mainly associated with obesity and fat accumulation in the suprapubic region, being considered a pathology that is difficult to manage and treat. Surgical intervention is the basis of treatment, and the main objective is the return of urinary and sexual function. Multiple surgical techniques are described for reconstruction in patients with buried penis and must be adapted to the characteristics presented by the patient.
Case Report: This article reports the surgical technique of dermolipectomy associated with the fixation of the base of the penis in pubic symphysis and a partial skin graft to approach a patient with a buried penis.
Conclusion: The presented technique showed good functional postoperative results due to clinical improvement of the patients' initial complaints and aesthetic ones, verbalized by the patient and the legal guardian due to the patient's low cognitive level.
Keywords: Penile diseases; Surgical procedures, operative; Reconstructive surgical procedures; Urology; Case reports.
RESUMO
Introdução: Pênis embutido é uma patologia rara relacionada à redução do comprimento peniano. É descrita com maior incidência em crianças, porém acomete também adultos. Nesta população está associado principalmente a obesidade e acúmulo de gordura em região suprapúbica, sendo considerada uma afecção de difícil manejo e tratamento. A intervenção cirúrgica é a base do tratamento e o objetivo principal é o retorno da função urinária e sexual. Múltiplas técnicas cirúrgicas são descritas para reconstrução em pacientes com pênis embutido e devem ser adaptadas para as características apresentadas pelo paciente.
Relato de Caso: Nesse artigo é relatada a abordagem de um paciente com pênis embutido, utilizando-se da técnica cirúrgica de lipoaspiração superficial e dermolipectomia associada à fixação da base do pênis em sínfise púbica com o uso de enxerto de pele parcial.
Conclusão: A técnica apresentada demonstrou bons resultados funcionais pós-operatórios, devido apresentar melhora clínica das queixas iniciais do paciente, e estéticos, verbalizados pelo paciente e pela responsável legal em virtude do baixo nível cognitivo do paciente.
Palavras-chave: Doenças do pênis; Procedimentos cirúrgicos operatórios; Procedimentos cirúrgicos reconstrutivos; Procedimentos cirúrgicos urológicos masculinos; Urologia; Relatos de casos
INTRODUCTION
Buried penis is a rare pathology characterized by the normal length of the penile shaft, however, adhered to deep planes or covered by prepubic tissues. It is associated with physical and psychological morbidity due to impairments in sexual function, hygiene, and self-esteem of affected individuals1.
Its etiology can be congenital or acquired, the first being related to genetic alterations of the Dartos fascia and affecting the pediatric population. Acquired causes include radical circumcision, local trauma, recurrent infection, periscrotal lymphedema, and obesity2.
The treatment is considered difficult to manage because there is no consensus or a single surgical technique3. This article aims to present one of the techniques that can be used in the treatment: superficial liposuction and dermolipectomy of the suprapubic tissue associated with the fixation of the base of the penis in the pubic symphysis and partial skin graft for penile coverage.
This article was registered under CAAE 45028621.1.0000.5362 and approved by the Ethics Committee of the proposing institution by opinion No. 4,644,902. The Free and Informed Consent Term was obtained from the patient and his legal guardian for using information from the medical record and images.
CASE REPORT
Male patient, 30 years old, with Down syndrome, sought medical care with his legal guardian, complaining of difficulty urinating, performing intimate hygiene and recurrent episodes of local infection. On physical examination, obesity, large lipodystrophy and supralabial flaccidity were observed, with the impossibility of exposing the penile shaft, establishing the diagnosis of buried penis associated with phimosis (Figure 1).
After discussion between the teams, a joint surgical correction between Plastic Surgery and Urology was chosen.
Dissection and dermolipectomy
The patient underwent the procedure on May 11, 2020, under general anesthesia. Marking was performed in the trapezoid suprapubic region, with the lower portion of the incision in the midline 2 cm from the base of the penis so that the skin of this region can be brought closer to the pubic symphysis.
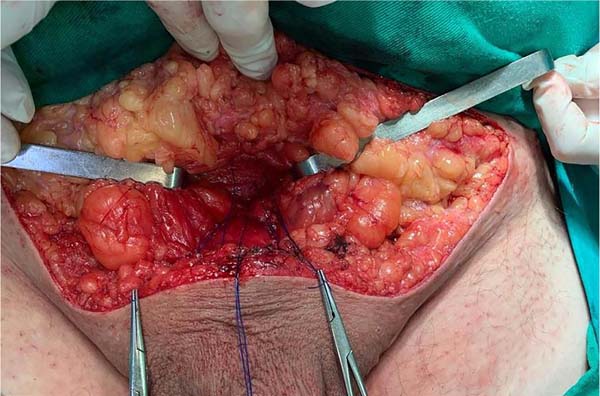
Superficial liposuction of the demarcated area was performed after infiltration with a vasoconstrictor solution (1:1,000), followed by dermolipectomy, limited to the deep fascia, without prejudice to local lymphatic drainage due to the preservation of the deep lymphatic vessels (Figure 2).
Fixation of the base of the penis to the pubis
The fascia adjacent to the base of the penis was fixed to the periosteum of the pubic symphysis with three simple stitches using 2.0 polypropylene thread, aiming at greater exposure of the penile shaft (Figure 3). A 4.8 suction drain was interposed at the liposuction and resected site. Synthesis of fascia and skin was performed in two planes with nylon 3.0 single stitches (Figure 4).
Phimosis correction
The opening of the foreskin was particularly laborious due to the firm adhesions with the glans and difficult identification of the planes due to longstanding phimosis and recurrent local infections.
We opted for resection of the foreskin due to Buck’s fascia’s pathological aspect and exposure (Figure 5). The anatomopathological examination of the resected specimen showed lichenoid dermatitis.
Grafting
A partial skin graft was removed from the right thigh with an electric dermatome, and the donor area was dressed in non-adherent gauze and dry compresses. Proximal fixation of the graft was performed at the base of the penis next to the healthy skin and distal fixation of the same next to the glans. The suture was performed with simple 4.0 polyglactin thread stitches (Figure 6).
Dressing
The dressing used was the Brown type. Long sutures were left to fix the slightly compressive dressing around the entire circumference of the penis using non-adherent gauze (Figure 7).
The patient remained with an indwelling urinary catheter, and the dressing was removed on the fifth postoperative day, being discharged after the first dressing change. He followed up with weekly outpatient visits, performing home dressings and hydrating the grafted skin with essential fatty acids. After 3 months, good graft integration, good healing of the donor area, adequate penile exposure and improved local hygiene were observed, voluntary diuresis, satisfactory flow, and absence of new infectious episodes (Figure 8).
DISCUSSION
The buried penis is associated with loss of sexual function, painful erections, poor hygiene and psychosocial disorder. It is related to voiding dysfunction due to the entrapment of urine by redundant tissue and phimosis, generating chronic cutaneous exposure to urine and dermatitis, as reported by the patient4-6. It is important to rule out differential diagnoses such as micropenis since the management of pathologies is different7. In the case described, the differentiation was made by physical examination, in which the penile shaft of normal length was palpated but without adequate exposure due to the suprapubic adipose tissue.
Multiple causes are related to the development of the disease in adults, such as local trauma, congenital lymphedema and radical circumcision involving scarring and fibrosis. Even so, obesity is the main cause in this population, a condition presented by the patient. The increase in fat, especially in the suprapubic region, creates an environment conducive to bacterial and fungal infection, leading to a self-perpetuating cycle of infection and scar contraction, conditions also present in this case5,6,8,9.
The various factors involved in the pathophysiology of the buried penis must be evaluated and addressed during treatment. In the absence of a consensus, this condition becomes a challenge for the surgeon. The main objective is the return of urinary and sexual function and may involve the joint action of the plastic surgeon and urologist. The various surgical techniques described for reconstruction must be adapted to the patient’s conditions, and many cases require a combination of procedures5.
The approach to the suprapubic tissue and lower abdomen is based on location, quantity, and etiology, with lipectomy, panniculectomy and abdominoplasty techniques being described 5,10. In patients with significant weight loss, in which the main factor involved is sagging of the lower abdominal skin, with consequent coverage of the penis, good surgical results are described with conventional or anchor abdominoplasty11.
In the technique presented, we chose to perform liposuction and suprapubic dermolipectomy due to the large amount of adipose tissue and flaccidity, with no indication for conventional abdominoplasty due to the patient’s obesity. Superficial liposuction was performed with preservation of the deep fascia, as described by Saldanha, aiming to preserve the perforating and lymphatic vessels, a technique proven to be associated with a reduction in the incidence of complications such as seroma, hematomas and skin necrosis, in addition to enabling the treatment of lipodystrophies in all regions of the abdomen12,13.
The technique presented by Figler et al.14, which served as the basis for the case presented, was associated with the fixation of the base of the penis in the pubic symphysis, aiming at better exposure of the penile shaft and maintenance of the result in the long term. Initially, there is a retraction of the skin close to this fixation suture, which in the postoperative period is gradually released, even without local conduct such as drainage and massage.
The viability of the skin of the penile shaft determines the type of technique for correction of the defect: excision and primary closure, z-plasties, flaps or skin grafts5. There was resection of the diseased skin of the foreskin and penile shaft due to local chronic inflammatory changes, with the subsequent need to cover the bloody area. A total skin graft is usually the option due to less secondary contraction and longer late nail length.15.16.
It is possible to use the skin of the foreskin or the resected skin in the dermolipectomy to obtain the graft; however, in the case presented, the first presented chronic inflammation and the second areas of dermatitis and folliculitis. A partial skin graft with a donor area in the thigh was then chosen. Postoperative care and mobilization were a concern of the team since the patient had an intellectual disability, corroborating the choice of partial graft because of its greater ease and shorter integration time.16.
The technique used showed good aesthetic and functional results in the postoperative follow-up. The patient and his legal guardian reported an important improvement in the initial symptoms, demonstrating a satisfactory result with the procedure performed.
CONCLUSION
Due to the progressive increase in the incidence of obesity, the buried penis tends to become an increasingly common pathology. Surgical intervention is the mainstay of treatment, and its approach must be individualized. The presented technique proved feasible and had favorable results concerning the patient’s initial complaints regarding hygiene, urination, and infections. Therefore, it is a good surgical option in treating buried penis.
REFERENCES
1. Smith-Harrison LI, Piotrowski J, Machen GL, Guise A. Acquired Buried Penis in Adults: A Review of Surgical Management. Sex Med Rev. 2020;8(1):150-7. PMID: 31101591 DOI: https://doi.org/10.1016/j.sxmr.2019.02.008
2. King ICC, Tahir A, Ramanathan C, Siddiqui H. Buried penis: evaluation of outcomes in children and adults, modification of a unified treatment algorithm, and review of the literature. ISRN Urology. 2013;2013:109349. DOI: https://doi.org/10.1155/2013/109349
3. Bilommi R. Hidden Penis in Children: Evaluation of Outcomes and Review of Literature. Med Surg Urol. 2015;4(4):1000156. DOI: https://doi.org/10.4172/2168-9857.1000156
4. Adham MN, Teimourian B, Mosca P. Buried penis release in adults with suction lipectomy and abdominoplasty. Plast Reconstr Surg. 2000;106(4):840-4. PMID: 11007398 DOI: https://doi.org/10.1097/00006534-200009020-00014
5. Tausch TJ, Tachibana I, Siegel JA, Hoxworth R, Scott JM, Morey AF. Classification System for Individualized Treatment of Adult Buried Penis Syndrome. Plast Reconstr Surg. 2016;138(3):703-11. PMID: 27152580 DOI: https://doi.org/10.1097/PRS.0000000000002519
6. Chopra CW, Ayoub NT, Bromfield C, Witt PD. Surgical management of acquired (cicatricial) buried penis in an adult patient. Ann Plast Surg. 2002;49(5):545-9. DOI: https://doi.org/10.1097/00000637-200211000-00017
7. Cezarino BN, Lopes RI, Machado MG, Oliveira LM, Giron AM, Tavares A, et al. Micropênis. Rev Bras Med (São Paulo). 2018;97(3):308-13. DOI: https://doi.org/10.11606/issn.1679-9836.v97i3p308-313
8. Pestana IA, Greenfield JM, Walsh M, Donatucci CF, Erdmann D. Management of “buried” penis in adulthood: an overview. Plast Reconstr Surg. 2009;124(4):1186-95. PMID: 19935302 DOI: https://doi.org/10.1097/PRS.0b013e3181b5a37f
9. Blanton MW, Pestana IA, Donatucci CF, Erdmann D. a unique abdominoplasty approach in management of “buried” penis in adulthood. Plast Reconstr Surg. 2010;125(5):1579-80. PMID: 20440190 DOI: https://doi.org/10.1097/PRS.0b013e3181d5166b
10. Ho TS, Gelman J. Evaluation and management of adult acquired buried penis. Transl Androl Urol. 2018;7(4):618-27. PMID: 30211051 DOI: https://doi.org/10.21037/tau.2018.05.06
11. Alter GJ. Pubic contouring after massive weight loss in men and women: correction of hidden penis, mons ptosis, and labia majora enlargement. Plast Reconstr Surg. 2012;130(4):936-47. PMID: 23018703 DOI: https://doi.org/10.1097/PRS.0b013e318262f57d
12. Saldanha OR, Pinto EBS, Matos Jr WN, Lucon RL, Magalhães F, Bello EML, et al. Lipoabdominoplastia - Técnica Saldanha. Rev Bras Cir Plást. 2003;18(1):37-46.
13. Saldanha OR, Azevedo DM, Azevedo SFD, Ribeiro DV, Nagassaki E, Gonçalves Junior P, et al. Lipoabdominoplastia: redução das complicações em cirurgias abdominais. Rev Bras Cir Plást. 2011;26(2):275-9. DOI: https://doi.org/10.1590/S1983-51752011000200014
14. Figler BD, Chery L, Friedrich JB, Wessells H, Voelzke BB. Limited Panniculectomy for Adult Buried Penis Repair. Plast Reconstr Surg. 2015;136(5):1090-2. PMID: 26182174 DOI: https://doi.org/10.1097/PRS.0000000000001722
15. Demzik A, Peterson C, Figler BD. Skin grafting for penile skin loss. Plast Aesthet Res. 2020;7:52. DOI: https://doi.org/10.20517/2347-9264.2020.93
16. Stephen JR, Burks FN. Buried penis repair: tips and tricks. Int Braz J Urol. 2020;46(4):519-22. PMID: 32167731 DOI: https://doi.org/10.1590/s1677-5538.ibju.2020.99.06
1. Hospital Municipal São José, Joinville, SC, Brazil
2. Universidade da Região de Joinville, Joinville, SC, Brazil
GAB Final Manuscript Approval, Project Management, Writing - Review and Editing, Supervision.
LECC Final Manuscript Approval, Project Management, Writing - Review and Editing, Supervision.
CSW Final approval of the manuscript, Data Collection, Conception and design of the study, Writing - Preparation of the original, Writing - Review and Editing.
MAB Data collection, Study conception and design, Writing - Preparation of the original, Writing - Review and Editing.
DAF Data collection, Study conception and design, Writing - Preparation of the original, Writing - Review and Editing.
Corresponding author: Djulia Adriani Frainer Rua Rio do Sul, 270, Joinville, SC, Brazil, Zip Code: 89202-201, E-mail: djuliafrainer@gmail.com
Article received: April 16, 2021.
Article accepted: July 14, 2021.
Conflicts of interest: none.


















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter