

Original Article - Year 2022 - Volume 37 - Issue 2
Burns unit at the Hospital de Clínicas of the Universidade Federal de Uberlândia, Brazil: an epidemiological study
Unidade de queimados do Hospital de Clínicas da Universidade Federal de Uberlândia, Brasil: estudo epidemiológico
ABSTRACT
Introduction: Burns, a public health problem, are injuries that can occur on the skin or other tissues of the body resulting from the trauma of thermal origin, which can cause mild, severe injuries and even death. Thus, the epidemiological characteristics of patients seen at the Burn unit of the Hospital de Clínicas of the Universidade Federal de Uberlândia are studied.
Methods: Cross-sectional study of the data recorded in patients' medical records treated for the burn at the Burn Units from 2016 to 2019.
Results: 252 medical records were reviewed, with the male gender of the adult group being most affected. The main causal agent was the flammable liquid (42.4%) with a predominance of alcohol (66.35), occurring at home (59.9%). The average percentage of burned body surface was 17.7%, requiring a graft or surgical debridement in 25% of the patients. The average hospital stay was 23.3 days, requiring 8.7% of the Intensive Care Unit. The attempt at selfextermination was 5.5%, with a general death rate of 3.5%.
Conclusions: Burn patients treated at the Burn Unit of the Hospital de Clínicas of the Universidade Federal de Uberlândia encompasses more of the young and adult population, with alcohol being the predominant cause, with an average death rate like other regions. This study will help create measures in search of reducing the number of cases and adapting the care quantitatively and qualitatively, contributing to the elaboration of care protocols to ensure the quality of the care of the patients and the population.
Keywords: Burns; Burn units; Epidemiology; Public health; Quality of life.
RESUMO
Introdução: As queimaduras, um problema de saúde pública, são lesões que podem ocorrer na pele ou outros tecidos do corpo decorrentes de trauma de origem térmica, podendo ocasionar lesões leves, graves e até mesmo o óbito. Assim, são estudadas as características epidemiológicas dos pacientes atendidos na Unidade de Queimados do Hospital de Clínicas da Universidade Federal de Uberlândia.
Métodos: Estudo transversal de dados registrados nos prontuários dos pacientes atendidos por queimadura na Unidade de Queimados de 2016 até 2019.
Resultados: Um total de 252 prontuários foram revisados, sendo mais atingido o gênero masculino da faixa etária adulta. O principal agente causal foi o líquido inflamável (42,4%), com predomínio do álcool (66,35), acontecendo no domicílio (59,9%). O percentual médio da superfície corporal queimada foi de 17,7%, precisando de enxerto ou debridamento cirúrgico 25% dos pacientes. A média de internaçação foi 23,3 dias, com 8,7% necessitando de Unidade de Terapia Intensiva. A tentativa de autoextermínio foi de 5,5%, sendo a taxa geral de óbito de 3,5%.
Conclusões: Pacientes por queimadura atendidos na Unidade de Queimados do Hospital de Clínicas da Universidade Federal de Uberlândia abrangem mais a população jovem e adulta, sendo o álcool a causa predominante, com média de óbitos similar a outras regiões. Este estudo ajudará a criar medidas no sentido de reduzir o número de casos e adequar o atendimento de forma quantitativa e qualitativa, contribuindo para a elaboração de protocolos de cuidados, a fim de assegurar a qualidade da assistência dos pacientes e da população em geral.
Palavras-chave: Queimaduras; Unidade de queimados; Epidemiologia; Saúde pública; Qualidade de vida
INTRODUCTION
Burns are injuries that can occur to the skin or other tissues of the body resulting from the trauma of thermal origin resulting from exposure or contact with flames, hot liquids, electricity, cold, chemical substances, radiation, or friction, which can lead to local or systemic changes. With partial or total destruction or compromise of adjacent tissues1,2. The extent of the damage depends on the temperature of the agent, the heat concentration and the duration of contact, as the body has few protective repair mechanisms specific to each type of burn3.
According to the World Health Organization (WHO), burns are a public health problem, being the fourth most common type of trauma, after traffic injuries, falls, and interpersonal violence2,4, which can cause mild, severe, and even minor injuries. the death.
Current global data on the number of people seeking specialized care for this type of injury are not available. However, in 2004 almost 11 million people suffered burns severe enough to require medical attention 2. Data from the American Burn Association (ABA) show that more than 450,000 people are treated annually in the United States and Canada, and in 2014, 3,275 deaths were recorded5.
According to the Brazilian Ministry of Health, in 2017, there were around 1,000,000 visits, of which 100,000 sought hospital care, and about 2,500 died directly or indirectly6. It is estimated that approximately 180,000 deaths occur every year in the world, the vast majority taking place in low- and middle-income countries 2, where up to 90% of burns occur 4. In fact, in many high-income countries, burn mortality rates have been decreasing.
OBJECTIVE
To study the epidemiological characteristics of patients treated at the burn unit (BU) of the Hospital de Clínicas of the Universidade Federal de Uberlândia (HCUFU), located in the city of Uberlândia, in the Southeast region of Brazil, the second largest municipality in the state of Minas Gerais, with a high Human Development Index (HDI 2010) (0.789), which is the referral center for burn patients in this region and follows the hospitalization criteria standardized by the Brazilian Medical Association (AMB) and the Federal Council of Medicine (CFM)1.
METHODS
A cross-sectional study of hospitalized patients and HC-UFU BU discharge data from Jan 1, 2016, to Dec 31, 2019. Patients treated or hospitalized in other services for some burn were excluded.
The analysis was performed on the data recorded in electronic and physical medical records employing frequency distribution and percentages from their tabulation and graphic representation in SPSS version 26.0.
The research was approved by the Research Ethics Committee involving human beings of Plataforma Brasil (opinion No. 4,351,266).
RESULTS
Distribution by age group, gender, and race
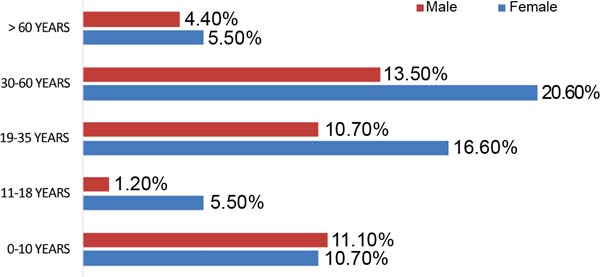
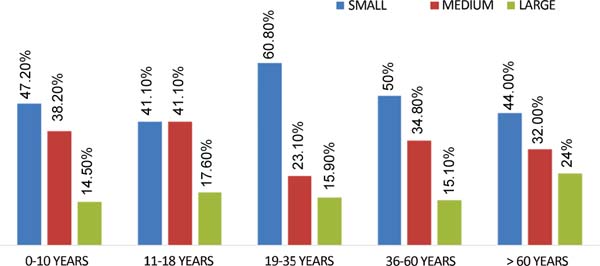
A total of 252 medical records were reviewed, corresponding to 59.1% of males and 40.8% of females, with a ratio of 1.4:1. 21.8% were children between 0 and 10 years old, 6.7% were adolescents between 11 and 18 years old, 27.3% were young people between 19 and 35 years old, 34.1% were adults between 36 and 60 years old, and 9.9% were elderly over 60 years old (Figure 1).
From the distribution by race, 48.4% were brown, 43.2% white, 7.9% black and another 0.4%.
Cities and burn environment
Patients were from the city of Uberlândia (53.1%), Patrocínio (7.9%), Araguari (7.5%), Monte Carmelo (4.7%) and other cities (26.8%).
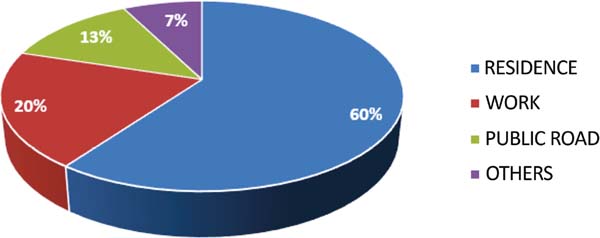
The environments where the burns occurred were the domicile (59.9%), work (19.8%), public roads (12.6%) and other places (13%) (Figure 2).
Anatomical areas of burns
Burns were categorized into four distinct anatomical areas. Upper extremities (29.6%), trunk (including buttocks and genitalia) (29.1%), lower limbs (20.9%) and head, face and neck (20.2%).
Extent of burned body surface (BBS) and degree of burns
The extent of the burn was classified as small, medium, and large, obtaining 51.1%, 32.5% and 16.2%, respectively, with an average percentage of 17.7%.
In children, small burns had SCQ below 10%, medium burns between 11-24% and large burns above 25%, with 47.2%, 38.1% and 14.5%, respectively. For adolescents, young people, and adults, 41.1%, 60.8% and 50% were considered as having minor burns (SCQ below 15%); average burn (SCQ 16-29%) 41.1%, 23.1% and 34.8%, respectively; and large burn (SCQ above 30%) 17.6%, 15.9%, 15.1%, respectively. Using the same extension categorization for the elderly, 44% were minor, 32% were medium, and 24% were major burns (Figure 3).
The general distribution by the degree of burns was 81.7% for the 2nd degree and 18.3% for the 3rd degree. In children, adolescents, young people and adults, this distribution was: 90.9%, 88.2%, 85.5% and 80.2% for the 2nd degree, respectively, and in the elderly, 52% for the 2nd degree and 48% for the 3rd degree.
Etiology of burns by age group
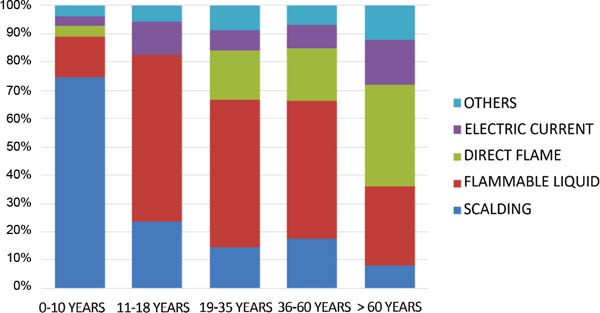
The main causes were flammable liquids, with 42.4%, scalding, 26.9%, direct flame, 16.2%, electric burn, 7.5%. Of the flammable liquids, alcohol was the agent in 66.35%, followed by gasoline, 12.1%.
In children, burns from scalding occurred in 74.5% and from flammable liquids in 14.5% (75% from alcohol). In adolescents, burns caused by flammable liquids occurred in 58.8% (60% by alcohol) and scalding in 23.5%. In young people, trauma by flammable liquids occurred in 52.1% (69.4% by alcohol) and direct flame in 17.3%. In adults, burns from flammable liquids occurred in 48.8% (76.1% by alcohol) and direct flame in 18.6%. Among elderly patients, we found direct flame in 36% and flammable liquids in 28% (42.8% for alcohol and oil) (Figure 4).
Surgical treatment
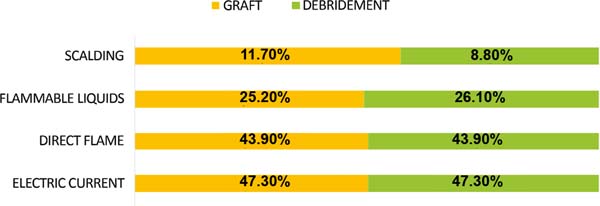
Grafting was performed in 25% of the patients, electrical causes in 47.3%, direct flame in 43.9%, flammable liquids in 25.2% and scalding in 11.7%; 24.2% also required surgical debridement, 47.3% by electric current, 43.9% by direct flame, 26.1% by flammable liquids and 8.8% by scalding (Figure 5). Required other surgical procedures 5.4%.
Hospitalization, intentionality of injury and death
The mean length of stay at the BU was 23.3 days, and 8.7% needed to stay in the Intensive Care Unit (ICU), with a mean time of 19.4 days. Intentional injuries (by other people) occurred in 7.1%, and attempted selfextermination was 5.5%. The overall death rate was 3.5%.
DISCUSSION
Burns is one of the most severe types of traumas, and their causes and associated factors differ between countries and regions, where hospital or BU data can provide useful information for establishing goals and methods in favor of their prevention and care.
This study, as well as others, carried out in UQ7,8, shows that burns affect the young and adult population more, with alcohol combustion being the major cause of hospitalization, as alcohol is the agent routinely used in our region as an energy source3,9, with hot liquid scalding included in most childhood accidents2,10 as the most frequent cause of burns in children.
As reported by the WHO2, the burns of our patients also occurred mainly in the domestic and work environment, with a predominance of male patients 11,12, which may be because men more than women perform household maintenance activities, leisure and engaged in risky professions, so they are more likely to be injured at home or at work, which would be the reason why we have more injuries in the upper limbs, similarly to what is reported in the literature11,13.
Skin grafting or surgical debridement was necessary for 25% of the patients, being more related to burns caused by electric currents and direct flame, which are the predominantly reported harmful causes13.
The percentage of attempted self-extermination (5.5%) is between the range of publications 11,14 and may have untreated or undiagnosed psychiatric pathologies as causes, with depression as the most frequent cause15.
The death rate (3.5%) was like other studies16, mainly due to the variables BBS 7 and depth of burns17.
Globally, there has been a decrease in severity, mortality, and a trend in the length of hospital stay, especially in countries with high and medium development18,19, variables that differ with this research in which the results were higher, despite our region having an HDI high.
CONCLUSION
Burn patients treated at the UQ of the HC-UFU cover more of the young and adult population, with alcohol combustion being the predominant cause, with an average of deaths similar to other regions. However, the trend toward decreasing severity, mortality and hospital stay in countries with high and medium development differs from our results, despite our region having a high HDI, so further studies are needed.
This study will help create measures to reduce the number of cases and adapt care quantitatively and qualitatively, contributing to the elaboration of care protocols to ensure the quality of care for patients at the UQ of HCUFU and the general population.
REFERENCES
1. Piccolo NS, Serra MCVF, Leonardi DF, Lima Jr EM, Novaes FN, Correa MD, et al.; Sociedade Brasileira de Cirurgia Plástica; Associação Médica Brasileira; Conselho Federal de Medicina. [Internet]. Queimaduras: Diagnóstico e Tratamento Inicial [Acesso 2008 Abr 9]. Disponível em: https://amb.org.br/files/_BibliotecaAntiga/queimaduras-diagnostico-e-tratamento-inicial.pdf
2. World Health Organization (WHO). [Internet]. Burns [Acesso 2018 Mar 6]. Disponível em: https://www.who.int/news-room/fact-sheets/detail/burns
3. Neligan PC, Gurtner GC. Cirurgia Plástica: princípios. 3ª ed. Rio de Janeiro: Elsevier; 2015.
4. GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385(9963):117-71. PMID: 25530442 DOI: https://doi.org/10.1016/S0140-6736(14)61682-2
5. American Burn Association (ABA). [Internet]. Prevention [Acesso 2018 Nov 14]. Disponível em: http://ameriburn.org/prevention/
6. Brasil. Ministerio da Saúde. [Internet]. Queimados [Acesso 2017 Jul 4]. Disponível em: https://www.saude.gov.br/component/content/article/842-queimados/40990
7. Albayrak Y, Temiz A, Albayrak A, Peksöz R, Albayrak F, Tanrıkulu Y. A retrospective analysis of 2713 hospitalized burn patients in a burns center in Turkey. Ulus Travma Acil Cerrahi Derg. 2018;24(1):25-30.
8. Duan WQ, Xu XW, Cen Y, Xiao HT, Liu XX, Liu Y. Epidemiologic Investigation of Burn Patients in Sichuan Province, China. Med Sci Monit. 2019;25:872-9. PMID: 30699102 DOI: https://doi.org/10.12659/MSM.912821
9. Dias LDF, Oliveira AF, Juliano Y, Ferreira LM. Unidade de Tratamento de Queimaduras da Universidade Federal de São Paulo: estudo epidemiológico. Rev Bras Cir Plást. 2015;30(1):86-92.
10. Baracat ECE, Paraschin K, Nogueira RJN, Reis MC, Fraga AMA, Sperotto G. Acidentes com crianças e sua evolução na região de Campinas, SP. J Pediatr (Rio J). 2000;76(5):368-74. DOI: https://doi.org/10.2223/JPED.76
11. Wolf SE, Cancio LC, Pruitt BA. Epidemiological, Demographic and Outcome Characteristics of Burns. In: Herdorn D. Total Burn Care. 5th ed. New York: Elsevier; 2018. p.14-27.e2.
12. Tian H, Wang L, Xie W, Shen C, Guo G, Liu J, et al. Epidemiologic and clinical characteristics of severe burn patients: results of a retrospective multicenter study in China, 2011-2015. Burns Trauma. 2018;6:14. PMID: 29850643 DOI: https://doi.org/10.1186/s41038-018-0118-z
13. Zikaj G, Xhepa G, Belba G, Kola N, Isaraj S. Electrical Burns and Their Treatment in a Tertiary Hospital in Albania. Open Access Maced J Med Sci. 2018;6(5):835-8. DOI: https://doi.org/10.3889/oamjms.2018.206
14. Dutra JPS, Custódio SR, Piccolo N, Daher RP. Estudo clínicoepidemiológico de pacientes queimados internados em uma unidade de terapia intensiva em Goiás. Rev Bras Queimaduras. 2017;16(2):87-93.
15. Mushin OP, Esquenazi MD, Ayazi S, Craig C, Bell DE. Self-inflicted burn injuries: etiologies, risk factors and impact on institutional resources. Burns. 2019;45(1):213-9. PMID: 30467036 DOI: https://doi.org/10.1016/j.burns.2017.07.016
16. Padua GAC, Nascimento JM, Quadrado ALD, Perrone RP, Silva Junior SC. Epidemiologia dos pacientes vítimas de queimaduras internados no Serviço de Cirurgia Plástica e Queimados da Santa Casa de Misericórdia de Santos. Rev Bras Cir Plást. 2017;32(4):550-5.
17. Greenhalgh DG. Management of Burns. N Engl J Med. 2019;380(24):2349-59. DOI: https://doi.org/10.1056/NEJMra1807442
18. Smolle C, Cambiaso-Daniel J, Forbes AA, Wurzer P, Hundeshagen G, Branski LK, et al. Recent trends in burn epidemiology worldwide: A systematic review. Burns. 2017;43(2):249-57. PMID: 27600982 DOI: https://doi.org/10.1016/j.burns.2016.08.013
19. Gurbuz K, Demir M. The Descriptive Epidemiology and Outcomes of Hospitalized Burn Patients in Southern Turkey: Age-Specific Mortality Patterns. J Burn Care Res. 2021;42(4):743-51. PMID: 33301559 DOI: https://doi.org/10.1093/jbcr/iraa206
1. Universidade Federal de Uberlândia, Uberlândia, MG, Brazil
Institution: Universidade Federal de Uberlândia, Hospital de Clínicas, Unidade de Queimados, Uberlândia, MG, Brazil.
IOGM Analysis and/or interpretation of data, Statistical analysis, Final approval of the manuscript, Acquisition of funding, Data Collection, Conceptualization, Conception and design of the study, Resource Management, Project Management, Investigation, Methodology, Carrying out the operations and/or experiments, Writing - Preparation of the original, Writing - Review and Editing, Software, Supervision, Validation, Visualization.
SSC Analysis and/or interpretation of data, Final approval of the manuscript, Data Collection, Conception and design of the study, Methodology, Writing - Preparation of the original, Writing - Review and Editing, Supervision, Validation, Visualization.
ARD Analysis and/or interpretation of data, Statistical analysis, Final approval of the manuscript, Data collection, Research, Methodology, Writing - Preparation of the original, Writing - Review and Editing.
GATOJ Analysis and/or interpretation of data, Final approval of the manuscript, Data Collection, Investigation, Carrying out operations and/or experiments, Writing - Preparation of the original, Writing - Review and Editing.
RMSC Analysis and/or interpretation of data, Final approval of the manuscript, Data Collection, Research, Writing - Preparation of the original.
Corresponding author: Iván Orlando Gonzales Mego Rua Padre Américo Ceppi, nº 673, Uberlândia, MG, Brazil, Zip Code: 38400-672 E-mail: medicogonzales@hotmail.com
Article received: April 04, 2021.
Article accepted: May 18, 2021.
Conflicts of interest: none.





 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter