

Original Article - Year 2022 - Volume 37 - Issue 2
Epidemiological profile of patients undergoing surgery to treat facial fractures in a university hospital
Perfil epidemiológico dos pacientes submetidos à cirurgia para tratamento de fratura de face em um hospital universitário
ABSTRACT
Introduction: Facial trauma presents aesthetic, social and economic relevance. Knowing its epidemiology makes it possible to formulate measures for prevention, education and systematization of care.
Methods: Research through the hospital information system, looking for patients who needed to undergo surgery for face fracture between April 2015 and April 2020. Epidemiological data were then collected.
Results: 141 patients were selected. The average age was 34 years, with most males (85%). The predominant etiology was motor vehicle accidents, and the most prevalent surgical fracture was orbit (67%). The median time between trauma and surgery was 18 days. Sixty patients had injuries associated with facial fractures, especially orthopedic and neurological injuries.
Conclusion: The most common etiology of surgical facial fractures was a traffic accident, predominantly among men. Orbit fractures were the most surgically treated.
Keywords: Facial injuries; Epidemiologic studies; Facial bones; Fracture fixation; Reconstructive surgical procedures.
RESUMO
Introdução: Trauma facial apresenta relevância estética, social e econômica. Conhecer sua epidemiologia permite formular medidas de prevenção, educação e sistematização de atendimento.
Métodos: Triagem, através do sistema de informação hospitalar, buscando pacientes que necessitaram de cirurgia para fratura de face entre abril de 2015 e abril de 2020. Foram, então, coletados dados epidemiológicos.
Resultados: Foram selecionados 141 pacientes. A média de idade foi 34 anos, com maioria do sexo masculino (85%). A etiologia predominante foi acidente com veículo automotor e a fratura cirúrgica mais prevalente foi a de órbita (67%). A mediana de tempo entre o trauma e a cirurgia foi de 18 dias. Sessenta pacientes apresentaram lesões associadas à fratura de face, com destaque para as ortopédicas e neurológicas.
Conclusão: A etiologia mais comum de fraturas faciais cirúrgicas foi acidente de trânsito, sendo o sexo masculino mais afetado. As fraturas de órbita foram as mais tratadas cirurgicamente.
Palavras-chave: Traumatismos faciais; Estudos epidemiológicos; Ossos faciais; Fixação de fratura; Procedimentos cirúrgicos reconstrutivos
INTRODUCTION
Traumas caused by external causes had a significant increase in the hospitalization rate in the Unified Health System (SUS) in the last decade1. In this context, facial fractures have presented an increasing frequency. Due to their anterior body projection, the facial skin and bones are extremely exposed in motor vehicle accidents and victims of urban violence. The etiology of facial trauma, as well as its epidemiological profile, is quite varied2.
According to the World Health Organization (WHO), approximately 1.2 million people die in traffic every year. Annually, the number of seriously injured varies from 20 to 50 million people. Traffic accidents are the leading cause of death in the 15-29 age group. Most of these deaths (90%) are concentrated in low- and middleincome countries. In Brazil, in 2013, approximately 40 thousand people died in traffic accidents. This number has grown in recent years3.
From 2000 to 2015, there was a 33% increase in fatalities in land transport accidents in Brazil. Of the 38,651 deaths, 31.4% were motorcyclists. The social and economic impact is great. In 2013 alone, the Unified Health System (SUS) recorded 170,000 hospitalizations due to land accidents, with a final cost of approximately BRL 231.5 million. Furthermore, in underdeveloped countries, high rates of urban and domestic violence contribute to increasing the social and economic impact of trauma4.
Since the face is the true region of expression of the soul, in which all feelings are represented, knowledge of the particularities of facial trauma is important, as it definitively compromises the life of the human being and, when poorly addressed, leaves sequelae, marginalizing the individual from the social interaction, generating work incapacity, condemning him to economic segregation5.
Facial fractures commonly result in injuries to soft tissues, teeth, mandible, maxilla, zygoma, nasal bones, naso-orbito-ethmoidal complex and supraorbital structures6. Proper treatment reduces the possibility of permanent deformities, which bring aesthetic, emotional and functional sequelae. Thus, detailed anatomical knowledge of facial structures is essential to obtain an accurate diagnosis and the best form of intervention. Advances in facial imaging and the improvement of evidence-based surgical indications have led to a reassessment of time-honored techniques and guidelines.
Epidemiological data on facial fractures are also essential to warn about diagnoses and draw attention to the management of these injuries and the need to carry out preventive campaigns aimed at the population. Furthermore, they contribute to the planning and assessment of collective health7. Given the relative frequency of this type of trauma in trauma centers and the socio-cultural changes, this study aims to trace the epidemiological profile of patients treated by the Plastic Surgery service of a teaching hospital in a city in the interior of the state of São Paulo between April 2015 and April 2020.
OBJECTIVE
To carry out an epidemiological survey of facial trauma with a diagnosis of facial fracture that were surgically treated among patients treated at the Plastic Surgery Service of the Universidade Estadual de Campinas (UNICAMP), in Campinas-SP.
METHODS
A retrospective epidemiological study was carried out at the Hospital de Clínicas da UNICAMP (HCUNICAMP), located in Campinas-SP, a university hospital.
The initial selection of patients was obtained through the registry of surgeries extracted from the HCUNICAMP Information System. After identifying all facial fracture surgeries performed between April 2015 and April 2020, there was an individual consultation of the medical records of each of the patients selected for the study.
Two examiners performed data collection, both resident physicians in the Plastic Surgery discipline, previously calibrated for standardized data collection.
Only patients who had a complete record in medical records related to facial fractures were included in the study, including trauma etiology, gender and age of the patient, the topography of facial fractures, comorbidities, treatment instituted, need for admission to the Intensive Care Unit (ICU) ) at some point during hospitalization and surgical complications. Participants who did not include the data proposed by the protocol and patients who only had dentoalveolar fractures were excluded from the study. This series did not include reductions in nasal bone fractures performed in an outpatient setting or an emergency room.
The data were submitted for descriptive analysis and quantitative, represented by mean, median, and percentages using Microsoft ExcelTM software.
Patients who are still undergoing outpatient followup or who have been contacted by telephone signed the Free and Informed Consent Term (FICT). Patients who no longer undergo outpatient follow-up and those not located (via telephone, contact with the social service, among other ways) were exempted from signing the informed consent. The Ethics Committee approved this work of the Universidade Estadual de Campinas under the Certificate of Presentation of Ethical Appreciation: 33327220.2.0000.5404.
RESULTS
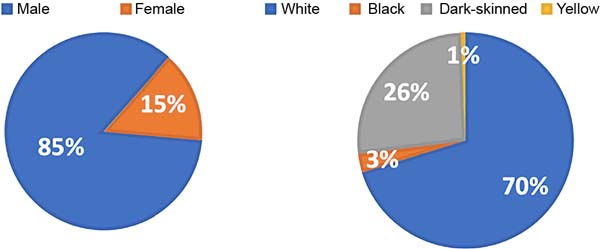
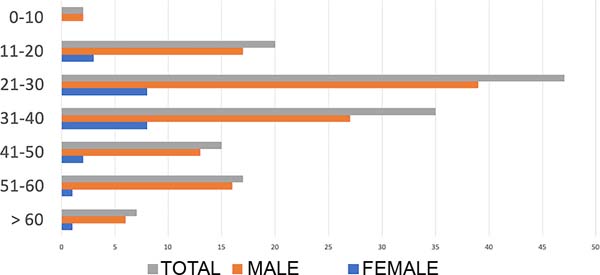
One hundred forty-seven patients who underwent surgery to correct a facial fracture in the period mentioned above were selected. Six patients were excluded from the study, as four had incomplete medical records, and two refused to sign the informed consent. A total of 141 patients were included, 120 (85%) male and 21 female (15%) (Figure 1). The gender ratio was approximately 6:1. The mean age was 34.3 years (ranging from 5 to 77 years), with a median of 32 years and 26 years (Figure 2). Ninety-nine (70%) patients declared themselves white, 37 (26%) brown, 4 (3%) black and 1 (1%) yellow.
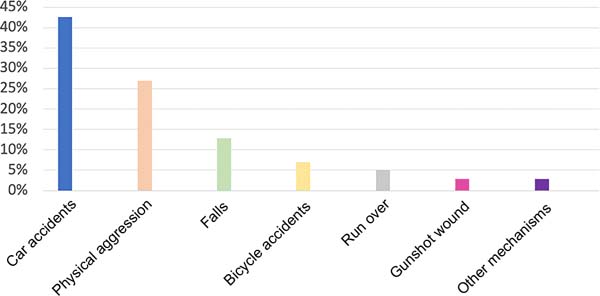
As for the etiology of the trauma, 60 (42%) suffered accidents with motor vehicles, 38 (27%) were victims of physical aggression, 18 (13%) suffered falls, 10 (7%) bicycle accidents, 7 (5%) being run over, 4 (3%) firearm injuries and 4 (3%) other mechanisms (Figure 3).
In the analysis of CT scans of facial bones performed after the trauma, we obtained the following results: 17 (12.0%) patients fractured the frontal bone, 95 (67%) the orbit - 30 exclusively in the right orbit, 38 the left and 27 bilaterally; 46 (32%) fractured the zygoma - 17 exclusively on the right, 24 exclusively on the left and 5 bilaterally; 38 (28%) fractured the nasal bone; 79 (56%) fractured the maxilla - 22 exclusively on the right, 34 exclusively on the left and 23 bilaterally; 58 (41%) fractured the mandible; 2 (1%) fractured the sphenoid bone; 2 (1%) fractured the temporal bone (both on the right) (Figure 4).
The mean time between trauma and surgery was 40.4 days (median: 18 days), with the shortest time being 0 days and the longest being 910 days. Thirty-one (22%) patients had some comorbidity, the most common being: hypertension (12) and smoking (9). Twenty (14%) patients had some complications from the surgery, the most frequent being: surgical wound dehiscence and titanium plate extrusion (5 patients with each complication). Other complications included: visual changes, surgical wound infection (FO), granuloma, palate fistula, lipodystrophy, periorbital cellulitis, and conjunctival hematoma.
Thirty-one (22%) patients had some sequel, predominantly ectropion and visual alteration. Thirty (21%) patients required the ICU after the trauma, with a mean hospital stay of 10 days. Sixty (43%) patients had injuries associated with facial fractures, the most common being orthopedic and neurological injuries. Thirty-six (26%) patients underwent surgery by other specialties during therapy. Fifteen (11%) patients had reports of alcohol ingestion in their records prior to the traumatic event.
DISCUSSION
The face is prone to different types of aggression. Thus, facial trauma assumes a prominent role in emergency care worldwide. The manifestations of facial fractures may vary according to gender, ethnicity, age and socioeconomic status5.
In this study, a significant difference was found between the male and female patients undergoing surgery to reduce and fix facial fractures. Approximately 85% of patients were male. The male-female ratio was approximately 6:1. These data are consistent with those found in the literature. Studies show ratios of 16.9:1, 14:1, 5.5:1, 8.2:1, 5.3:1 8-12. Several reasons can explain the higher incidence of facial fractures in men: men are more frequent drivers, especially on highways, a higher rate of drug abuse, and a greater tendency to get involved in accidents/fights2.
Although the male-female ratio remains high, we have seen a decrease in this ratio in recent years. In the last three decades, there has been a significant increase in the incidence of trauma in women, especially younger ones. This is due to the change in female behavior in society, including an increase in the number of female drivers, greater inclusion of women in the labor market, an association between alcohol and driving, and the practice of sports that involve physical contact2,6. Despite the increasing number of traumas among women, there are few cases with most female victims13.
The most prevalent ethnicity was white, followed by brown, black and yellow. Few epidemiological articles analyzed addressed this topic. A study carried out in Salvador-BA in 2008 showed a higher incidence of facial trauma in browns and blacks13. This difference can be explained by the fact that our study was carried out in Campinas-SP, whose ethnic composition is mostly white, while the other study was carried out in Salvador-BA, whose population is mostly mixed race14.
Regarding the etiology of the trauma, the most common mechanism was that related to motor vehicles, followed by physical aggression. In Brazil, traffic accidents and aggressions predominate as the main mechanisms related to facial trauma2,5-7. In Europe, the main trauma mechanisms include sports accidents, especially cycling accidents15,16. Another important factor that can influence the increase of a certain mechanism, to the detriment of others, is the hospital where the study is being carried out. This is what the study carried out by Motta in 200917 suggests, which presented the fall as the main mechanism of trauma. According to the author, the fact that the study was carried out in a secondary hospital contributed to this result since serious traumas, such as car accidents, are rare.
The results of this research are consistent with what is found in the Brazilian literature on the etiology of trauma. In Brazil, accidents with motor vehicles and physical aggression correspond to the main causes of facial trauma5-7,13,18,19. This can be explained by the fact that Brazil has high and growing socioeconomic inequality, with a high rate of unemployment, low education and abuse of licit substances, such as alcohol or illicit substances13.
The most fractured structure was the orbit, followed by the maxilla, mandible, zygoma, nasal bone, frontal bone, sphenoid, and temporal. The literature is quite varied in this regard. A study carried out in Austria with 14,654 patients also found the orbit to be the most fractured structure15. Other studies point to the nasal bone as the most fractured6,17. The nasal bone is the most prominent structure on the face. This characteristic, associated with the fragility of the nasal bone, makes this segment prone to fracture in trauma17. Therefore, many authors consider it the most fractured facial bone in trauma.
In our study, the low incidence of nasal fractures can be explained by two reasons: only patients who underwent surgery to correct a facial fracture under general anesthesia. Not all patients who present a nasal fracture have indications for surgical intervention for its correction. In addition, in our service, many cases of nasal bone fractures are treated with a reduction in an outpatient setting, with local anesthesia and sedation when necessary. These patients treated on an outpatient basis were not included in this series.
The mean time between the trauma and the surgical procedure was 40.4 days. This data is above that found in the literature17,20,21. This occurred because, in some cases, conservative treatment was initially chosen; however, surgical intervention proved necessary during follow-up. In some cases, patients had prolonged hospitalization due to the severity of the condition, requiring ICU and surgical intervention by other specialties, causing facial fracture surgery to be postponed until stabilization of the patient’s clinical condition or treated as a sequel in varied time, but usually for more than one month after the trauma. For comparative purposes, we can use the median found in our work, 18 days, which more faithfully represents the mean time between trauma and surgical intervention. This time is slightly higher than the average found in the literature, but it is within an acceptable time interval for treating fractures17,20.
Approximately 14% of patients had some complications. This rate is higher than the 5.8% and 7.4% presented in other works by Brazilian authors17,22. We believe that one of the factors contributing to this high rate is the fact that the study was carried out in a university hospital, a regional reference, where highly complex cases are often referred to. The high rates of ICU admission (21%), associated injuries (43%) and surgical procedures performed by other specialties (26%) demonstrate the challenging scenario of traumas treated in our service.
Only 11% of patients reported drinking alcohol before the trauma. In the literature, the relationship between alcohol use and facial fractures is well described17,22. This information is collected in trauma care with the patient, who may omit or lie about this data. In addition, there is no routine test that evaluates the amount of alcohol in the body. Furthermore, possibly in the high-demand emergency room scenario, medical records are often not detailed, making it difficult to tabulate these data. Therefore, we believe that this information is underestimated in our work.
When analyzing the age distribution of our patients, we observed that most of them are between 20 and 40 years old. Traditionally, it represents the age group with the highest risk of trauma, as young people, especially men, tend to have higher risk behavior than children, adolescents and the elderly7. In no age group analyzed, there was a predominance of females. This study did not explain the distribution between fracture etiology and age group. However, a greater number of victims of accidents with motor vehicles and victims of aggression are expected in young people and a greater number of falls in the elderly5.
CONCLUSION
Traffic accidents predominantly caused surgical facial fractures, followed by physical aggression and falls. The victims were male in 85% of the cases, and the mean age of the patients was 34.2 years. Orbit fractures were the ones that most required surgical treatment. The epidemiological data are important for the Institution that seeks an improvement in the measures of prevention, education, and systematization of care.
REFERENCES
1. Luna EJA, Silva Jr. JB. Doenças transmissíveis, endemias, epidemias e pandemias. In: Fundação Oswaldo Cruz. A saúde no Brasil em 2030 - prospecção estratégica do sistema de saúde brasileiro: população e perfil sanitário. Rio de Janeiro: Fiocruz/Ipea/Ministério da Saúde/ Secretaria de Assuntos Estratégicos da Presidência da República; 2013.
2. Montovani JC, de Campos LM, Gomes MA, de Moraes VR, Ferreira FD, Nogueira EA. Etiology and incidence facial fractures in children and adults. Braz J Otorhinolaryngol. 2006;72(2):235-41.
3. Brasil. Ministério do Trabalho e Previdência Social. Boletim Epidemiológico 2. O Impacto dos Acidentes de Trânsito para a Previdência Social. [Internet]. Brasília: Ministério do Trabalho e Previdência Social; 2016. 10 p. Disponível em: http://sa.previdencia.gov.br/site/2017/03/3%C2%B0-Quadrimestre-Boletim-2-ImpactoAcidentes-de-Tr%C3%A2nsito.pdf
4. Dahlberg LL, Krug EG. Violência: um problema global de saúde pública. Ciênc Saúde Colet. 2006;11(Suppl):1163-78.
5. Falcão MFL, Segundo AVL, Silveira MMF. Epidemiológico de 1758 Fraturas Faciais Tratadas no Hospital da Restauração, Recife/PE. Rev Cir Traumatol Buco Maxilo Fac. 2005;5(3):65-72.
6. Ramos JC, Almeida MLD, Alencar YCG, Sousa Filho LF, Figueiredo CHMC, Almeida MSC. Epidemiological study of bucomaxilofacial trauma in a Paraíba reference hospital. Rev Col Bras Cir. 2018;45(6):e1978.
7. Mendes N, Ferreira BCB, Bracco R, Martins MAT, Fonseca EV, Souza DFM. Perfil epidemiológico dos pacientes portadores de fraturas de face. Rev Assoc Paul Cir Dent. 2016;70(3):323-9.
8. Adekeye EO. The pattern of fractures of the facial skeleton in Kaduna, Nigeria. A survey of 1,447 cases. Oral Surgery Oral Med Oral Pathol. 1980;49(6):491-5.
9. Abiose BO. The incidence and management of middle third facial fractures at the University College Hospital, Ibadan. East Afr Med J. 1991;68(3):164-73.
10. Brusati R, Biglioli F, Salvato G. Maxillofacial fractures sustained during sports. Eur J Sport Traumatol Relat Res. 1998;20(1):15-22.
11. Hill CM, Burford K, Martin A, Thomas DW. A one-year review of maxillofacial sports injuries treated at an accident and emergency department. Br J Oral Maxillofac Surg. 1998;36(1):44-7.
12. Lobo SE, Marzola C, Toledo Filho JL, Pastori CM, Zorzetto DLG. Incidência e tratamento de fraturas do côndilo da mandíbula no Serviço de Cirurgia e Traumatologia Bucomaxilofacial da Faculdade de Odontologia de Bauru da Universidade de São Paulo e Associação Hospitalar de Bauru, no período de 1991 a 1995. Rev Odontol Ciênc. 1998;13(25):7-38.
13. Santos MS, Almeida TF, Silva RA. Traumas faciais: perfil epidemiológico com ênfase nas características sociais e demográficas e características da lesão, Salvador, BA, 2008. Rev Baiana Saúde Pública. 2013;37(4):1003-14.
14. Brasil. Instituto Brasileiro de Geografia e Estatística (IBGE). Estudos Sociodemográficos e Análises Espaciais Referentes aos Municípios com a existência de Comunidades Remanescentes de Quilombos - Relatório Técnico Preliminar. Rio de Janeiro: IBGE; 2007.
15. Kraft A, Abermann E, Stigler R, Zsifkovits C, Pedross F, Kloss F, et al. Craniomaxillofacial trauma: synopsis of 14,654 cases with 35,129 injuries in 15 years. Craniomaxillofac Trauma Reconstr. 2012;5(1):41-50.
16. van Hout WM, Van Cann EM, Abbink JH, Koole R. An epidemiological study of maxillofacial fractures requiring surgical treatment at a tertiary trauma centre between 2005 and 2010. Br J Oral Maxillofac Surg. 2013;51(5):416-20.
17. Motta MM. Análise epidemiológica das fraturas faciais em um hospital secundário. Rev Bras Cir Plást. 2009;24(2):162-9.
18. Vasconcelos B, Rodolfo Neto C, Silva A. Perfil epidemiológico de pacientes submetidos a tratamento cirúrgico no hospital de urgências de Goiânia - Hugo. In: Almeida DRMF, org. Odontologia: Tópicos em atuação odontológica. São Paulo: Editora Científica Digital; 2020. p. 115-35. DOI: 10.37885/201001800.
19. Minari IS, Figueiredo CMBF, Oliveira JCS, Brandini DA, Bassi APF. Incidence of multiple facial fractures: a 20-year retrospective study. Res Soc Dev. 2020;9(8):e327985347.
20. Guidi MC. Estudo retrospectivo das fraturas faciais atendidas pela disciplina de cirurgia plástica FCM - UNICAMP no período de maio de 1994 a maio de 2001 [Dissertação de mestrado]. Campinas: Universidade Estadual de Campinas (UNICAMP); 2002.
21. Thaller SR, Kawamoto HK. Care of maxillofacial injuries: survey of plastic surgeons. Plast Reconstr Surg. 1992;90(4):562-7.
22. Brasileiro BF, Passeri LA. Epidemiological analysis of maxillofacial fractures in Brazil: A 5-year prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102(1):28-34.
1. Universidade Estadual de Campinas, Hospital de Clínicas, Departamento de Cirurgia,
Campinas, SP, Brazil
2. Universidade Cidade de São Paulo, São Paulo, SP, Brazil
LHZP Analysis and/or interpretation of data, Statistical analysis, Final approval of the manuscript, Conceptualization, Conception and design of the study, Project Management, Research, Methodology, Writing - Original preparation, Writing - Review and Editing.
BBS Analysis and/or interpretation of data, Statistical analysis, Final approval of the manuscript, Conception and design of the study, Project Management, Research, Methodology, Writing - Preparation of the original, Writing - Review and Editing, Visualization.
RCFB Statistical analysis, Final approval of the manuscript, Data Collection, Conceptualization, Conception and design of the study, Supervision, Visualization.
FFF Study conception and design, Research, Visualization.
TFCA Investigation, Carrying out operations and/or experiments, Visualization.
RCP Project Management, Operations and/or Experiments.
RBS Carrying out operations and/or experiments.
PK Writing - Preparation of the original, Supervision, Visualization.
Corresponding author: Luiz Henrique Zanata Pinheiro Cidade Universitária Zeferino Vaz - Barão Geraldo, Campinas, SP, Brazil, Zip Code: 13083-970, E-mail: henriquez_pinheiro@hotmail.com
Article received: May 12, 2021.
Article accepted: July 14, 2021.
Conflicts of interest: none.







 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter