

Original Article - Year 2022 - Volume 37 -
Descriptive and temporal analysis of the mortality rate and average hospital stay due to burns and corrosion in the elderly in Brazil between 2010 and 2019
Análise descritiva e temporal da taxa de mortalidade e média de permanência hospitalar por queimaduras e corrosões em idosos no Brasil entre 2010 e 2019
ABSTRACT
Introduction: Aging leads to physical and cognitive limitations and decreased functional capacity. Therefore, there is a greater risk, a higher rate of complications and death in elderly patients from burns.
Methods: Cross-sectional and documentary study with a quantitative approach, with elderly (=60 years old) hospitalized for burns and people in Brazil (2010 - 2019) corrosion notice through the Hospital Morbidity Declaration System of Department of Informatics of the Brazilian Public Health System.
Results: The overall mortality rate for the period studied was 9%, going from 8.37% in 2010 to 8.6% in 2019. The average hospital stay in Brazil between 2010 and 2019 was 8.5 days. During this period, there was a reduction in the average number of days, from 8.6 days in 2010 to 8.1 days in 2019. The mortality rate in the elderly (9%) was higher than in the general population (2. 87%) due to the inherent weaknesses of the elderly that contribute to the elderly having a higher risk of mortality from burns. The average hospital stay found is in line with the literature, demonstrating that the higher the average hospital stays for the elderly, the higher the mortality rate.
Conclusion: Because of this, it is possible to prove the correlation between the elderly age group and the high annual mortality rate from burns. It becomes more expressive as the age group gets older.
Keywords: Burns; Aged; Hospital information systems; Public health; Unified health system; Mortality.
RESUMO
Introdução: O envelhecimento leva a limitações físicas e cognitivas, além de uma diminuição da capacidade funcional. Logo, evidencia-se maior risco, maior índice de complicações e óbito nos pacientes idosos diante de queimaduras.
Métodos: Estudo transversal e documental de abordagem quantitativa, com idosos (=60 anos) internados por queimaduras e corrosões no Brasil (2010 - 2019) notificados por meio do Sistema de Declaração de Morbidade Hospitalar do Departamento de Informática do Sistema Único de Saúde.
Resultados: A taxa de mortalidade geral para o período estudado foi de 9%, indo de 8,37% em 2010 para 8,6% em 2019. A média de internação para o Brasil entre 2010 e 2019 foi de 8,5 dias. Neste período, houve redução da média de dias, indo de 8,6 dias em 2010 para 8,1 dias em 2019. A taxa de mortalidade nos idosos (9%) foi maior do que na população geral (2,87%) devido às fragilidades inerentes à terceira idade que contribuem para que o idoso tenha um maior risco de mortalidade por queimaduras. A média de permanência hospitalar vai ao encontro da literatura, a qual demonstra que, quanto maior a média de permanência do idoso em hospitais, maior será a taxa de mortalidade deste.
Conclusão: Diante disso, é possível comprovar a correlação entre a faixa etária idosa e a alta taxa de mortalidade anual por queimaduras. Esta se torna mais expressiva à medida que o grupo etário envelhece.
Palavras-chave: Queimaduras; Idoso; Sistemas de informação hospitalar; Saúde pública; Sistema único de saúde; Mortalidade
INTRODUCTION
With the increase in life expectancy, the elderly population in Brazil has grown. Therefore, the frequency of accidents with burns in this age group also increased due to risk factors such as slowing of gait, cognitive difficulties, psychiatric disorders, chronic comorbidities, and polypharmacy. These often-limiting factors contribute to some restrictions that can favor the occurrence of functional, psychological, and aesthetic sequelae that, consequently, directly influence the prognosis and increase the mortality rate1.
In addition, it is important to note that burn injuries can occur due to chemical, thermal, radioactive, and electrical agents. Most accidents involving burns occur at home, being mostly preventable and facilitated by negligence in daily home activities2.
The growth of the elderly population also interferes with the increase in the need for hospital medical care in this age group, as they remain hospitalized for longer, presenting a worse prognosis, which results in increased mortality, data that are in line with the current study2.
According to Padua et al.1, most cases of burns occur in low-income regions that probably do not have adequate infrastructure that can help reduce the length of hospital stay and, consequently, reduce the mortality rate.
OBJECTIVES
This study aims to analyze the mortality rate and the average hospital stay of elderly patients (≥ 60 years) who are burns victims so that the appropriate public and community health sectors can be held responsible for intervening adequately, quickly, and effectively.
METHODS
This is a cross-sectional and documental study with a quantitative approach, whose epidemiological information on hospital morbidity and mortality and health indicators from January 2010 to December 2019 were obtained through the Department of Informatics of the Brazilian Public Health System (DATASUS - Departamento de Informática do Sistema Único de Saúde)3 Hospital Morbidity Declaration System.
Information on hospital morbidity and mortality was searched according to interest in the results: Burns and Corrosion (Code ICD-10: T20-T32). For this group, the following categories of analysis were specified: sex, age group, the average length of stay (in days), mortality rate and place of residence.
The graphics of the figures were made using the Pages program (Apple)TM.
RESULTS
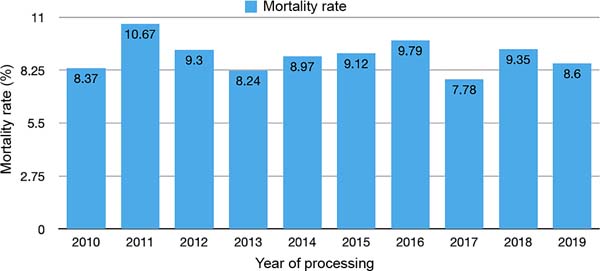
Figure 1 shows data on mortality from burns and corrosion in the elderly from 2010 to 2019, totaling 9%. There was no significant change in the mortality rate in the elderly in this time interval and in individuals younger than 60 years, who presented an overall rate of 2.87% for the period studied.
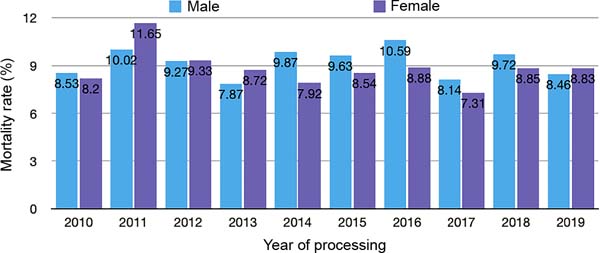
Regarding gender, the mortality rate for women was 8.77% and 9.18% for men in the period studied. Figure 2 shows inconsistent rates for men and women, showing no significant increase or decrease.
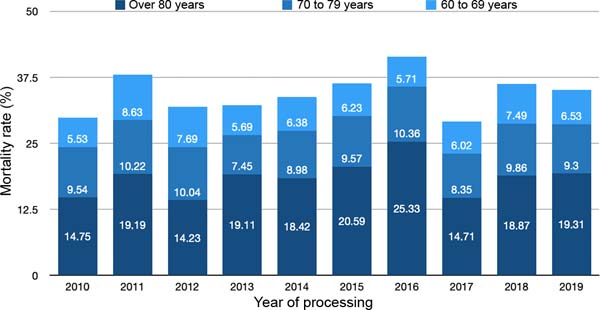
Figure 3 shows the mortality rate by age group for the period studied. In this time interval, there was a 30.91% increase in the rate for the age group over 80 years old (growing from 14.75% in 2010 to 19.31% in 2019). As for the age groups between 60 and 79 years old, no significant variations were observed.
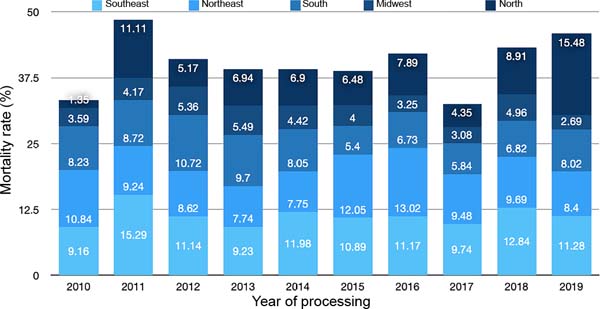
Regarding the distribution of reported cases, Figure 4 shows the mortality rate by region of the country by year of processing. The Southeast Region had the highest mortality (11.21%), followed by the Northeast Region (9.55%), South (7.68%), North (7.52%) and Midwest (4.03%). The North Region recorded the highest mortality growth rate, going from 1.35% in 2010 to 15.48% in 2019 (growth of 1046.6%).
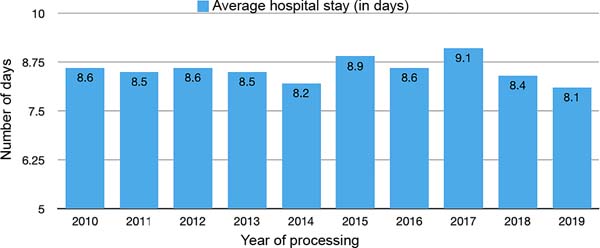
Concerning the average hospital stay, the average hospital stay for Brazil as a whole between 2010 and 2019 was 8.5 days. In this period, there was a reduction in the average number of days (0.5 day decrease), from 8.6 days in 2010 to 8.1 days in 2019. Figure 5 and Table 1 show the evolution of the average hospital stay per year in Brazil during the period studied and the average for Brazilian regions.
| Average hospital stay (in days) | |
|---|---|
| North | 9.7 |
| Northeast | 7.6 |
| Southeast | 10.4 |
| South | 7.9 |
| Midwest | 5.7 |
DISCUSSION
In Figure 1, it was observed that there was no significant variation in the mortality rate among the elderly who suffered burns between 2010 and 2019.
Regarding the mortality rate in the studied period, in the elderly (9%) it was higher than in the general population (2.87%), mainly considering that the inherent fragilities of the elderly contribute to the fact that, regardless of the treatment implemented for burns in the health service, the elderly are subject to a higher risk of mortality concerning younger individuals than 60 years with burns, especially when other chronic diseases are present, such as systemic arterial hypertension, diabetes, cardiovascular diseases, arthritis, among other conditions4, since the presence of more comorbidities is closely related to a less favorable outcome for the individual.
Furthermore, as seen in Figure 3, the age group of the elderly over 80 years old had a higher mortality rate than the others. Due to the comorbidities mentioned above, the greater the age, the greater the mortality of the elderly victim of burns. In this regard, the National Burn Repository in the United States points out that, for an index of 50-59.9% of body surface burned, the mortality rate of an older adult over 80 years of age is approximately 28 times higher compared to an older adult aged between 60 and 69 years, as complications such as urinary tract infection, pneumonia, cardiac arrest, respiratory failure, among others, become more frequent during treatment with increasing age5.
Considering each older adult’s physical and mental illnesses, increasingly individualized treatment should be implemented to control the patient’s hemostasis and prevent large volume losses, which is difficult due to the individual’s previous comorbidities.
In addition, the aging of the skin itself, which culminates in lower regenerative power and a decrease in the barrier function of the epidermis, makes it thinner and more fragile, in addition to being more susceptible to injuries6.
Regarding gender, it was observed in Figure 2 that males have the highest mortality due to burns, but the difference for females is slight. Both, when elderly, are subject to a higher risk of mortality from burns, and the prominent place of occurrence is the domestic environment, especially the kitchen, where they are prone to suffer scalds from overheated water, coffee and soups7.
Figure 4 shows the prevalence of the mortality rate in the states of the Southeast Region, followed by the Northeast Region, then the South Region, then the Center-West and, finally, the North Region. The predominance of mortality from burns in the Southeast Region is due to the region’s higher socioeconomic and health development index compared to others, resulting in a higher life expectancy for the elderly population and a percentage increase in this age group8.
In this context, it is known that the elderly have become more active and have started to live alone, regardless of the gradual and natural decrease in functional capacities, limiting them physically and cognitively. Thus, this age group becomes more exposed to the risk of accidents such as burns when performing domestic or work tasks.
There is also a progressive increase in mortality in the North region over the period evaluated. Several factors influence this variation, such as the lack of information and the sociocultural level of the population, for which, when living in poverty and overcrowded environments, the risk of burns increases. Another important issue is the existence of only one referral center for burns in the northern region, the Hospital Metropolitano de Urgência e Emergência (HMUE), located in Pará and which receives patients from both Pará and other states in the region9. Thus, several patients are subject to a prolonged interval until specialized care, increasing the risk of a negative outcome to the case, aggravated by the fact that land transport is the most used to the detriment of aeromedical support.
Furthermore, the mortality rate of each region is closely related to the capacity and infrastructure to reduce the occurrence rates and severity of burns10.
Finally, when analyzing the data presented in Figure 5, it is noted that there is no relevant variation in the average hospital stay in the evaluated period, as described when evaluating the mortality rate. This data agrees with the literature, which demonstrates that the longer the average length of stay of the elderly in hospitals, the higher their mortality rate11.
One of the observations described is that patients who suffered burns need to undergo wound debridement, which reduces the risk of infection and, consequently, the length of hospital stay. In addition, it is important to emphasize that a longer hospital stay increases the risk of contracting an infection resulting from in-hospital exposure. This can be quite harmful, especially for the elderly patient, who, due to changes in aging, the greater presence of comorbidities, and polypharmacy, among other factors, becomes more vulnerable to a negative evolution.
CONCLUSION
Given this, it is possible to prove a high mortality rate from burns in the elderly, becoming more expressive as the age group ages. In addition, it is possible to determine the relevance of the hospitalization period for the elderly population concerning the positive outcome of burn conditions. This reflection is supported by the data that an adequate conduct reduces the period related to hospitalization, reducing, in turn, the exposure to pathogens related to the hospital environment.
In this way, the importance of particularization of treatment and adequate preparation of professionals involved in the multidisciplinary care of the elderly is noted to promote more positive resolutions in these patients’ conditions.
REFERENCES
1. Padua GAC, Nascimento JM, Quadrado ALD, Perrone RP, Silva Junior SC. Epidemiologia dos pacientes vítimas de queimaduras internados no Serviço de Cirurgia Plástica e Queimados da Santa Casa de Misericórdia de Santos. Rev Bras Cir Plást. 2017;32(4):550-5.
2. Silva RV, Reis CMS, Novaes MRCG. Fatores de risco e métodos de prevenção de queimaduras em idosos. Rev Bras Cir Plást. 2015;30(3):461-7.
3. http://datasus.saude.gov.br/informacoes-de-saude/tabnet
4. Comini ACM, Lança PM, Antunes RB, Oliveira Júnior FF, Prearo SV, Vidal MA, et al. Perfil epidemiológico dos pacientes idosos queimados internados em unidade de tratamento de queimados do Noroeste paulista. Rev Bras Queimaduras. 2017;16(2):76-80.
5. Lima GL, Santos Júnior RA, Silva RLM, Cintra BB, Borges KS. Características dos idosos vítimas de queimaduras no Hospital de Urgências de Sergipe. Rev Bras Queimaduras. 2017;16(2):100-5.
6. American Burn Association (ABA). National Burn Repository 2017 Report. Chicago: ABA; 2018. 141 p.
7. Freitas LDO, Waldman BF. O processo de envelhecimento da pele do idoso: diagnósticos e intervenções de enfermagem. Estud Interdiscip Envelhec. 2011;16(Supl):485-97. DOI: https://doi.org/10.22456/2316-2171.17924
8. Cruz BF, Cordovil PBL, Batista KNM. Perfil epidemiológico de pacientes que sofreram queimaduras no Brasil: revisão de literatura. Rev Bras Queimaduras. 2012;11(4):246-50.
9. Marinho LP, Andrade MC, Goes Junior AMO. Perfil epidemiológico de vítimas de queimadura internadas em hospital de trauma na região Norte do Brasil. Rev Bras Queimaduras. 2018;17(1):28-33.
10. Serra MCVF, Sasak AL, Cruz PFS, Santos AR, Paradela EMP, Macieira L. Perfil epidemiológico de idosos vítimas de queimaduras do Centro de Tratamento de Queimados Dr. Oscar Plaisant do Hospital Federal do Andaraí - Rio de Janeiro-RJ. Rev Bras Queimaduras. 2014;13(2):90-4.
11. Moura NR, Schramm SMO. Lesões por queimaduras em idosos em um hospital de referência. Rev Bras Queimaduras. 2019;18(2):78-83.
1. Universidade de Fortaleza, Curso de Medicina, Fortaleza, CE, Brazil
AACPP Analysis and/or interpretation of data, Final approval of the manuscript, Data Collection, Conception and design of the study, Project Management, Methodology, Writing - Preparation of the original.
ESCF Statistical analysis, Acquisition of funding, Conceptualization, Conception and design of the study, Resource Management, Investigation, Conducting operations and/or experiments.
ALSP Data Collection, Conceptualization, Study Conception and Design, Resource Management, Project Management, Investigation, Methodology.
PLA Project Management, Conducting operations and/or experiments, Writing - Review and Editing, Software, Supervision, Validation, Visualization.
AAC Study conception and design, Project Management, Methodology, Writing - Document preparation, Supervision, Visualization.
TSB Resource Management, Project Management, Methodology, Conducting operations and/or experiments, Writing - Original preparation, Writing - Review and Editing, Software, Validation.
LDR Final approval of the manuscript, Conceptualization, Conception and design of the study, Carrying out operations and/or experiments, Writing - Preparation of the original, Software.
SLC Final Manuscript Approval, Data Collection, Methodology, Supervision, Visualization.
Corresponding author: Arthur Antunes Coimbra Pinheiro Pacífico, Rua Mariana Furtado Leite, 1250 - apto 1201 - torre 1, Eng. Luciano Cavalcante, Fortaleza, CE, Brazil Zip Code: 60811-030, E-mail: arthurcoimbra@edu.unifor.br
Article received: April 14, 2021.
Article accepted: December 13, 2021.
Conflicts of interest: none.








 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter