

Articles - Year 1997 - Volume 12 -
The Trapezoid Flap A New Technique for Nipple Reconstruction
Retalho Trapezóide Nova Técnica para Reconstrução da Papila
ABSTRACT
The author reports his experience witlr a newjlap for railoring a neo-nipple in breast reconstructions. Aseries of 50 cases with a four year post-operative follow-up is presented. The teclrnique is based on the foct that tire design of tire jlap is predaminalllly horizolllal with a 3: I ratio over the vertical size. The central 1/3 of the greater axis corresponds to tire dermal vascular pedicle, which ensures its greater viability. At closure, the trapezoidjlap determines a conical or cylindrical structure for the neo-nipple, depending on the design and hall' it is sutured. The main advantages oftlris jlap are tlrat tire donor site can be closed primarily by advancemelll and after fashioning, thejlap can be implanted on a dermal bed where thefuture areola will also be grafted. A vascular reinforcement is achieved through this procedure. This dermal platform serves to contain the neonipple. prevellling its collapse. When the jlap is closed margin to margin, a loss is observed in height of about 30% in six months. However, ifthe Slllure is made in a twisted manner, it is substantially reduced with a more significant and definitive result. Because ofthese observations, a hypercorrection compared 10 the opposite side is recommended. Up to the present, only two cases ofcomplete and one ofpartial necrosis have occurred, which corresponds to a complication rate of about 0.5%. It is indicated for all reconstructions, including for irradiated skins. The esthetic disadvantage ofa lighter colored skin can be eliminated by immediate grafting of skin like the neoareola or by pigmentation.
Keywords: Abdominal Flap, Breast Reconstruction, Tram-flap
RESUMO
O autor apresenta sua experiência pessoal, com uma nova forma de retalho para a confecção da neopapila nas reconstruções mamárias. A casuística apresentada consta de 50 casos, com observação por quatro anos de pós-operatório. O princípio da técnica baseia-se no fato de que o desenho do retalho tem a dimensão horizontal predominante sobre a vertical, na proporção de 3:1, sendo que o terço central do eixo maior corresponde ao pediculo vascular dérmico, garantindo maior viabilidade ao mesmo. A forma trapezóide do retalho determina ao final do fechamento uma estrutura cônica ou cilíndrica para a neopapila, dependendo da maneira como o desenhamos e como o suturamos. As principais vantagens desse retalho estão no fato de que a área doadora pode ser fechada primariamente por avanço, e o retalho depois de ser modelado pode ser implantado sobre um leito dérmico onde também será enxertada a futura aréola, constituindo-se, assim, num reforço vascular. Essa plataforma dérmica serve de contenção para a neopapila, impedindo seu desabamento. Quando o fechamento do retalho é feito borda a borda, observamos perda de altura de mais ou menos 30% em seis meses. Porém, se a sutura é feita em torsão, essa perda é bastante reduzida e o resultado mais significativo e definitivo. Por essas observações recomendamos seja feita uma hipercorreção em relação ao lado oposto. Até o momento, tivemos apenas dois casos de necrose total e um parcial, o que corresponde a aproximadamente 0,5% de complicações. As indicações se estendem a todas as formas de reconstruções, incluindo as peles que tenham sido irradiadas. A desvantagem estética é que a pele de cor mais clara pode ser perfeitamente eliminada através da enxertia imediata de pele igual à da neo-aréola ou da pigmentação.
Palavras-chave: Papila, Mama, Complexo Aréolo-papilar, Reconstrução Mamária
For some decades, numerous authors have been publishing various reconstruction techniques for the areola-papillary complex, ranging from the first report by Berson(1), followed by Adams(2) and Dufourmentel(3).
The possibilities of using the contralateral complex were well reported by Millard(8), after observations of the case demonstrated by Kiskadden(4), in 1950. This involved the successful transplant of the complex in a case of an arm burn. Tattoos were introduced by Epstein in 1956(5). The idea of the horizontal division of the nipple by Millard was used in the sagital forn1 by Pitanguy(11). The study of the skin tonalities introduced by Broadbent in 1977(14) practically defined the choice of technique for the areola by grafting the root of the thigh in most patients. However, this did not occur with the nipple, where a vast variety of flaps is describcd. Many flap shapes arc dcscribcd in thc literature, such as semilunar, cartilaginous, rhomboid, quadrangular. in omega, finger grafts, vertical with upper or inferior pcdicle, of the latissimus dorsi. in "T", in "S" and many others(3,7,12-20). These descriptions are interesting because the flaps are basically vertical or grafted or folded over themselves with dermal or subcutaneous pedicle. These principles usually determine that the blood supply in the flaps is a greater risk and, therefore, resulting in marked reduction of volume as time goes by. Consequently.
an attempt was made to modi fy this vascular principle, by designing a shape which would bring a greater volume of well nourished skin; the trapezoid shape provided the use of this principle with safety.
Material and Methods
AII the patients in whom this technique was uti Iized were postmasteetomy with breast rcconstructions by myocutaneous flaps of the rectus abdominus, or expanders or by lateral thoraeoepigastrie flaps. This means that the trapezoid flap was also utilized in cases of prothesis directly under the skin. The minimum time in which the trapezoid flap was used was three months a fter the first stage breast reconstruction. The new nipple is marked as symmetrically as possible to the opposite side, preferably before the surgery, with the patient seated or semi-scatcd. We should not bc bound by rigid markings such as the external furcula or the clavicular midline or the mideorporalline. The reason is that there is no uniformity in the performance of the mastectomies and consequently. in the results of reconstructions.
Thesc mcasurcments often result in errors. From all esthetic and sum metrical point of vicw. the best parameter is purely visual. Aftcr determining the point ofthe nco-nipple we need not be concerncd with designing the arcola at this time. This point corresponds to the base of the pedicle from which we will construct our trapezoid design (Figs. I and 2). The entire structure of the trapezoid is based on a measurement termed "x" and which most of the time is close to Icm. The base is 3x, the height is a minimum of Ix and it is always determined by bidigital gra p of the amount of skin that can be used, varying from one subject to another. The other side of the trapezoid is 2x.
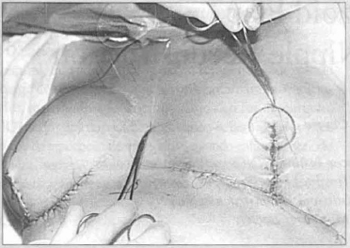
Fig. 1 - Design of tire exacr site for the neo-nipple compared to fire contralateral one.
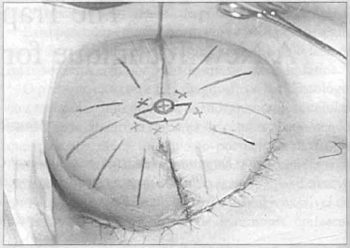
Fig. 2 - Central nipple circumferellce olld trapezoid ourlined around if. Design of tire various axes possible, evading possible scars.
This designs can be made using any directional axis of the new breast, i.e., the trapezoid can be vertical, horizontal. or oblique, with the pedicle in any position. This represents a big advantage, for often there arc scars which cross the new breast and therefore, the design can be adapted according to the situation, without impairing the flap's viability (Fig.3).
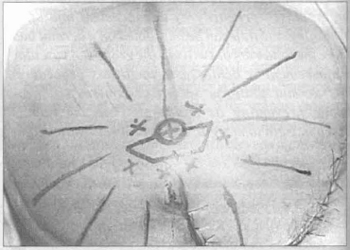
Fig. 3 - Design of the trapezoid; three portions in lire base and two on the opposite side, all of the same size.
It is a dermal-adipose flap, but in relation to the pedicle, the central portion should contain more fat than the sides for better shaping and simplification of closure (Fig. 4).

fig. 4 - Derma1-fat incision sparing the central zone of the pedicle.
Closure may be accomplished in either or two ways: by direct approximation of thc margins resulting in a final conical shape, or by approximation by twisting. In the latter, one of the edges is sutured to the base of the other and the remainder adapted naturally margin to margin (Figs.5 and 6).
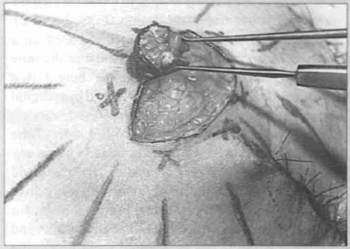
Fig. 5 - Intubation of the liberated flap as described in the text.
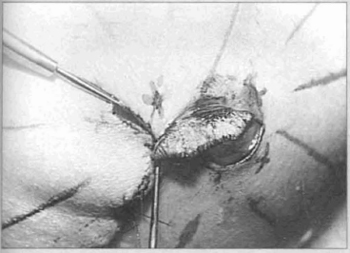
Fig. 6 - Advancement of the margins ofthe donor sire. forming a platform which will support the flap, after decortication to receive neo-areola.
The latter result is a cylindrical form. In both cases a good amount offat remains in the intcrior. The upper portion of the neo-nipple (the roof) should remain open without sutures, resulting in slight invagination by secondary epithelization. Thc donor site is easily closed by direct subdemlal approximation.
It is only at this point that the nco-arcola is marked and it is decorticated around the nco-nipple. The former will be supported on this demlial platform, taking care not to strangle the pedicle. All sutures are accomplished with 5-0 nylon (Fig. 7).
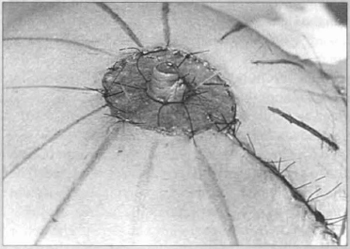
Fig. 7 - Already formed nipple and grafted areola taken from the root of the thigh.
Both the dermal bed and the trapezoid are grafted with skin from the root of the thigh. This graft should be completely independent, with separate sutures so that retraction will occur in different directions. Whcn the trapezoid is grafted, in order to obtain a darker tone, it should be decorticated while still attached to its original bed.
Contrarily, it can be pigmented later (Figs. 8 and 9).

Fig. 8 - Result 15 days p.o.

Fig. 9 - Preoperative aspect.
Discussion
Several techniques arc available for fashioning the nco-nipple. The main ones arc those that usc the opposite side, the dermal-fat grafts with vertical pedicle and superior or inferior base, and the triangular or quadrangular flaps with fatty central pedicle. Up to the present time, in our experience, the most esthetic and definitive results were obtained with the opposite nipple. However, because it is a composite graft, superficial losses are more common and frequently, the opposite nipple does not have enough projection to be used as a donor site. The single demlal pedicle flaps grafted, demonstrate some problems concerning both their structure and the donor site. They are flaps whose vertical dimension predominates leading to circulatory impairment, for they are outlined within another flap. This is confirmed by the absorption they undergo over time in the same way that the rate of graft loss is more common. It was also noted that these flaps shorten and undergo caudal or cephalic deviations because of retraction, depending on the pedicle used. It is often impossible to close the donor site directly, which results in the areolar graft over the fat, obviously making integration difficult. The Morton-Berson type flaps with central pedicle in the fat, with closure for elevation of the central cone, are the most problematic. These flaps frequently become ischemic and are lost. And those that initially progress well, undergo much reabsorption, leading to insufficient projection. The graft for the areola falls even more on a fat bet interspersed with small dermal bands, with a good deal of unevenness.
These technique are even more impaired if the new breast has scars close to the projection of the neonipple.
In order to avoid these scars, the neo-nipple becomes decentralized.
The easily fashioned trapezoid flap can always be placed in the central position ofthe new breast perfectly symmetrical with the opposite site, since its horizontal axis predominates, there will be various possibilities of avoiding the prior scars and by this, protecting the pedicle and its circulation. The donor site may be closed in all cases because the predominance of the flap's horizontal axis (3:1) ensures this feature, plus the fact that the edges of the flap are acute angles permitting easier closure. Although the flap circulation was impaired in three cases (we believe caused by technical error), up to the present, we have observed in almost all the cases obvious bleeding throughout the margin. We believe that because it is supported on a well-vascularized platform, this confers a second source of vascularization over the long teml, which must be one ofthe reasons for its satisfactory anatomic maintenance. This dermal platform also prevents its sinking by preserving its support. Since in most patients the normal nipple is not more than I em, this height and even more is easily achieved by the trapezoid flap.

Fig. 10 - Thirty days p.o.

Fig. 11 - Thirty days p.o.
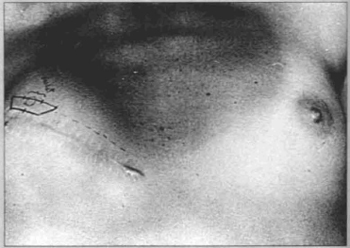
Fig. 12 - Application of trapezoid flap in the event of prosthesis implantation.
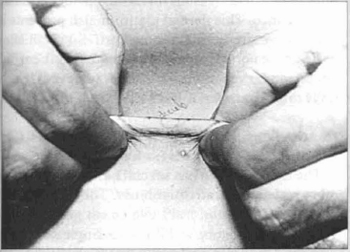
Fig. 13 - Bidigital pinch to evaluate skin elasticity.
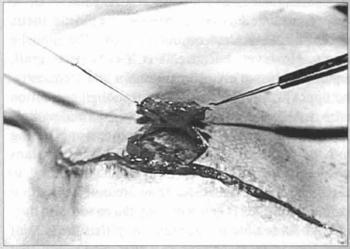
Fig. 14 - Raising of the flap, escaping the mastectomy scar.
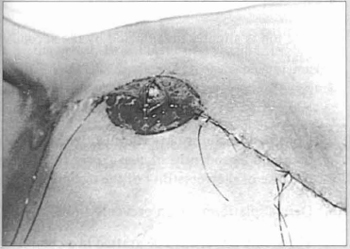
Fig. 15 - Flap shaped into a nipple and on the dermal platform.
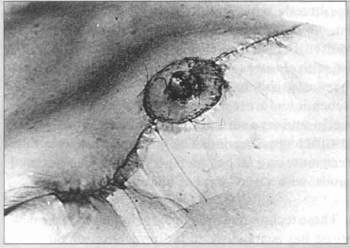
Fig. 16 - Graft already placed in the bed for the new areola and nipple.
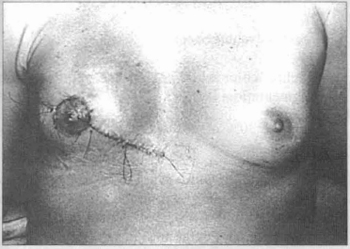
Fig. 17 - Immediate p.o. result.
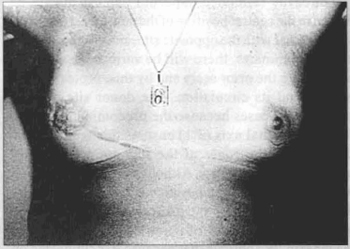
Fig. 18 - Results at three year fallow-up.
Conclusion
The trapezoid flap has several advantages over the other techniques currently in use. They include:
1. Great circulatory viability in a single pedicle, in which the horizontal axis is three times the vertical one, establishing a more favorable proportion in the midst of fibrosis. It is of lower risk;
2. Final shape conical or cylindrical;
3. The top is slightly invaginated by the secondary scar;
4. A secondary pedicle originating In the dermal bed;
5. Constant possibility of centralization in the new breast independently of the existence of scars, because of the versatility of the design;
6. Dermal platform which prevents sinking;
7. The areola can always be grafted in a completely dermal bed without fat, due 0 the closure of the donor area;
8. A small loss of the initial shape is acceptable.
The disadvantages are:
1. Lighter color when not grafted, reqUiring later pigmentation;
2. Loss of 30% of its volume when closed in the cone-shape;
3. The possibility of the scar left in the donor site of the flap extending beyond the limits of the neoareola graft, but even so, it has not been the subject of complaint until now;
4. Small axis deviations of the neo-nipple due to inadequate fixation and scar retraction.
References
1. BERSON NL. Construction of pseudoareola. Surgery 20: 808, 1946.
2. ADAMS WM. Labial transplant for correction of loss of the nipple. Plast Reconstr Surg 4: 295, 1949.
3. DUFOURMENTEL L. Chirurgie reparatrice et eorrectrice des teguments et des formes. Massons et Cie. Paris, 1950.
4. KISKADDEN WS (1950). Case report on split grafting the nipple. Plast and Reconstructive Surgery, 5, 184.
5. EPSTEIN E. Therapeutic tattoing. In Skin Surgery. Philadelphia. Lea & Febiger, 1956.
6. DiPI RRO E. Reconstruction ofthe nipple and arcola after a bum. Plast and Reconstructive Surg 46: 229, 1970.
7. HOLDSWORTH WG. A method of reconstructing the breast. Br J Plast Surg 9: 1961, 1956.
8. MILLARD DR. Nipple and arcola reconstruction by split-skin graft from the normal side. Plast and Reconstruct Surg. 50: 350, 1972.
9. WEXLER MR and O'NEAL RM. Arcola sharing to reconstruct the abscnt nipple. Plast and Reconstruct Surg. 51: 176, 1973.
10. BU CHMAN HH, LARSO DL, HUANG TT et al. Nipple reconstruction in bum breast. The double bubble technique.Plast and Reconstruct Surg 54: 531, 1974.
11. PITANGUY J. Reconstruction of the arcola and the nipple. Rev Bras Cirurg. 65: 237-244, 1975.
12. MURUCI A, DANTAS JJ, NOGUEIRA LR. Reconstruction of the nipple arcola complex. Plast Reconstr Surg. 61 :558. 1978.
13. BRENT B and BOSTWICK J. ipple arcola reconstruction with auricular tissues. Plast and Reconstruct Surg 60: 353, 1977.
14. BROADBENT TR, WOOLF RM., and MHZ PS. Restoring the mamary arcola by skin graft from the upper inner thigh. Br. J. Plast. Surg. 30: 220, 1977.
15. BARTON FE. Latissimus dermal-epidemlalnipple reconstruction. Plast and Reconstruct Surg. 70: 234, 1982.
16. LITTLE IN 1II, MUNASIFI T, McCULLOCH DT. One stage reconstruction ofa projecting nipple: The quadropod nap. Plast and Reconstr Surg 71: 126, 1983.
17. BOSCH G and RAMIREZ M. Reconstruction ofthe nipple. Plast and Reconstruct Surg. 73: 977, 1984.
I - Plastic Surgeon and Mastologist, National Cancer Institllle (INCa) - Rio de Janeiro, Brazil Plastic Surgeon and Mastologist, "Hospirallsraelita Albert Sabin" Member ofBrazilian Society ofPlastic and Reconstructive Surgery Member of Brazilian Mastology Society
ADDRESS FOR CORRESPONDENCE
Mauricio Chveid
Pra,a da Cruz Vennelha, 23 Centro
Rio de Janeiro - Brazil CEP.: 20230-130
From the Plastic and Reconstructive Surgery Service (INCa) - Rio de Janeiro, Brazil


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter