

Case Report - Year 2022 - Volume 37 -
Post-COVID-19 syndrome and plastic surgery: case report of a patient with return of respiratory symptoms in the postoperative period of reduction mammaplasty
Síndrome Pós-COVID-19 e cirurgia plástica: relato de caso de paciente com retorno de sintomas respiratórios em pós-operatório de mamoplastia redutora
ABSTRACT
Introduction: As the concept of post-COVID-19 syndrome emerges, the negative result of an RT-PCR test is no longer enough to represent a patient's complete clinical recovery. In this context, a question arises: what are the risks of performing surgery on a patient whom COVID-19 has already infected?
Case Report: Female patient, 36 years, infected by COVID-19 in December 2020, showing mild symptoms. Once asymptomatic and with a negative RT-PCR test, she was submitted to a breast reduction surgery, in January 2021, through the inferior pedicle technique by Liacyr Ribeiro and Nipple-Areolar Complex (NAC) ascension by Letterman maneuver. On the first postoperative day, the patient developed respiratory symptoms, which continued throughout the postoperative period. Despite the unsatisfactory treatment of partial necrosis of the right NAC, the patient maintained respiratory and systemic symptoms suggestive of the return of COVID-19 in the late postoperative period.
Discussion: Post-COVID-19 syndrome is defined as the persistence of symptoms of COVID-19, for at least 6 months, after the acute phase of infection. The syndrome's pathophysiology is not completely elucidated; however, a relationship with the Mast Cell Activation Syndrome is proposed. In the report, we emphasize the chronological proximity between SARS-CoV-2 infection and the return of respiratory and systemic symptoms suggestive of post-COVID-19 syndrome and the need to know the possible symptoms and complications of this syndrome, especially in the context of postoperative.
Conclusion: The need for a thorough preoperative analysis in patients with a clinical history of COVID-19 infection is evident since there is a greater risk of postoperative complications.
Keywords: Coronavirus infections; Postoperative complications; Mammaplasty; Respiratory system; Reconstructive surgical procedures.
RESUMO
Introdução: Com o surgimento do conceito de síndrome Pós-COVID-19, o RT PCR negativo, isoladamente, não deve representar a completa recuperação da doença. Nesse contexto, interroga-se: qual segurança de operar um paciente que já apresentou COVID-19?
Relato de Caso: Paciente feminina, 36 anos, apresentou COVID-19, com sintomas leves, em dezembro de 2020. Já com resultado negativo de RT-PCR e assintomática, foi submetida a mamoplastia redutora, em janeiro de 2021, utilizando-se a técnica de pedículo inferior do tipo I de Liacyr Ribeiro, com ascensão do complexo areolopapilar (CAP) pela manobra de Letterman. No primeiro dia de pós-operatório, reabriu quadro gripal sintomático e o manteve durante todo o período pós-operatório. Apesar do tratamento satisfatório da necrose parcial de CAP direito, a paciente manteve sintomas respiratórios e sistêmicos sugestivos do retorno do quadro de COVID-19 em pós-operatório tardio.
Discussão: Define-se síndrome Pós-COVID-19 como a persistência dos sintomas de COVID-19, por pelo menos 6 meses, após fase aguda da infecção. A fisiopatologia da síndrome não é completamente elucidada, todavia propõe-se relação com a síndrome de Ativação Mastocitária. No relato, ressaltamos a proximidade cronológica entre a infecção por SARS-CoV-2 e o retorno de sintomas respiratórios e sistêmicos sugestivos da síndrome Pós-COVID-19, assim como enfatizamos a necessidade de conhecer os possíveis sintomas e complicações desta síndrome, sobretudo no contexto de pós-operatório.
Conclusão: É evidente a necessidade de análise pré-operatória minuciosa em pacientes com histórico clínico de infecção pelo COVID-19, uma vez que há maior risco de complicações pós-operatórias.
Palavras-chave: Infecções por coronavírus; Complicações pós-operatórias; Mamoplastia; Sistema respiratório; Procedimentos cirúrgicos reconstrutivos
INTRODUCTION
Throughout 2020, the COVID-19 pandemic constituted a major challenge for medicine, both for diagnosing and treating patients affected by SARSCoV-2. Clinical experience gained during this period and the follow-up of infected patients in studies carried out in the US, France and China showed that some patients considered recovered, either according to clinical or laboratory factors, maintained the symptoms of COVID-19 even after the acute phase of the disease1. The persistence of clinical signs in patients who have overcome the acute phase of the virus infection led to the emergence of a new concept: the post-COVID syndrome, a term that defines the maintenance of the symptoms of the disease after at least 6 months of recovery from its acute phase2.
Most centers specializing in the treatment of COVID-19 use two tests of Reverse Transcription followed by Polymerase Chain Reaction (RT-PCR) consecutive negative, with upper respiratory tract samples collected at 24-hour intervals, to define the criteria for patient discharge or recovery. However, the emergence of the concept of post-COVID syndrome indicates that the negative result of RT-PCR isolated no longer represents the guaranteed cure of the patient but the beginning of a process of monitoring the same to control possible manifestations of the disease.
Since microbiological tests’ negative results cannot define the full recovery of symptoms, a big question arises: what is the safety of electively operating on a patient who has already had COVID-19? Therefore, to minimize the postoperative risk, it is essential to know the symptoms that may remain in the long term and their possible complications.
CASE REPORT
A 36-year-old female patient, previously healthy, started on December 11, 2020, with fever, dry cough and diffuse myalgia. On December 18, through the RTPCR exam, she confirmed the diagnosis of COVID-19. She was accompanied by a clinical doctor during this period and showed remission of all symptoms, still at the end of December 2020, without the need for hospital admission. She underwent a new RT-PCR test for SARS-CoV-2 on January 8, 2021, with a negative result. At that time, the patient was asymptomatic, and after reassessment by the clinical assistant, she was released for surgical procedure as she recovered from COVID-19.
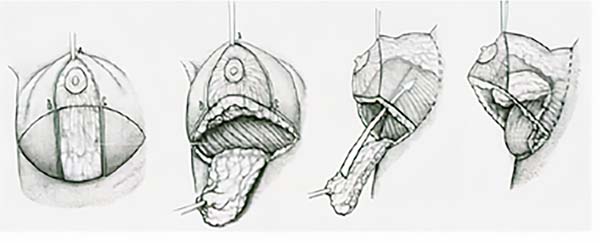
The patient underwent a reduction mammoplasty procedure at Hospital da Plástica do Rio de Janeiro, on January 14, 2021, under general anesthesia, with a total duration of 5 hours, without complications. Liacyr Ribeiro’s type I pedicle technique was used (Figure 1)3, with the ascent of the nipple-areolar complex (NAC) through the Letterman maneuver4.
On the first postoperative day, the patient had a dry cough and runny nose, symptoms that had not been reported in the preoperative period, and asymmetric swelling between the breasts, larger on the right, without signs of bleeding on examination. In addition, she had a more pale right NAC when compared to the contralateral breast (Figure 2A). As measures to improve local vascularization and reduce edema, treatment was started with: (1) 1ml of intramuscular betamethasone, single-dose, (2) 400mg of pentoxifylline and (3) 50mg of cilostazol. On the same day, the patient was discharged from the hospital with instructions to maintain the use, at home, of (1) antibiotic therapy with 875+125mg of amoxicillin + potassium clavulanate, (2) staggered analgesia with 1g of dipyrone and 10mg of trometamol ketorolac, (3) 400mg of pentoxifylline and 50mg of cilostazol and (4) vitamin C, in a daily dose of 500mg.
On the third postoperative day, still with a persistent dry cough, the patient had a darkened region on the lateral half of the right NAC, with involvement of the papilla (Figure 2B). At that moment, 100mg of acetylsalicylic acid was added to the treatment once a day to potentiate the antiplatelet action. On the fifth postoperative day, a new dose of 1 ml of intramuscular betamethasone was administered since the right breast showed only partial improvement in edema (Figure 2C).
Despite the complete improvement of the edema in the right breast and the efforts of the assistant team to improve the vascularization of the right NAC, on the 21st postoperative day, the patient presented superficial necrosis of the lateral half of the right areola without compromising the papilla (Figure 2D). At that moment, alternate treatment was started with: (1) hydrogel ointment with alginate and (2) collagenase ointment with topical chloramphenicol, aiming, respectively, for hydration and superficial debridement of the fibrin area.
On the 26th postoperative day, the patient returned for an outpatient consultation, presenting an area of f ibrin delimited in the right NAC. Mechanical debridement was performed in the region of partial necrosis of the right areola, with subsequent primary suture with complete wound closure. At that moment, she clinically presented with cough, myalgia, and diffuse pain in the lower limbs, but without signs of deep thrombosis. Palpation of peripheral arterial pulses in the lower limbs was performed, pain on palpation of the calf when compressed towards the tibia, mobility of the calf compared to the contralateral calf and Homans sign5 were evaluated, all negative. As a result of the progression of symptoms, the patient was referred again to a clinician for follow-up.
On the return for the removal of stitches, on the 33rd postoperative day, the wound presented complete closure. It should be noted that treatment with a skin graft was offered in the region of areolar necrosis; however, the patient was satisfied with the final result (Figure 3) and chose only to complement the diameter of the areola with a tattoo.
In a late consultation, on the 69th postoperative day, the patient returned to the outpatient clinic without any surgical complaints, however, she maintained a clinical picture of fatigue, myalgia in the lower limbs and episodes of dry cough. When asked about the continuation of the cough, she informed that she was followed up with a medical doctor and, despite the regular use of antihistamine medication, she did not show improvement. Therefore, she was guided through a medical report sent by the surgical team to the clinical assistant, who investigated changes in the lung parenchyma with chest computed tomography.
Clinical and surgical follow-up should be maintained for at least 12 months to assess the progression of clinical symptoms and the evolution of postoperative healing.
DISCUSSION
In fact, one of the possible unfavorable results related to the reduction mammaplasty surgery is the NAC ischemic complication, a condition that was evidenced in the immediate postoperative period of the reported case, with subsequent evolution to partial areola necrosis. The incidence of areola necrosis in mammoplasty is variable in the literature. Pinsolle et al.6 determined an incidence between 0.6 and 3.7% of this phenomenon in a review article. In 1966, Mandrekas et al.7 described an incidence of 0.8% of NAC necrosis when using the inferior pedicle technique, as performed in the report. Van Deventer et al.8 also defined the causes of NAC ischemia and necrosis as insufficient arterial supply or venous congestion, the latter being the main cause8. Thus, NAC necrosis can be an infrequent complication but is expected from the surgical procedure performed.
In addition to areola necrosis, another point that draws attention in the patient’s history is respiratory symptoms, correlated with a probable post-COVID syndrome. This condition is defined as the persistence of one or more symptoms of COVID-19, or symptoms related to the disease, for at least 6 months in patients who have recovered from the acute phase of the infection2. In patients who present this condition with an evolution period of fewer than six months, the diagnosis of Post-Infectious Fatigue Syndrome is correct2.
Lamprecht2 cites that, after infection with SARSCoV-2, 35% of outpatients and 87% of hospitalized patients are affected by the post-COVID syndrome or the Infectious Fatigue syndrome, depending on the analyzed population. Similarly, it is interesting to note that several patients developed persistent symptoms after the acute episode of infection during the SARS-CoV-1 (Severe Respiratory Distress syndrome) epidemic in 20039, especially healthcare workers. These symptoms were characterized as a syndrome of Chronic Fatigue or myalgic encephalomyelitis10, and a relationship between the maintenance of these symptoms and the development of psychological diseases was evidenced. Moderate to severe depression and anxiety were described in more than one-third of patients after one year of recovery from the initial condition11.
In patients affected by post-COVID-19 syndrome, fatigue was reported as the most important persistent symptom2,12. Its causative mechanism is still not entirely clear, but the cause is estimated to be multifactorial. In a study conducted in Egypt in 2020, Kamal et al.13 evaluated 287 patients described as survivors of the disease and of these, only 10.8% had no symptoms after recovery from the acute phase. The persistence of symptoms in the study was defined as their maintenance for at least 20 days from the last negative PCR test. A wide variety of post-COVID symptoms have been described, from mild symptoms such as persistent headache (28.9%) to severe conditions such as acute myocardial infarction, renal failure, and pulmonary fibrosis. It is worth mentioning that, among the patients who maintained the symptoms, 72.8% had persistent fatigue, 38% had anxiety, and 31.4% had joint pain13.
Psychological manifestations, as previously described in SARS-CoV-1 infection, permanent fibrotic changes in the lung parenchyma, and thromboembolic complications are also noteworthy. Kamal et al.13 also point to a possible relationship between the severity of post-COVID-19 symptoms and the initial condition of the disease; that is, the most severe cases of the initial disease had the most severe post-COVID manifestations. Galván-Tejada et al.1, in parallel, in a case-control study carried out in the city of Zacatecas, Mexico, in which they evaluated 219 patients, described dyspnea as the most important symptom to suspect post-COVID syndrome since it was absent in the control group of 78 patients.
The pathophysiology of the post-COVID syndrome not yet elucidated generates suspicion about its existence and questions about the possibility that the symptoms are the result of a reinfection framework. Among those who defend its existence, Afrin et al.14 propose that a possible basis for the post-COVID syndrome is the Mast Cell Activation Syndrome (MAS). MAS is a chronic multisystem disorder with an estimated prevalence of 17%, which is very similar to the number of COVID-19 cases that develop severe forms of the disease, between 15 and 20%. A hyperinflammatory pattern is observed in these patients, which progresses with an inflammatory cytokine storm characterized by the rapid proliferation of T lymphocytes, macrophages, and NK cells. Without leukocyte cytotoxic activity, this pattern causes cell death by activating the humoral immune system.
In inflammation, mast cells play a central role since they are responsible for synthesizing cytokines that mediate the intense immune response and regulate the activity of other cell types involved in the process14. It should be noted that a significant number of fatal cases of COVID-19 are related to cardiovascular complications, such as thromboembolism, pulmonary embolism and sepsis14, conditions whose pathophysiology involves mast cell activity.
Because of the above report, there is a correlation between the respiratory condition and previous infection by COVID-19 since these symptoms are not expected after an elective reduction mammoplasty surgery, especially in a previously healthy patient. As already pointed out, the pathophysiological mechanisms responsible for the manifestation of COVID-19 and the post-COVID syndrome are still uncertain; however, in the case mentioned above, the chronological proximity between the SARS-CoV-2 infection and the return of symptoms in the immediate postoperative period.
It is extremely important to emphasize that the clinical manifestations presented by the patient are considered mild and that the differential diagnosis of the condition could easily be achieved with the performance of complementary tests, such as imaging and laboratory tests. However, as demonstrated, there are serious outcomes reported in post-COVID syndrome, and the possibility of these conditions developing during a postoperative period represents, in practice, a diagnostic and therapeutic challenge.
Although they are not considered classic postoperative symptoms, especially in cosmetic surgery, cough and myalgia in the lower limbs should be promptly investigated, as they are possible presentations in cases of pulmonary thromboembolism and deep vein thrombosis. The presentation of deep vein thrombosis varies from the absence of symptoms to the classic presence of swelling, pain, heat, and redness in the affected extremity. Pulmonary thromboembolism, however, presents dyspnea, tachypnea, chest pain, syncope, and cough as the main symptoms15.
Hatef et al.16 showed an estimated risk of venous thromboembolism of 2.91% in patients undergoing aesthetic breast and upper extremity body contouring procedures, as reported in the case reported. Tummy tuck and circumferential tummy tuck procedures are still associated with higher risks of thromboembolism.
A wide variety of clinical and surgical complications may arise in the postoperative period, which correlates with the surgical procedure performed and the patient’s clinical factors. In times of a pandemic, a wide range of clinical presentations is added to this scenario, from mild symptoms to severe outcomes, presented by patients with previous infections by COVID-19. In this context, the question arises: could the clinical changes presented by the patient, that is, the post-COVID syndrome, increase her risk of postoperative complications? Also, to what extent could the endocrine-metabolic changes expected in the postoperative period contribute to worsening the symptoms resulting from the post-COVID syndrome?
Despite the lack of answers to most of these questions, the authors suggest that all patients who will undergo elective surgery - aesthetic or otherwise -once previously infected with SARS-CoV-2 be carefully evaluated for the presence of respiratory symptoms and systemic in the preoperative period. The presence of symptoms must be reported in the medical record and the decision to proceed with surgery, if symptoms arise in the preoperative period, is an individual decision of each surgeon.
The American Society of Anesthesiology (ASA)17, in a statement issued on December 8, 2020, suggests different periods between surgery and the initial picture of COVID-19 infection according to the severity of the condition presented and the patient’s comorbidities. The ASA also cites the possibility of residual conditions and long-term deleterious effects, both in the anatomy and myocardial function. It is worth mentioning that the post-COVID syndrome is an entity still poorly understood, with a wide range of clinical presentations, from mild symptoms to severe complications, and, due to the inherent risks of surgical procedures, we believe that such a decision should always be directed to ensure safety. of the patient, especially in elective surgeries.
CONCLUSION
Post-COVID syndrome has a recent description and still requires more robust scientific evidence to explain its pathophysiology. However, it is a fundamental clinical aspect to be analyzed in the preoperative period of patients undergoing elective procedures. As in the case reported, negative RT-PCR is not a complete guarantee of cured COVID-19 and, for this reason, a thorough clinical investigation is necessary to ensure that the history of infection by the new coronavirus is not overlooked before surgery. Therefore, it is concluded, because of the overall clinical presentation of the post-COVID syndrome, which ranges from mild symptoms to severe complications, that the additional risk of unfavorable outcomes should be evaluated in the postoperative period of patients previously infected with COVID-19.
REFERENCES
1. Galván-Tejada CE, Herrera-García CF, Godina-González S, Villagrana-Bañuelos KE, Amaro JDL, Herrera-García K, et al. Persistence of COVID-19 Symptoms after Recovery in Mexican Population. Int J Environ Res Public Health. 2020;17(24):9367.
2. Lamprecht B. Gibt es ein Post-COVID-Syndrom? [Is there a postCOVID syndrome?]. Pneumologe (Berl). 2020;17(6):398-405. German.
3. Gasperin BDM, Pavelecini M, Possamai LM, Freitas Neto FM de, Ely PB. Viabilidade do uso de retalhos de Liacyr dos tipos I e III em mastopexias com implantes em pacientes com incisão prévia no sulco inframamário. Rev Bras Cir Plást. 2018;33(Suppl.1):28-30.
4. Letterman G, Schurter M. Facilitation of the upward advancement of the nipple-areola complex in reduction mammaplasty by Kiel resection. Plast Reconstr Surg. 1981;67(6):793-5.
5. Sternbach G. John Homans: the dorsiflexion sign. J Emerg Med. 1989;7(3):287-90.
6. Pinsolle V, Tierny C, Héron A, Reynaud P, Pélissier P. Unfavorable results of reduction mammoplasty: Causes, preventions and treatments. Ann Chir Plast Esthet. 2019;64(5-6):575-82.
7. Mandrekas AD, Zambacos GJ, Anastasopoulos A, Hapsas DA. Reduction mammaplasty with the inferior pedicle technique: early and late complications in 371 patients. Br J Plast Surg. 1996;49(7):442-6.
8. van Deventer PV, Page BJ, Graewe FR. The safety of pedicles in breast reduction and mastopexy procedures. Aesthetic Plast Surg. 2008;32(2):307-12.
9. Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565-74.
10. Moldofsky H, Patcai J. Chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post-SARS syndrome; a case-controlled study. BMC Neurol. 2011;11:37.
11. Lee AM, Wong JG, McAlonan GM, Cheung V, Cheung C, Sham PC, et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry. 2007;52(4):233-40.
12. Perrin R, Riste L, Hann M, Walther A, Mukherjee A, Heald A. Into the looking glass: Post-viral syndrome post COVID-19. Med Hypotheses. 2020;144:110055.
13. Kamal M, Abo Omirah M, Hussein A, Saeed H. Assessment and characterisation of post-COVID-19 manifestations. Int J Clin Pract. 2021;75(3):e13746.
14. Afrin LB, Weinstock LB, Molderings GJ. Covid-19 hyperinflammation and post-Covid-19 illness may be rooted in mast cell activation syndrome. Int J Infect Dis. 2020;100:327-32.
15. Wilbur J, Shian B. Diagnosis of deep venous thrombosis and pulmonary embolism. Am Fam Physician. 2012;86(10):913-9.
16. Hatef DA, Kenkel JM, Nguyen MQ, Farkas JP, Abtahi F, Rohrich RJ, et al. Thromboembolic risk assessment and the efficacy of enoxaparin prophylaxis in excisional body contouring surgery. Plast Reconstr Surg. 2008;122(1):269-79.
17. ASA and APSF Joint Statement on Elective Surgery and Anesthesia for Patients after COVID-19 Infection. [Internet]. Schaumburg: American Society of Anesthesiologists. 2020 [acesso 2021 Jan 31]. Disponível em: https://www.asahq.org/about-asa/newsroom/newsreleases/2020/12/asa-and-apsf-joint-statement-on-elective-surgeryand-anesthesia-for-patients-after-covid-19-infection
1. Hospital da Plástica, Cirurgia Plástica e Reconstrutiva, Rio de Janeiro, RJ, Brazil
2. Universidade Federal do Estado do Rio de Janeiro, Rio de Janeiro, RJ, Brazil
TSG Analysis and/or interpretation of data, Acquisition of funding, Data collection, Conception and design of the study, Project Management, Carrying out operations and/or experiments, Writing - Preparation of the original, Writing - Review and Editing, Supervision.
BLC Analysis and/or interpretation of data, Data Collection, Carrying out operations and/or experiments, Writing - Review and Editing.
GLC Analysis and/or interpretation of data, Statistical analysis, Data collection, Conception and design of the study, Project Management, Writing - Preparation of the original, Writing - Review and Editing.
LPB Analysis and/or interpretation of data, Data Collection, Writing - Review and Editing.
FH Final Approval of Manuscript, Acquisition of Funding, Supervision, Viewing.
Corresponding author: Thais de Sousa Gonçalves Estrada do Galeão, 2751, sala 212, Rio de Janeiro, RJ, Brazil, Zip Code: 21931-387, E-mail: thais_sg92@yahoo.com.br
Article received: May 02, 2021.
Article accepted: May 18, 2021.
Conflicts of interest: none.








 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter