

Case Report - Year 2022 - Volume 37 -
Madelung's disease: combined surgical approach of lipectomy and liposuction
Doença de Madelung: abordagem cirúrgica combinada de lipectomia e lipoaspiração
ABSTRACT
Madelung's disease (MD) or Multiple Symmetric Lipomatosis is a condition characterized by the accumulation of unencapsulated adipose tissue deposited symmetrically around the neck and upper trunk (type I - most common form). Its etiology is still unclear, but it is clearly associated with chronic excessive consumption of alcoholic beverages. Physical deformities lead the patient to seek medical care, along with possible symptoms of cervical involvement such as reduced mobility and respiratory disorders. Multiple Symmetric Lipomatosis diagnosis is clinical and can be complemented with imaging to rule out other diagnostic hypotheses and assess the extent of involvement. Treatment can be performed in two ways: clinical or surgical (lipectomy or liposuction). We report the case of a patient with Multiple Symmetric Lipomatosis type I surgically treated with both techniques: cervical lipectomy and abdominal liposuction. The patient evolved satisfactorily, with a reduction in complaints and no recurrences so far.
Keywords: Multiple symmetric lipomatosis; lipomatosis; Lipoma; Reconstructive surgical procedures; Lipectomy.
RESUMO
A doença de Madelung ou lipomatose simétrica múltipla é uma patologia caracterizada pelo acúmulo de tecido adiposo não encapsulado e depositado simetricamente ao redor do pescoço e tronco superior (tipo I - forma mais comum). Sua etiologia ainda é pouco esclarecida, porém apresenta evidente associação com o consumo crônico excessivo de bebidas alcoólicas. As deformidades físicas são o que levam o paciente a buscar serviço médico, juntamente com eventuais sintomas de acometimento cervical como redução de mobilidade e afecções respiratórias. O diagnóstico da lipomatose simétrica múltipla é clínico, podendo ser complementado com exame de imagem para afastar demais hipóteses diagnósticas e avaliar a extensão do acometimento. O tratamento pode ser realizado por duas modalidades: clínico ou cirúrgico (lipectomia ou lipoaspiração). Relata-se o caso de paciente com lipomatose simétrica múltipla tipo I abordado cirurgicamente com ambas as técnicas: lipectomia cervical e lipoaspiração abdominal. Paciente evoluiu de maneira satisfatória, com redução de queixas e sem recidivas até o presente momento.
Palavras-chave: Lipomatose simétrica múltipla; Lipomatose; Lipoma; Cirurgia plástica Lipectomia; Alcoolismo
INTRODUCTION
Madelung’s disease or Multiple Symmetric Lipomatosis (MSL) is a rare disorder of adipocyte metabolism, characterized by the accumulation of non-encapsulated adipose tissue, located symmetrically in the facial region neck, shoulders, trunk, limbs and other areas1.
Otto Madelung described it in 1888, and, since then, there have been just over 280 reported cases of this disease in the literature. There is no fully clarified pathophysiology about it, but it seems associated with chronic excessive consumption of alcoholic beverages. A possible autosomal dominant inheritance with variable penetration of mitochondrial DNA has been discussed2.
In 1978, Carlsen and Thomsen classified benign lipomatosis into 3 distinct clinical groups, according to the fat accumulation site, as shown in Chart 13.
| Type 1 Congenital diffuse lipomatosis | Located principally in trunk, bad delimited from neighboring tissues, not hereditary. |
|---|---|
| Type 2 Symmetrical Diffuse Lipomatosis | Develops at life adult, firstly located in the cervical region, hereditary. |
| Type 3 Multiple Lipomatosis | Numerous small encapsulated subcutaneous lipomas, mainly located on the limbs. |
The classic clinical presentation of the disease is in adult men, alcoholics with comorbidities, who notice the appearance of symmetrical lipomatous lesions with slow and progressive growth. The vast majority of them decrease quality of life due to the aesthetic damage caused by adipose lesions3.
Computed tomography is the main method for diagnosis, preoperative staging and postoperative follow-up of patients. The tomographic characteristic of the disease is the distribution of non-encapsulated and homogeneous lipomatous tissue, with imprecise limits and without a cleavage plane with the adjacent subcutaneous tissue, and there may also be deep (submuscular) deposition of adipose tissue4. In some cases, calcifications within the lipomas can be identified.
Complications involved in Madelung’s disease result from compression of the cervical structures by fat deposition, which can cause dysphagia, odynophagia and hoarseness5. Death resulting from a direct complication of lipomas is quite uncommon; however, despite being rare, malignant degeneration of Madelung’s disease has already been reported in the literature6.
OBJECTIVE
The objective of this study is to report the case of a patient with MSL who was surgically treated by the combination of lipectomy and liposuction techniques and to discuss the choice of treatment and its effectiveness, in addition to analyzing the possibilities of clinical and surgical treatments available so far.
CASE REPORT
A 55-year-old male patient reported the appearance of painless expansive masses in various parts of the body about a year ago. The progressive growth of these masses triggered compressive complaints such as dyspnea, dysphagia and dysphonia, and abdominal pain and aesthetic deformity, with consequent social isolation.
Personal history: Patient with systemic arterial hypertension, a former smoker for 24 years/pack and former alcoholic of spirits (200 ml/day) for 35 years.
Surgical history: Lipoma excision in the right breast region three years ago.
The general physical examination showed no alterations, except for the symmetrical, non-delimitable and painless masses in the upper part of the body - anterior and posterior cervical, submental, supraclavicular, deltoid, thoracic, dorsal and abdominal regions (Figure 1) compatible with Madelung’s disease type I.
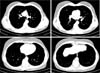
There were no significant changes in her laboratory tests. A computed tomography (CT) scan of the neck was performed (Figure 2), which showed prominence of adipose tissue in the cervical subcutaneous tissue, more pronounced in the submandibular, posterior cervicodorsal supraclavicular regions. Chest CT (Figure 3) showed prominence of adipose tissue in the subcutaneous tissue of the breast, anterior chest wall and dorsal region, including between the muscular planes, with a swelling effect. Abdominal CT showed prominence of adipose tissue in the abdominal subcutaneous tissue (Figure 4).
Once the diagnosis of Madelung’s disease with cervical and trunk involvement was established, surgical treatment was chosen together between the Head and Neck Surgery and Plastic Surgery teams from the Celso Pierro Hospital and Maternity, Campinas, SP, in two stages, combining the methods of cervical lipectomy and abdominal liposuction, taking into account the symptoms, extent of the lesions, physical deformity and the patient’s desire. According to the Helsinki principles, the patient signed the Free Informed Consent Form prior to the surgical procedures.
In the first surgical stage, performed by the Head and Neck Surgery team in September 2019, the patient underwent cervical lipectomy with the removal of three non-encapsulated fatty lesions (Figure 5), followed by primary closure of the single transverse cervicotomy. The anatomical pieces were sent for anatomopathological (AP). The AP report revealed histopathology consistent with lipoma.
In the second surgical time performed by the Plastic Surgery team, in February 2020, anterior abdominal liposuction was performed, with a wet technique, with the removal of 1700 milliliters of fat tissue, which was later discarded (Figure 6).
The patient evolved satisfactorily in the postoperative period, did not present surgical complications, attended follow-up appointments, and performed an evolutionary photographic record. She received non-pharmacological antithrombotic prophylaxis during the intraoperative and postoperative periods. In the postoperative follow-up, he was satisfied with the surgical results, with a significant improvement in appearance (Figure 7), improvement in his clinical complaints, and increased self-esteem. Nowadays, he has not had recurrences of lesions in the treated regions.
DISCUSSION
Madelung’s disease or Multiple Symmetric Lipomatosis is a rare disorder of adipocyte metabolism, predominantly in adult men aged 30 to 60 years. Its slow and progressive growth can determine social isolation and depression1. Compressive symptoms can arise in the cervical and thoracic territory, giving the patient a significant loss of quality of life.
After diagnosing this syndrome, a therapeutic plan must be drawn up to guarantee that patients relief from their symptoms and complaints, both physical and psychological. The treatment of these patients is palliative and may include clinical and surgical measures.
In addition to correcting the metabolic syndrome when present, drugs have demonstrated control over the growth of lesions. The use of beta-2-adrenergic agonists was described in work by Leung et al. from 1987. This work experimentally presented the use of oral Salbutamol as a drug to reverse rapidly progressive Madelung’s disease. The recommended regimen for therapy with Salbutamol consisted of the intake of 12 mg/day divided into three doses for six months7. However, few studies have proven its effectiveness, and its use is not routine in treating these patients.
Non-surgical techniques have been developed as an adjunct or substitute for surgery, such as lipolytic injection. This is performed by applying lipolytic actives, such as phosphatidylcholine and deoxycholate, causing fibrosis of the adipose tissue and improving the appearance of the disease8. However, its use generates severe adhesions in the treated region, which technically difficult liposuction or surgical excision in case of recurrence.
Surgical techniques such as adipose tissue resection and liposuction are widely reported in the literature. It is estimated that 63% of patients have a recurrence in the postoperative period of open surgery and 95% in the case of liposuction9.
The excision of lipomatous masses is complex, not only because of its extension but also because of the fibrous, hypervascular and infiltrative nature of this tissue10. As there is no cleavage plane between the lesions and normal adipose tissue, the total resection of the deposits becomes a major challenge for the surgeon. Despite rigorous hemostasis and use of drains in the postoperative period, the appearance of seromas and hematoma is relatively common11.
Liposuction has the advantage of presenting lower perioperative mortality than conventional surgery, being extremely important since patients commonly have multiple comorbidities12. Its execution presents technical difficulties, such as resistance to penetration of the cannula due to the fibrous nature of the tissue, profuse bleeding due to the tissue’s rich vascularization and the need for a cautious approach due to the intimate relationship of the tissue with vessels and nerves13. Thus, this technique must be performed by experienced hands and in large regions where open resection is unfeasible.
Constantinidis et al.14, in their 2003 study, used lipectomy and liposuction together to treat neck masses in 11 patients with Madelung’s disease. Lipectomy was performed first and liposuction second. During the 32-month postoperative follow-up, all patients showed functional improvement, and more than 80% of patients were satisfied with the esthetic result. Two relapses were observed in this study14.
Wollina et al.15, in their 2017 study, described ten cases of Madelung’s disease. Three patients underwent surgical correction of neck masses by lipectomy (one case) and liposuction (two cases). In most cases, liposuction was chosen because it is a safe technique, with less downtime and without extensive scarring. Two patients had a recurrence, one after lipectomy and the other after liposuction15.
Based on the therapeutic possibilities available in the literature, and the fact that the patient was young and healthy, we opted for surgical treatment with the combination of lipectomy and liposuction techniques.
Aiming at greater safety in the procedures, an approach was carried out by two different teams, each with an emphasis on its area of operation. The Head and Neck Surgery team performed cervical lipectomy, and the Plastic Surgery team performed abdominal liposuction.
Cervical lesions were addressed by lipectomy, as they were relatively small lesions and easily accessible by cervicotomy. In abdominal injuries, as they are very extensive and distributed throughout the abdominal quadrants, liposuction was chosen, resulting in small, well-positioned scars that allowed the aspiration of a large amount of adipose tissue in all regions of the anterior abdomen.
As he did not present metabolic syndrome, no additional clinical treatment was proposed, only oriented to maintain the regular treatment of systemic arterial hypertension.
The patient was informed of the palliative nature of the approaches since fat deposits can re-accumulate due to the permanence of the defect in lipid metabolism. However, he judged that the aesthetic and psychological benefits would justify the surgical interventions.
In the postoperative period, the patient was satisfied with the aesthetic result, evolved with aesthetically acceptable and well-positioned scars and felt relief from the compressive symptoms he had already been experiencing.
CONCLUSION
Madelung syndrome is a rare disease, and its etiology is not yet fully understood. Due to its involvement in different body segments, the interaction between surgical teams is extremely important in planning the treatment of these patients.
Choosing the right treatment for patients with Madelung syndrome depends on the extent of the disease, age, associated comorbidities, patient expectations, and the surgical team’s experience.
Aware of the potential risk of recurrence, these patients need to be advised with caution in the preoperative period, aligning their expectations with the real palliative purpose of the treatment and informed of the real chances of recurrence.
In the case reported here, the association between the surgical techniques of lipectomy and liposuction provided a favorable esthetic result, in addition to not making future procedures unfeasible, as in the case of lipolytic enzymes, because it was a young patient with the possibility of recurrence.
This study has a postoperative follow-up of less than one year, with no recurrence of the lesions so far. This fact makes it impossible to compare the maintenance of results between the techniques of lipectomy and liposuction.
REFERENCES
1. Chen CY, Fang QQ, Wang XF, Zhang MX, Zhao WY, Shi BH, et al. Madelung’s Disease: Lipectomy or Liposuction? Biomed Res Int. 2018;2018:3975974. DOI: 10.1155/2018/3975974
2. Plummer C, Spring PJ, Marotta R, Chin J, Taylor G, Sharpe D, et al. Multiple Symmetrical Lipomatosis--a mitochondrial disorder of brown fat. Mitochondrion. 2013;13(4):269-76. DOI: 10.1016/j.mito.2013.03.003 PMid:23524250
3. Carlsen A, Thomsen M. Different clinical types of lipomatosis. Case report. Scand J Plast Reconstr Surg. 1978;12(1):75-9. DOI: 10.3109/02844317809010484 PMid:663569
4. Bulum T, Duvnjak L, Car N, Metelko Ž. Madelung’s disease: case report and review of the literature. Diabetol Croat. 2007;36(2): 25-30.
5. Tadisina KK, Mlynek KS, Hwang LK, Riazi H, Papay FA, Zins JE. Syndromic lipomatosis of the head and neck: a review of the literature. Aesthetic Plast Surg. 2015;39(3):440-8. DOI: 10.1007/s00266-015-0478-8 PMid:25860506
6. Tizian C, Berger A, Vykoupil KF. Malignant degeneration in Madelung’s disease (benign lipomatosis of the neck): case report. Br J Plast Surg. 1983;36(2):187-9. DOI: 10.1016/0007- 1226(83)90089-9 PMid:68310198
7. Leung NW, Gaer J, Beggs D, Kark AE, Holloway B, Peters TJ. Multiple symmetric lipomatosis (Launois-Bensaude syndrome): effect of oral salbutamol. Clin Endocrinol (Oxf). 1987;27(5):601-6.
8. Andou E, Komoto M, Hasegawa T, Mizuno H, Hayashi A. Surgical excision of madelung disease using bilateral cervical lymphnode dissection technique-its effect and the influence of previous injection lipolysis. Plast Reconstr Surg Glob Open. 2015;3(4):e375. DOI: 10.1097/GOX.0000000000000337 PMid:25973353 PMCid:PMC4422206
9. Brea-García B, Cameselle-Teijeiro J, Couto-González I, Taboada-Suárez A, González-Álvarez E. Madelung’s disease: comorbidities, fatty mass distribution, and response to treatment of 22 patients. Aesthetic Plast Surg. 2013;37(2):409-16. DOI: 10.1007/s00266-012-9874-5
10. Hugo NE, Conway H. Benign symmetric lipomatosis: a case report. Plast Reconstr Surg. 1966;37(1):69-71.
11. Sonni VF, Pires CEB, Kay MS, Neiva IF, Bier GE. Síndrome de Madelung - Relato de caso. Rev Bras Cir Plast. 1999;14(2):65-74.
12. Adamo C, Vescio G, Battaglia M, Gallelli G, Musella S. Madelung’s disease: case report and discussion of treatment options. Ann Plast Surg. 2001;46(1):43-5.
13. Verhelle NA, Nizet JL, Van den Hof B, Guelinckx P, Heymans O. Liposuction in benign symmetric lipomatosis: sense or senseless?Aesthetic Plast Surg. 2003;27(4):319-21.
14. Constantinidis J, Steinhart H, Zenk J, Gassner H, Iro H. Combined surgical lipectomy and liposuction in the treatment of benign symmetrical lipomatosis of the head and neck. Scand J Plast Reconstr Surg Hand Surg. 2003;37(2):90-6. DOI: 10.1080/02844310005612 PMid:12755508
15. Wollina U, Heinig B. Madelung’s Disease - Case Series and Treatment by Tumescent Liposuction or Lipectomy. Open Access Maced J Med Sci. 2017;5(4):427-31.DOI: 10.3889/oamjms.2017.114
1. Celso Pierro Hospital and Maternity, Plastic Surgery and Head and Neck, Campinas,
SP, Brazil.
Corresponding author: Amanda Bishop Perseguim, Rua Professor Doutor Euryclides de Jesus Zerbini, 1516 - Parque Rural Fazenda Santa Cândida, Campinas, SP, Brazil, Zip Code 13087-57, E-mail: amandaperseguim@hotmail.com
Article received: November 29, 2020.
Article accepted: April 19, 2021.
Conflicts of interest: none.


















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter