

Special Article - Year 2022 - Volume 37 -
Evolution of mammary prostheses and the incision methods used in adhesive mamoplasty procedures
A evolução das próteses mamárias e os métodos de incisão utilizados em procedimentos de mamoplastia de aumento
ABSTRACT
The study aims to analyze articles already published in breast augmentation, to analyze the various procedural techniques used for the placement of breast prostheses, highlighting their disadvantages and advantages, types and evolution of prostheses. The choice of prosthesis and the type of Surgical incisions are very important decisions that must be taken together (doctor and patient), taking into account the advantages and disadvantages of each incision. A good clinical preoperative explanation is essential to determine the goals to be achieved, thus avoiding possible repair surgeries or replacement of the size of the prosthesis. The enhancement of external beauty has gained more and more space, proof of which is the increasingly crowded plastic surgeons' offices. The USA is the champion country in plastic surgery, followed by Brazil. Augmentation mammoplasty is the second most performed surgery worldwide, second only to liposuction. People seek this method as an alternative to improve self-esteem or to try to fit into a "fictitious" beauty standard established by society. The present work has a study methodology of the narrative bibliographic review type. The instrument used was a literature review and a comparative method between articles published in plastic surgery, focusing on breast augmentation based on the inductive method. The study was based on international and national articles, using SciELO and The Lancet as research sources.
Keywords: Mammaplasty; Prostheses and implants; Reconstructive surgical procedures; Breast; Surgical wound; Reoperation.
RESUMO
O estudo desenvolvido tem como objetivo analisar artigos já publicados na área da mamoplastia de aumento, analisar as diversas técnicas de procedimentos utilizadas para colocação de próteses de mama, ressaltando suasincisão cirúrgica são decisões muito importantes que devem ser tomadas em conjunto (médico paciente), levando em consideração as vantagens e desvantagens de cada incisão. É indispensável um bom esclarecimento pré-operatório clínico que permita objetivar as metas a serem alcançadas, evitando, assim, possíveis cirurgias de reparo ou troca do tamanho da prótese. O enaltecimento da beleza exterior tem ganhado cada vez mais espaço, prova disso são consultórios dos cirurgiões plásticos cada vez mais cheios. Os EUA é o país campeão em cirurgias plásticas, e logo em seguida vem o Brasil. A mamoplastia de aumento é a segunda cirurgia mais realizada mundialmente, perdendo apenas para a lipoaspiração. Pessoas buscam esse método como alternativa para melhorar a autoestima, ou para tentar se inserir em um padrão de beleza "fictício" estabelecido pela sociedade. O presente trabalho conta com uma metodologia de estudo do tipo revisão bibliográfica narrativa. O instrumento utilizado foi revisão de literatura e método comparativo entre artigos já publicados na área da cirurgia plástica com foco em mamoplastia de aumento baseado no método indutivo. O estudo foi fundamentado em artigos internacionais e nacionais, usando como fonte de pesquisa a SciELO e The Lancet.
Palavras-chave: Mamoplastia; Próteses e implantes; Procedimentos cirúrgicos reconstrutivos; Mama; Ferida cirúrgica; Reoperação
INTRODUCTION
The cult of beauty and the search for perfect harmony with the body has increased the number of patients in medical offices looking for a plastic surgeon to achieve the expected goal. Studies show that in the last 25 years, one of the plastic surgeries that grew the most in Brazil (second only to the USA) and the world was the surgery to include breast implants since the breasts represent the organ of femininity. In Mexico, aesthetic and reconstructive plastic surgery ranked first in 2012 and 20131,2.
The average is two million women who opt for breast augmentation surgery in the US. Most prefer more natural prostheses, but some prefer saline ones; this number is still not higher. Some women claim prostheses may have some disadvantages, such as contractures silicone migration causing systemic conditions such as lupus fibromyalgia and, in some cases, the need for reoperation. However, it is known that studies have been developed to increase the safety of prostheses3.
Plastic surgery can be both reconstructive and aesthetic, including surgical and non-surgical procedures to reshape normal body structures to improve the patient’s appearance and self-esteem. Some factors contribute to the search for breast augmentation, such as age, genetics, pregnancy, changes in weight, dissatisfaction with the size of the breasts, among others4.
Breast implant surgeries began to appear around 1962. Medical science lives in constant discovery; every moment, a new method, a new cure, a new diagnosis comes to the fore. In medical aesthetics, it is no different. Along with the emergence of plastic surgery, several challenges and techniques were emerging, such as the high rates of capsular contracture and rupture, partially improved with textured and polyurethane coatings5.
According to data from the International Society of Aesthetic Plastic Surgeons (ISAPS), in 2011, 905,124 aesthetic surgical procedures were performed, with liposuction (removal of localized fat) being one of the most sought after, occupying the first place in the ranking, followed by augmentation mammoplasty (insertion of a prosthesis for breast augmentation), which appears in second place, and in third place comes abdominoplasty (removal of excess fat and flaccidity from the abdomen). One study reported that, in 2011, 211,108 liposuction surgeries, 148,962 mammoplasty surgeries and 95,004 abdominoplasty surgeries were performed4 (Table 1).
| Types of surgeries | Amount | % |
|---|---|---|
| Liposuction | 211.108 | 46 |
| Mammoplasty | 148.962 | 33 |
| tummy tuck | 95.004 | 21 |
| TOTAL | 455.074 | 100 |
Source: Veloso et al.4
The high rates of registered surgical procedures reflect the dissatisfaction with the image and the consequent search for perfection, which many people seek because they want to fit into the “fictitious” world of beauty imposed by the media, bringing numerous consequences, including psychological ones, such as anxiety, depression and low self-esteem due to this dissatisfaction with the body.
OBJECTIVE
The objective is to report the evolution of silicone breast implants’ existing types and compare the incision methods for their placement.
METHODS
The present study presents a study methodology of the narrative bibliographic review type, in which comparisons were made between scientific articles focused on the area of plastic surgery with a focus on augmentation mammoplasty, not requiring submission to the Research Ethics Committee (CEP), since that the study did not involve humans.
Development
The study aims to evaluate various procedural techniques used for the placement of breast prostheses, highlighting their advantages and disadvantages, their evolution and the types of existing prostheses. The topic addressed by this article is of great importance for the population, as it will be an enlightening source for many doubts of people who fear having surgery or those who do not feel comfortable asking the doctor. It can also help choose which procedure and the type and profile of prostheses to choose.
Dissatisfaction with appearance, defensive attitude and affective sensitivity are the reasons cited by Sante (2008) in the search for a body and facial modification. Aquino (2009, p. 10), referring to the concept of aesthetic plastic surgery, emphasizes that the intervention “responds to the immediacy of modernity, bringing short-term results.” The human body and the search for beauty and perfection have become a physical, economic, symbolic and social capital and the desired lifestyle. After all, healthy people who undergo surgery are looking to change their way of life, and often making this decision is related to self-esteem and self-confidence4.
In most cases, the silicone implant is placed on top of the muscle under the mammary gland. In very thin patients, breast reconstruction or patients who do not have a breast (breast agenesis), the prosthesis must be placed under the muscle. The prosthesis insertion can be done through the axillary route, through the areola or through the inframammary fold (the breast fold), which is the most common location4.
Phases of prostheses
1st phase: Thick denture wraps with Dacron patch.
The first prostheses that appeared were composed of a thick wrapping with a Dacron patch that presented unnatural results, and they began to present some complications, such as foreign body-type inflammatory reactions and their inevitable consequences1.
Due to the great problems arising from this type of prosthesis, the manufacturing companies then decided to modify the thickness of the envelope, making it very thin, which turned out to be the worst phase of advances in prostheses, as the thin coating would determine ruptures, in the long term, because the gel acts as a solvent for this coating1.
2nd phase: Thin wraps, no patch.
A thin, patchless wrap marked the second phase of the denture evolution. The big problem is that the silicone gel of the prosthesis over time will dissolve its own wrapping, making the coating thinner or even dissolving it completely, leaving the viscous product inside the organic fibrous capsule, causing, in certain cases, the migration of the gel to the gland and neighboring tissues, forming a granule, more inflammation of the skin with skin rash, urticaria, chronic pain, calcifications, migration to the lymph nodes, migration to the path of peripheral nerves, or even infiltration of the chest simulating tumors, that even require exploratory thoracotomy. There are cases of patients with broken or dissolved prosthesis wraps who do not have any symptoms1.
3rd phase: Double lumen wraps.
Denture manufacturers realized that the evolution to thin-encased dentures was not as efficient as expected, so they continued to make progress by making double-lumen dentures (internally silicone gel with a second aqueous liquid wrap), but the new denture proved not to be practical., which resulted in a bad acquisition in the market, and they were soon withdrawn1.
4th phase: First inflatable prostheses.
With the failure of prostheses with double lumen wraps, the prostheses industries started to base their studies on inflatable prostheses, but they presented insecure valves and the manufacturers’ recommendation that such prostheses be filled with macromolecular solutions (dextran)1.
Inflatable prostheses also did not have good market acceptance since they presented an emptying caused by the poor quality of the valve (low safety level). As with any prosthesis, there is no impermeability barrier with the organic environment, the exchanges with both media developed, causing a significant increase in the number of organic capsular contractures1.
5th phase: Textured coating wraps.
The industries then began to develop prostheses with a coating layer with a greater capacity to resist the action of the gel in order to avoid the same problems caused in the previous phases. At this stage, the first textured prostheses began to appear, with traditional gelatinous filling and later with specific treatment of this gel (cohesive) and even other fillings that were not well accepted by surgeons from different parts of the world, such as castor oil, etc.1
6th phase: Wraps with polyurethane overlay.
Despite the advances already achieved by the industries, it was necessary to make the prostheses more resistant to avoid future complications, giving the consumer more security and protection to the body. As a result, studies began to seek a product capable of coating the silicone itself (which would be superimposed on the protective silicone cover) to minimize the effect of capsular contracture. The chosen product was polyurethane, which covers a large part of the prostheses on the market1.
7th phase: Inflatable saline prostheses.
The inflatable prostheses refused on the market in the 4th phase gained space again. However, the recommended filling became the saline solution this time, as it is isotonic instead of macromolecular solutions (dextran). Along with advances in textured and polyurethane prostheses, researchers have sought to invest in safer types of valves, aiming to win the market with inflatable prostheses1.
As mentioned before, the silicone coating of the inflatable prosthesis, like that of any other type of prosthesis, is not absolutely impermeable, and the phenomenon of bleeding (transudation of the prosthesis) may occur. This phenomenon is directly linked to two primary factors: intraprosthesis pressure and isotony of the fluid that fills it1.
The phenomenon of osmosis explains the need for the filling liquid to be isotonic, as there will be no hydroelectrolytic exchange between the two media. Another factor that contributes to the emptying of the inflatable prosthesis is the internal pressure caused by the excess of filling liquid; if there is an internal pressure greater than that of the environment in which the prosthesis is located, this hyperbaric environment will undoubtedly tend to seek equilibrium, causing the bleeding phenomenon. Then, the prosthesis will deflate1.
Incision methods used for breast augmentation
Different types of incisions can be performed in breast augmentation. The choice of method of implantation of the breast implant is of paramount importance, as it will depend on the desired volume, the anatomical conditions of the patient, skin characteristics, areola size, and the amount of breast and fatty tissue in the breasts, for example. Furthermore, it must be taken into account that each method has distinct advantages and disadvantages.
The main types of incisions performed for breast augmentation are the inframammary fold, the periareolar and the transaxillary. The choice of which incision will be performed in the procedure must consider the patient’s wishes and the surgeon’s technical analysis; the decision is taken together.
Incision in the inframammary fold
The inframammary fold incision is one of the methods most used by surgeons, as this type of incision generates very direct access to the breast region, allowing adequate visualization of the dissection area. This type of incision affects the breast tissue little, has the advantage of not altering the functioning of the breasts, not causing problems in future breastfeeding. The incision size must be enough to introduce the implant without tissue damage2,6.
The scar is located in the inframammary fold, leading to a discreet and disguised result in some cases and may leave hypertrophic scars (enlarged), however visible, which may be considered a disadvantage of this procedure.
The incision size varies according to the size of the silicone prosthesis chosen by the patient, reaching an average of 5. One of the advantages of this type of incision is the physician’s better visualization and direct access to the place to be implanted with the prosthesis and not affect the mammary gland and the areola7. It is carried out 1 cm above the furrow and has a 4-7 cm; this incision offers good results and leaves barely visible scars7.
This type of incision allows the patient and their doctor to choose whether to place the retroglandular implant (behind the mammary gland only or behind the fascia) or the retromuscular implant (behind the muscle). Each method has its advantages and disadvantages, and the decision must be made together with your surgeon6.
Periareolar incision
This technique is more common in women with small breasts and large areolas since this surgery allows the reduction of the same, which characterizes an advantage of this incision. In the periareolar approach, despite resulting in a well-disguised scar, the positioning of the implant is visible in the middle of the breast unit and has the advantage of good control of homeostasis and excellent access to the breast, which translates into postoperative fibrosis7,8.
The periareolar incision is performed in the lower area of the areola, located at the transition from the areolar tissue to the skin. Some disadvantages must be taken into account, such as damage to part of the mammary gland and lactiferous ducts, with possible harm to breastfeeding (the issue of implantation of breast implants and breastfeeding has been the subject of many studies, which many claims do not have any interference). In addition, the technique can only be used if the areola has a size that allows the introduction of the chosen implant7,9.
Another disadvantage is the risk of contamination by injury to the lactiferous ducts. This type of incision can also cause changes in the sensitivity of the areola and become visible if there is a different pigmentation in the region or if there is enlargement9.
Transaxillary incision
Axillary augmentation mammoplasty is not widely used. The technique was described in 1973 by Hoehler and received criticism regarding the poor visualization of the surgical field, particularly in the area close to the submammary crease, which translates into greater difficulty in symmetry and poor implant positioning. In addition to a greater risk of hematoma, it brings more complications to the patient, with a greater possibility of displacing the prosthesis and even risks of infections.
On the other hand, it has the advantages of inconspicuous scars located outside the aesthetic unit of the breast, and the non-violation of the mammary gland, keeping its unit unchanged. The scar is positioned in a natural fold in the axillary region and maintains the breast parenchyma and lactiferous ducts inviolate10.
The disadvantage of this incision is that it is more difficult to place prostheses with greater volume and position the implant in the breast. It also becomes difficult to reuse, requiring a new incision for cases where treatments are needed in place, or there is a replacement of the prosthesis. In this type of incision, asymmetry of the inframammary folds (and the base/lower region of the breasts)10 is more frequent.
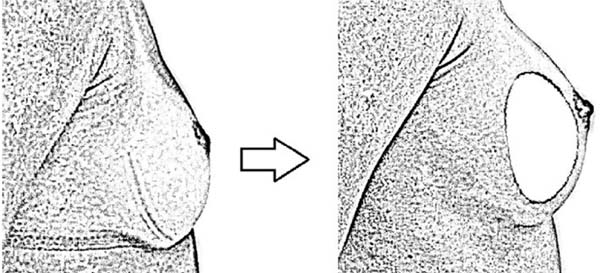
Types of breast implants: shapes and projections (Figure 1)
In 1993, numerous surgeons popularized anatomical implants, but very little literature compares the precise indications, advantages and disadvantages between round implants and anatomical implants11.
In the surgery for the inclusion of breast implants, one of the greatest difficulties is planning the volume adequate to the breast anatomy, biotype and patient’s wishes12.
A point as important as the choice of the prosthesis volume is the type of prosthesis that should be placed. Undoubtedly, before undergoing surgery, it is necessary to understand and learn to respect the biotype and understand that everyone has their own to achieve a harmonious and natural result12.
Many surgeons have their “formulas” or protocols regarding the choice of volume and type of implant, location, sulcus position and incision, widely published in the medical literature and used in clinical practice. The availability, by manufacturers, of implants with various shapes and projections allowed a range of options, but there are also additional factors that we must consider when planning an augmentation mammoplasty11,12.
The criteria for choosing volume, inclusion plane and incision site are based on pre-established concepts, the surgeon’s experience and the patient’s wishes11.
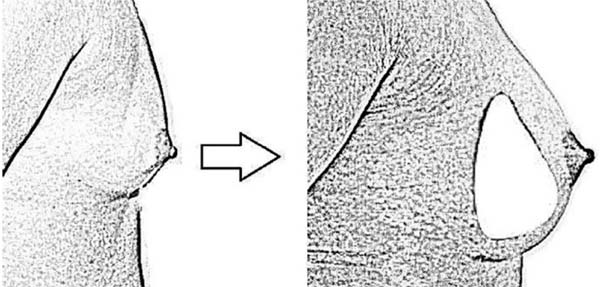
Round shape x anatomical shape implants
Round-shaped implants cause greater projection in the central portion of the breast, while the so-called anatomical implants produce greater projection in the lower pole of the breast. Based on the preoperative shape of the breast, surgeons propose an algorithm for choosing implants with a round shape or those with a lower projection (anatomical), according to the desired final shape (Figures 2 and 3)12.
The round prosthesis format is the most used since it has symmetry in all its dimensions, filling equally all the spaces of the breast, especially the breast neck, a normally empty region.
The fuller anatomical prosthesis shape in its central and lower part simulates the most natural shape of the female breast and is more suitable for thinner women, who do not want a very “marked” or “ball-like” result and for those who do not have the fallen breast. It is also widely used in breast reconstruction cases after breast cancer surgeries. This type of prosthesis fills the neck of the breast less than the round one and can further accentuate the drooping aspect of the breast. Therefore, it is more suitable for women with well-proportioned breasts and without any type of sagging12.
Another type of prosthesis is conical in shape, very suitable for patients with narrow chests and shoulders because it has the smallest width. It is an implant that projects the breast a lot without increasing the volume on the sides and without providing the artificial rounded appearance caused by the round prosthesis12.
This type of prosthesis also allows for a more natural shape, which has increasingly attracted the attention and choice of patients and surgeons. The conical prosthesis helps to leave the breasts with a less rounded shape and with the feeling of pert. As it focuses on projection, large volumes of the prosthesis are not needed to find the desired size. With conical prostheses, a good shape and projection of the breast neck is achieved, which is the result desired by many women12.
Round prostheses are distinguished by their projections or different profiles, which must be defined when choosing prostheses: “The difference in the profiles is in the projection of the prostheses (or how much they leave the breasts “further forward”), and in the width of the base of the prosthesis (how much it “spreads over the breast”). For the same volume, the higher the profile, the smaller the implant base and the greater its height”13.
With the choice of different profiles in terms of diameter/volume ratio, the patient and surgeon can first choose the desired implant volume and select the implant profile that best matches the patient’s base diameter. Dr. Flávio Borges highlighted the following characteristics for each type of round prosthesis profile13,14:
Round prosthesis with high profile: indicated for women with a proportional chest and little volume in the lap. High profile saline implants provide a useful option for those patients who desire an implant whose result exceeds the natural diameter of the breast base in standard profiles13.
Round prosthesis with super-high profile: indicated for women who have a narrow chest, the width of the prosthesis is narrower and has greater projection. Due to the preference for large breasts, these are the types of profile most used by women, as they allow larger volumes with less increase in the base, preventing the prosthesis from advancing to unwanted regions, that is, to the sides14.
Round prosthesis with low profile: the width is greater (diameter), and the projection (height) is smaller. It is indicated for patients with a broad chest or who want breast augmentation to the sides with a small projection in the front, which is not widely used today14.
RESULTS AND DISCUSSION
Undoubtedly, it is possible to perceive the great advance of the industries in the face of the evolution of breast implants, the search for compatibility with the tissue, the concern with not breaking them; however, something 100% safe has not been reached, which allows setbacks occur and possible reoperation is made15.
Augmentation mammoplasty, whether using the periareolar technique or the transaxillary technique, is a safe procedure with low morbidity and high satisfaction levels. The use of the technique via the transaxillary route does not add morbidity and can be an excellent alternative for patients who wish to undergo surgery but do not accept the idea of having a scar on their breasts3.
The content of modern prostheses is made up of cohesive silicone gel, which prevents leakage, maintaining the shape of the breast even in the event of a rupture. All these advances contribute to a more beautiful, natural and safer result13.
The implant filled with silicone gel is one of the most used, especially when breast reconstruction surgery is performed after mastectomy. Not much is known about the rate of implant rupture and its possible sequelae; studies prove through testing prosthesis materials that, as implants age in vivo, they weaken and may tend to rupture15.
Some sequelae of denture rupture include gel migration accompanied by inflammation and silicone granuloma formation. The issue of free silicone gel concerning idiopathic connective tissue disease is not well understood. Some routine exams can detect the rupture of the breast prosthesis, with magnetic resonance imaging being more visible when compared to mammography or ultrasound15.
The choice of type of incision to be made varies according to the patient (which can fit the profile for that type of incision chosen or not). What makes the patient think about this choice is the scar mark, and it is an important variable that the surgeon in the preoperative consultation should highlight. Some studies have shown that people opt for the inframammary incision in the USA and Brazil, while in China, the prevalence is due to the axillary scar, and the periareolar scar is more performed in patients with a large areola since it is possible to reduce it16.
A study carried out with 22 patients between 22 and 55 years old, with a mean age of 33 years, shows positive results9, giving good marks to the shape, symmetry and height of the breasts, scar quality, position, and position size of the areolas. These data were collected using a questionnaire.
CONCLUSION
The increase in plastic surgery is evident, and the advance in prostheses has contributed to this, as they provide greater safety for patients and have shown satisfactory results for the population.
Preoperative clinical clarifications that allow the objectives and goals to be achieved with the procedures to be analyzed are essential7.
Based on the researched articles, it was evident that plastic surgery is one of the most performed worldwide. Brazil is in second place in the ranking, behind the USA13.
The type of incision to be used varies according to the patient’s anatomy, based on the advantages and disadvantages (such as recovery time and scarring), and the healthcare professional’s opinion responsible for the surgery. Nevertheless, it is a decision made jointly by the doctor-patient12.
The prosthesis volume is also an important factor to be discussed in the office, as many women are dissatisfied with the breast volume achieved, leading to reoperation. The literature mentions that the number reaches 20% of patients, but when it is discussed before the operation, it has less morbidity for patients and avoids expenses, which in the US alone reached US$.5,770.0016.
REFERENCES
1. Sperli A, Bersou A Jr, Freitas JOG, Michalany N. Complicações com Próteses Mamárias. Rev Bras Cir Plást. 2000;15(3):33-46.
2. Vallarta-Rodríguez RA, Ruiz-Treviño JJ, Guerrero-Burgos F. Mamoplastia de aumento dinámica con control de vectores. Cir Plást Ibero-Latinoam. 2014;40(4):377-84.
3. Ault A. Silicone breast implants may be close to US approval. Lancet. 2003;362(9393):1384.
4. Veloso CN, Abbas K, Tonin JM da F. Cirurgia plástica: qual o custo da indústria da beleza? In: XX Congresso Brasileiro de Custos; 2013 Nov 18-20; Uberlândia, MG, Brasil [Acesso 2018 Set 29]. Disponível em: https://anaiscbc.emnuvens.com.br/anais/article/view/20
5. Montandon RE. Estudo de complicações em próteses mamárias: avaliação de 546 casos em oito anos. Rev Bras Cir Plást. 2014;29(3):352-60.
6. Valente DS, Carvalho LA, Ferreira MT. Avaliação da qualidade de cicatrizes em mamoplastia de aumento por via submamária e transareolomamilar: um estudo longitudinal prospectivo. Rev Bras Cir Plást. 2011;26(1):81-6.
7. Calderón JM, Carriquília C. Actualidad en mamoplastía de aumento. Horiz Méd. 2016;16(2):54-62.
8. Ferraz HP, Roxo ACW, Aboudib JH, Castro CC, Nahas F, Serra F. Mamoplastia de aumento: análise comparativa das técnicas periareolar e transaxilar. Rev Bras Cir Plást. 2012;27(3 Suppl 1):55.
9. Cardoso IF, Cardoso JB, Cardoso GF. Mastopexia periareolar (circum-areolar) com implante mamário cônico: tratamento de ptose, hipomastia e alterações de posição e tamanho do complexo aréolo-papilar. Rev Bras Cir Plást. 2014;29(3):368-74.
10. Roxo ACW. Análise comparativa entre as técnicas de mamoplastia de aumento transaxilar sem o uso de videoendoscopia e videoassistida. Rev Bras Cir Plást. 2013;28(3):348-54.
11. Cárdenas-Camarena L, Encinas-Brambila J. Round gel breast implants or anatomic gel breast implants: which is the best choice? Aesthetic Plast Surg. 2009 Sep;33(5):743-51.
12. Tavares-Filho JM, Franco D, Franco T. Implante mamário redondo versus anatômico: algoritmo para escolha da forma adequada. Rev Bras Cir Plást. 2015;30(3):413-22.
13. Baxter RA. Indications and practical applications for high-profile saline breast implants. Aesthet Surg J. 2004 Jan-Feb;24(1):24-7.
14. Fortes FB. Tipos de Próteses Mamárias: Tire suas dúvidas. In: Dr. Flávio Borges Fortes Cirurgia Plástica. Blog [Acesso 2018 Set 29]. Disponível em: http://clinicaborgesfortes.com.br/tipos-de-proteses-mamarias-esclareca-suas-duvidas/
15. Brown SL, Silverman BG, Berg WA. Rupture of silicone-gel breast implants: causes, sequelae, and diagnosis. Lancet. 1997 Nov 22;350(9090):1531-7.
16. Motta RDS, Roxo ACW, Nahas FX, Serra-Guimarães F. Comparação entre diferentes métodos de escolha de volume de implantes mamários e o grau de satisfação pós-operatório. Rev Col Bras Cir. 2018;45(1):e1345.
1. Guaçuí University, Human Anatomy, Itaperuna, RJ, Brazil.
| COLLABORATIONS | |
|---|---|
| LLM | Analysis and/or data interpretation, Conception and design study, Conceptualization, Methodology, Project Administration, Validation, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing |
| WM | Supervision, Visualization, Writing - Review & Editing |
| DGM | Conception and design study, Conceptualization, Final manuscript approval, Formal Analysis, Realization of operations and/or trials, Resources, Supervision, Validation, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing |
Corresponding author: Lays Lopes Monteiro, Rua, André Luis, 22, Jardim Carioca, Campos dos Goytacazes, RJ, Brazil, Zip Code 28080-720, E-mail: layslopesmonteiro@outlook.com
Article received: January 28, 2020.
Article accepted: October 15, 2021.
Conflicts of interest: none.









 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter