

Original Article - Year 2022 - Volume 37 -
Contrast between surgical treatment of obesity and postbariatric plastic surgeries
Contraste entre o tratamento cirúrgico da obesidade e cirurgias plásticas pós-bariátricas
ABSTRACT
Introduction: Obesity is a disease of epidemic proportions associated with increased morbidity and mortality. Gastroplasty is searched for sustained weight loss with improved quality of life as an alternative treatment. Repairing surgeries are searched after by more than 70% of patients to improve results. The study describes the number of hospitalizations for bariatric surgery and body contour surgery in postbariatric patients in Bahia.
Methods: Observational cross-sectional study with aggregated data obtained through the Department of Informatics of the Ministry of Health carried out from 2009 to 2019 in Bahia. Cases of hospitalization for bariatric surgery and postbariatric body contour surgery were included, in addition to the average length of stay of postbariatric patients hospitalized for body contour surgery and the total amounts spent per patient in gastroplasty with intestinal bypass abdominal dermolipectomy.
Results: 124 patients admitted for postbariatric surgery were identified: 64 for abdominal dermolipectomy, 25 for crural dermolipectomy, 22 by brachial dermolipectomy, and 13 by mammoplasty. The average hospital stay for postbariatric surgeries ranged from 1.5 to 4.2 days, with abdominal dermolipectomy having the highest total average: 2.8 days. Six hundred three hospitalizations for bariatric surgery were recorded. The average total amount spent per patient in gastroplasty with intestinal derivation was R$5,767.95, whereas abdominal dermolipectomy registered R$973.30.
Conclusions: 124 hospitalizations for body contouring surgeries were identified during the period 2009-2019 in the state of Bahia
Keywords: Obesity; Bariatric surgery; Reconstructive surgical procedures; Public health; Abdominoplasty.
RESUMO
Introdução: A obesidade é uma doença de proporções epidêmicas associada ao aumento da morbidade e mortalidade. Como alternativa de tratamento, a gastroplastia é procurada para uma perda de peso sustentada com melhora da qualidade de vida. As cirurgias reparadoras são procuradas por mais de 70% dos pacientes para o aperfeiçoamento dos resultados. O estudo visa descrever o número de internamentos por cirurgias bariátricas e por cirurgias de contorno corporal em pacientes pós-bariátricos na Bahia.
Métodos: Estudo observacional transversal com dados agregados obtidos através do Departamento de Informática do Ministério da Saúde e realizado no período de 2009-2019 no estado da Bahia. Foram incluídos casos de internamentos por cirurgias bariátricas e por cirurgias de contorno corporal pósbariátricas, além da média de permanência dos pacientes pós-bariátricos internados pelas cirurgias de contorno corporal e os valores totais gastos por paciente na gastroplastia com derivação intestinal e na dermolipectomia abdominal.
Resultados: Foram identificados 124 pacientes internados por cirurgia pós-bariátrica: 64 por dermolipectomia abdominal; 25 por dermolipectomia crural; 22 por dermolipectomia braquial e 13 por mamoplastia. A média de permanência do internamento das cirurgias pós-bariátricas variou de 1,5 a 4,2 dias, sendo que a dermolipectomia abdominal apresentou a maior média total: 2,8 dias. Foram registrados 603 internamentos por cirurgia bariátrica. A média dos valores totais gastos por paciente na gastroplastia com derivação intestinal foi de R$ 5.767,95, já a dermolipectomia abdominal registrou R$ 973,30.
Conclusões: são identificados 124 internamentos por cirurgias de contorno corporal durante o período 2009-2019 no estado da Bahia.
Palavras-chave: Obesidade; Cirurgia bariátrica; Procedimentos cirúrgicos reconstrutivos; Saúde pública; Abdominoplastia
INTRODUCTION
Obesity is a disease of epidemic proportions in Brazil and in the world that is associated with increased morbidity and mortality1,2. In addition, it contributes to a reduction in life expectancy and quality of life, mainly caused by functional limitations and low self-esteem1-4. However, in most obese patients, conventional treatment, such as food restriction, is ineffective in the long term, greatly increasing the application of interventional therapy: bariatric surgery5.
In addition to a sustained weight loss of 40 to 60% of the initial weight, gastroplasty provides a better lifestyle and significantly reduces risk factors for comorbidities associated with obesity2,6,7. A 30% reduction in these common problems in the morbidly obese is observed for every 10% weight loss, which shows how beneficial bariatric surgery is6.
However, after massive weight loss, patients present distortions in body contour due to excess skin and flaccidity2,7,8. Consequently, there are interferences in the quality of life, which cause damage to the movement, posture, suitability of clothes, and hygiene, which is usually associated with fungal infections and cases of recurrent dermatitis1,2,4,7,8. In addition, psychological problems arise, such as self-image disorders, and depression, among others1-4,8.
Faced with this situation, reconstructive plastic surgeries serve as an alternative to improve the results obtained by gastroplasty and are sought after by more than 70% of patients undergoing this type of intervention2,7. The procedures performed include different techniques, such as abdominoplasty, mammoplasty, flankoplasty, brachioplasty, cruroplasty, torsoplasty and rhytidoplasty2,3,6. Usually, the abdomen is the first to be operated on, as it is the most affected region8.
In order to obtain the best result for the postbariatric patient, it is necessary to carry out a meticulous evaluation before performing plastic surgery since there is an interference of nutritional disorders and other comorbidities3. In this context, it is recommended not to submit patients to body contouring procedures until weight loss is complete and remains stable for a certain time3.
Therefore, reconstructive surgeries should be performed in stages, avoiding large associations1,3,8. The complication rates are tolerable, occur in the immediate postoperative period and do not pose a risk to the patient’s life, with seroma and small dehiscence being the most frequent9,10.
OBJECTIVE
To describe the number of hospitalizations for bariatric surgeries and body contouring surgeries in postbariatric patients in Bahia.
METHODS
This is a cross-sectional observational study with aggregated Time Series data carried out from 2009 to 2019 in Bahia. Data collection was carried out on the Department of Informatics of the Ministry of Health (DATASUS) website, particularly through the Hospital Information System (SIH).
Cases of admissions for bariatric surgeries and postbariatric body contouring surgeries were included in the study, thus identifying the most frequent type of plastic surgery. In addition, the average length of stay of postbariatric patients hospitalized for body contouring surgeries and the total amounts spent per patient in gastroplasty with intestinal bypass and abdominal dermolipectomy were incorporated into this study.
The codes used were Authorization for Hospital Admission (AIH): vertical band gastroplasty (0407010181), gastroplasty with intestinal bypass (0407010173), gastrectomy with or without intestinal diversion (0407010122), abdominal dermolipectomy after bariatric surgery (0413040054), Crural dermolipectomy after bariatric surgery (0413040070), postbariatric surgery brachial dermolipectomy (0413040062), postbariatric surgery mammoplasty (0413040089). Unprocessed cases in Bahia and those registered before the year 2009 or after the year 2019 were excluded from this work.
About the indicators used, this work consisted of the presentation of the data found that were tabulated through the Microsoft Excel 2010 software for descriptive statistical analysis.
According to Resolution 510/2016, this study did not need to be submitted to the Research Ethics Committee (CEP) system since the information used is in the public domain, of the aggregated type, without the possibility of individual identification.
RESULTS
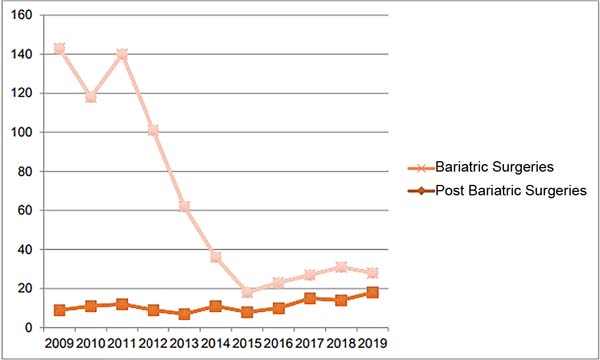
We identified 124 patients hospitalized for postbariatric surgery between 2009 and 2019 (Table 1). Among these results, abdominal dermolipectomy had the highest record, 64 hospitalizations (Table 2), representing about 52% of the total value; crural dermolipectomy had the second-highest record, 25 hospitalizations, about 20% of the total value. On the other hand, 603 admissions for bariatric surgery were recorded in this period (Figure 1), which allows us to consider that postbariatric surgeries combined represented 20.56% of total gastroplasty.
| Year | Bariatric surgeries | Postbariatric surgeries |
|---|---|---|
| 2009 | 134 | 9 |
| 2010 | 107 | 11 |
| 2011 | 128 | 12 |
| 2012 | 92 | 9 |
| 2013 | 55 | 7 |
| 2014 | 25 | 11 |
| 2015 | 10 | 8 |
| 2016 | 13 | 10 |
| 2017 | 12 | 15 |
| 2018 | 17 | 14 |
| 2019 | 10 | 18 |
| Total | 603 | 124 |
Source: DATASUS.
| Year | Abdominal dermolipectomy | Brachial dermolipectomy | Crural dermolipectomy | Mammoplasty | Total |
|---|---|---|---|---|---|
| 2009 | 7 | 1 | 0 | 1 | 9 |
| 2010 | 6 | 1 | 3 | 1 | 11 |
| 2011 | 6 | 3 | 3 | 0 | 12 |
| 2012 | 2 | 2 | 2 | 3 | 9 |
| 2013 | 3 | 1 | 1 | 2 | 7 |
| 2014 | 7 | 3 | 1 | 0 | 11 |
| 2015 | 3 | 2 | 3 | 0 | 8 |
| 2016 | 6 | 0 | 2 | 2 | 10 |
| 2017 | 6 | 4 | 5 | 0 | 15 |
| 2018 | 10 | 1 | 0 | 3 | 14 |
| 2019 | 8 | 4 | 5 | 1 | 18 |
| Total | 64 | 22 | 25 | 13 | 124 |
Source: DATASUS.
When the percentage of each surgery is evaluated, the number of abdominal dermolipectomy represented 10.61% of the total number of gastroplasty, while the crural dermolipectomy corresponded to 4.14%, these being the most frequent plastic surgeries for obesity. In addition, the average length of stay in this period of each surgery was identified (Table 3), in which abdominal dermolipectomy recorded the longest average length of hospital stay (2.8 days), while mammoplasty had the lowest rate (1.31 days).
| Year | Abdominal dermolipectomy | Brachial dermolipectomy | Crural dermolipectomy | Mammoplasty |
|---|---|---|---|---|
| 2009 | 3.7 | 2 | 0 | 3 |
| 2010 | 4.2 | 2 | 3.7 | 2 |
| 2011 | 3.3 | 1.7 | 2 | 0 |
| 2012 | 2 | 2 | 2 | 2 |
| 2013 | 2 | 2 | 4 | 1.5 |
| 2014 | 2.6 | 2 | 2 | 0 |
| 2015 | 4 | 2.5 | 2.7 | 0 |
| 2016 | 2.5 | 0 | 2 | 2 |
| 2017 | 1.7 | 2.3 | 0 | 0 |
| 2018 | 2.6 | 2 | 2 | 2 |
| 2019 | 2.3 | 2.3 | 3.2 | 2 |
| Total Average | 2.80 | 1.89 | 2.14 | 1.31 |
Source: DATASUS.
The total amounts spent per patient in gastroplasty with intestinal bypass ranged from R$ 5,232.80 to R$ 6,474.57 (Table 4), with R$ 5,767.95 being the average calculated in this period. Concerning abdominal dermolipectomy, the total value ranged from R$ 865.32 to R$ 1,463.62, with an average value of R$ 973.30.
| Year | Gastroplasty with intestinal bypass | Abdominal dermolipectomy |
|---|---|---|
| 2009 | 5,294.46 | 875.34 |
| 2010 | 5,299.02 | 877.07 |
| 2011 | 5,251.67 | 873.69 |
| 2012 | 5,232.80 | 937.35 |
| 2013 | 5,886.33 | 870.35 |
| 2014 | 6,218.92 | 1,103.20 |
| 2015 | 6,399.32 | 1,463.62 |
| 2016 | 6,474.57 | 865.69 |
| 2017 | 5,862.83 | 869.02 |
| 2018 | 5,745.48 | 1,105.75 |
| 2019 | 5,782.13 | 865.32 |
| Average Total Amount |
5,767.95 | 973.30 |
Source: DATASUS.
There were no records on admissions for brachial dermolipectomy in 2016, crural dermolipectomy in 2009 and 2018, and mammoplasty in 2011, 2015 and 2017.
DISCUSSION
The data collected identified that the type of procedure most performed in postbariatric surgery in this federative unit corresponded to the expectations described in the literature6,11, since abdominal dermolipectomy represented approximately 52% of the literature the procedures in the period studied. However, there were obstacles in interpreting these results since the brachial dermolipectomy, crural dermolipectomy and mammoplasty surgeries revealed a lack of data in some years, demonstrating a possible lack of execution of these procedures.
From the total comparison between the hospitalizations of these different procedures, it was noticed that in Bahia, body contouring surgeries represent only 20% of the hospitalizations of the 603 bariatric surgeries identified. This data demonstrates the incompatibility of previous findings in the literature2, which suggest that 70% of patients undergoing gastroplasty seek body contouring surgeries to improve the results.
In this context, with the knowledge that the same patient can undergo other types of reconstructive surgeries, the percentage of abdominal dermolipectomy can be even lower, being represented by only 10%. Thus, considering that the same patient performs an average of three repairing procedures and based on a demand of up to 70%, the number of surgeries should be around 1,266 and not 124 as found in the study.
Although there has been an upward pattern in the number of body contouring surgeries in the last 5 years in Bahia, the results are still not promising, especially when compared to gastroplasty. When analyzing the total amounts spent per patient in these two types of surgeries, there is a possibility that there is low availability of health establishments to perform these procedures since the number of vacancies for the performance of professionals is reduced.
The average total value per patient in gastroplasty with intestinal bypass is R$ 5,767.95, related to an average surgical time of 229 minutes; in an hour of procedure, the amount involved is approximately R$ 1,511.2512. In abdominal dermolipectomy, relating the average total value per patient (R$ 973.30) with the surgical time (240 minutes), in one hour, the amount involved is R$ 243.32, which only corresponds to about 16% of the cost of one hour of gastroplasty2.
From these data, it is possible to verify that even though body contouring surgeries promote significant changes in postbariatric patients’ quality of life, health institutions have lower revenue. The consequence of this is the existence of possible interference in the reduced number of procedures in Bahia and the need for the private sector to act as a supplementary agent.
On the other hand, a decline in hospitalization cases for bariatric surgery was observed over time in the Unified Health System (SUS) of Bahia, which shows a certain inconsistency since the number of obese people in Brazil continues to increase their main interventional treatment presents a decline2. Given the findings, the possibility arises of a lack of access by patients to these services in this federative unit.
This idea is reinforced when the discrepancy concerning other country regions is perceived. While the South Region had a 505% increase in bariatric surgeries between 2008 and 2018, the Northeast Region reduced the number of procedures performed13. In the same context, this study found a drop from 134 gastroplasty procedures to 10, which corresponds to a reduction of about 92%. On the other hand, even in lower-cost procedures, such as reconstructive surgeries, a similar difficulty was identified since it was evidenced that patients in the state of Bahia had an average waiting period of 8 to 10 years to perform them11.
Therefore, a question is raised about the cause of this lack of assistance in these surgeries relevant to the treatment of obesity, whether due to high demand, a scarcity of specialized local services, a low financial return for health facilities, or all these possibilities together.
Regarding the average length of stay of hospitalizations for body contouring surgeries, abdominal dermolipectomy is highlighted again for demonstrating the highest total average. Since prolonged hospitalizations increase the risk of infections and thrombosis, since this type of surgery is the one that causes the most complications, and the postbariatric patient already has a high susceptibility to postoperative complications, these findings guarantee its importance and impact on the prognosis3,14,15.
However, from 2016 onwards, there was a decrease in the average length of stay for this procedure, with the highest value represented by 2.6 days. This demonstrates that there has been an effective mobilization to reduce hospitalization time over the years. However, the change was not enough, and there is still a need for improvement since it is proposed in the literature that the average length of stay is around two days1,6,7. Therefore, in this federative unit, abdominal dermolipectomy appears to lack the inclusion of new techniques to promote a greater reduction in the average length of hospital stay.
Therefore, it is possible that, given the epidemic of obesity, the state of Bahia shows a generalized reduction in the assistance of surgical treatment services that involve weight loss.
CONCLUSION
Between 2009 and 2019, 124 hospitalizations for body contouring surgeries were identified in Bahia, while the number of bariatric surgeries was 603, approximately five times greater than the number of plastic surgeries involving the treatment of obesity.
REFERENCES
1. Rosa SC, Macedo JLS, Freitas FG, Ferreira JLD, Canedo LR, Casulari LA. Abdominoplastia em pacientes pós-bariátricos: perfil antropométrico, comorbidades e complicações. Rev Bras Cir Plást. 2018;33(3):333-42.
2. Daher JC, Campos AC, Cammarota MC, Peixoto BE, Dos-Santos GC, Barcelos LDP, et al. Cirurgia pós-bariátrica: seis cirurgias em dois tempos. Rev Bras Cir Plást. 2019;34(2):218-27.
3. Herman CK, Hoschander AS, Wong A. Post-Bariatric Body Contouring. Aesthet Surg J. 2015;35(6):672-87.
4. Toma T, Harling L, Athanasiou T, Darzi A, Ashrafian H. Does Body Contouring After Bariatric Weight Loss Enhance Quality of Life? A Systematic Review of QOL Studies. Obes Surg. 2018;28(10):3333-41.
5. Meira AAM, Andrade IF, Ferreira FPM. Cirurgia Plástica Após Gastroplastia Redutora: Abordagem Pré, Per e Pós-operatória. Rev Bras Cir Plást. 2008;23(1):15-21.
6. Kaluf R, Azevêdo FN, Rodrigues LO. Sistemática Cirúrgica em Pacientes Ex-Obesos. Rev Bras Cir Plást. 2006;21(3):166-74.
7. Holanda EF, Pessoa SGP. Cirurgia plástica de contorno corporal pós-bariátrica: revisão de literatura. Rev Bras Cir Plást. 2018;33(Suppl.2):16-8.
8. Gerk PO. Cirurgia do contorno corporal após grandes perdas ponderais. Rev Bras Cir Plást. 2007;22(3):143-52.
9. García Botero A, García Wenninger M, Fernández Loaiza D. Complications After Body Contouring Surgery in Postbariatric Patients. Ann Plast Surg. 2017;79(3):293-7.
10. Grieco M, Grignaffini E, Simonacci F, Raposio E. Analysis of complications in postbariatric abdominoplasty: Our experience. Plast Surg Int. 2015;2015:209173.
11. Silva CF, Felzemburgh VA, Rosa FP, Menezes JVL. Perfil dos pacientes submetidos à cirurgia plástica pós-bariátrica. Rev Ciênc Méd Biol. 2017;16(3):277-82.
12. Nguyen NT, Goldman CD, Ho HS, Gosselin RC, Singh A, Wolfe BM. Systemic stress response after laparoscopic and open gastric bypass. J Am Coll Surg. 2002;194(5):557-66.
13. Tonatto-Filho AJ, Gallotti FM, Chedid MF, Grezzana-Filho TJM, Garcia AMSV. Cirurgia bariátrica no sistema público de saúde brasileiro: o bom, o mau e o feio, ou um longo caminho a percorrer. Sinal amarelo! ABCD Arq Bras Cir Dig. 2019;32(4):e1470.
14. Silva RP, Pinto PIDP, Alencar AMC. Efeitos da hospitalização prolongada: o impacto da internação na vida paciente e seus cuidadores. Rev Saúde (Santa Maria). 2018;44(3):1-2.
15. Fraccalvieri M, Datta G, Bogetti P, Verna G, Pedrale R, Bocchiotti MA, et al. Abdominoplasty after weight loss in morbidly obese patients: a 4-year clinical experience. Obes Surg. 2007;17(10):1319-24.
1. Universidade Salvador, Salvador, BA, Brazil
2. Centro Universitário UniFTC, Curso de Medicina, Salvador, BA, Brazil
JCM Analysis and/or interpretation of data, Statistical analysis, Final approval of the manuscript, Acquisition of funding, Data collection, Conceptualization, Conception and design of the study, Resource Management, Project Management, Investigation, Methodology, Carrying out the operations and/or experiments, Writing - Preparation of the original, Writing - Review and Editing, Software, Supervision, Validation, Visualization.
ARS Analysis and/or interpretation of data, Statistical analysis, Final approval of the manuscript, Acquisition of funding, Data collection, Conceptualization, Conception and design of the study, Resource Management, Project Management, Investigation, Methodology, Carrying out the operations and/or experiments, Writing - Preparation of the original, Writing - Review and Editing, Software, Supervision, Validation, Visualization.
VAF Final Manuscript Approval, Project Management, Supervision.
Corresponding author: Juliana Correia de Matos, Av. Luís Viana, 3100-3146 - Pituaçu - Imbuí, Salvador, BA, Brazil, Zip Code: 41720-200, E-mail: julianacdematos@outlook.com
Article received: May 11, 2021.
Article accepted: July 14, 2021.
Conflicts of interest: none.







 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter