

Original Article - Year 2022 - Volume 37 - Issue 1
Evaluation of the epidemiological profile of burned adult patients admitted to a referral center in the interior of the state of Bahia, Brazil
Avaliação do perfil epidemiológico de pacientes adultos queimados internados em um centro de referência no interior do estado da Bahia, Brasil
ABSTRACT
Introduction: Burns are skin lesions caused by heat, with different agents that can compromise muscle tissue, tendons, bones and bring risks of loss of limbs, function or even death of the patient. These are problems that can result in clinical, physical and psychological damage. The objective is to evaluate the epidemiological profile of adult patients admitted to a burn treatment center in the Recôncavo da Bahia over 13 months.
Methods: A retrospective descriptive study evaluated patients' medical records admitted to the institution in question.
Results: In the period in question, 102 adult patients were admitted, with a balance between the male and female sexes. When analyzing the reason for the burn, it can be seen that the majority had burns of an accidental nature. Scalding by hot liquids, including milk, coffee and oil at high temperatures, was the main agent, with 68 cases (66.7%). As for the depth of the injuries, 83 (81.4%) were victims of 2nd-degree burns, 17 (16.7%) of 3rd-degree and 2 (2%) with wound depth not specified in the records. Regarding the outcome, 96 (94.1%) were discharged from the hospital, 3 (2.9%) died, and 3 (2.9%) were transferred to another service.
Conclusion: Burns are preventable, so epidemiological data are tools that contribute to the development of care and prevention aimed at this group. This study may serve to plan public health policies to care for and prevent burns.
Keywords: Burns; Patients; Epidemiology; Accident Prevention; Public health policies.
RESUMO
Introdução: As queimaduras são lesões cutâneas causadas pelo calor, tendo aquelas diversos agentes, que podem comprometer tecido muscular, tendões, ossos e trazem riscos de perda de membros, de função ou até a morte do paciente. São problemas que podem resultar em danos clínicos, físicos e psicológicos. O objetivo é avaliar o perfil epidemiológico dos pacientes adultos internados em um centro de tratamento de queimados no Recôncavo da Bahia, no período de 13 meses.
Métodos: Estudo descritivo retrospectivo, no qual foram avaliados os prontuários médicos dos pacientes internados na instituição em questão.
Resultados: No período em questão, foram admitidos 102 pacientes adultos, existindo um equilíbrio entre os sexos masculino e feminino. Ao analisar o motivo da queimadura, pode-se observar que a maioria apresentava queimaduras de natureza acidental. A escaldadura por líquidos quentes, englobando leite, café e óleo em altas temperaturas, foi o principal agente, com 68 casos (66,7%). Quanto à profundidade das lesões, 83 (81,4%) foram vítimas de queimaduras de 2° grau, 17 (16,7%) de 3° grau e 2 (2%) com profundidade da lesão não especificada nos registros. Com relação ao desfecho, 96 (94,1%) receberam alta hospitalar, 3 (2,9%) foram a óbito e 3 (2,9%) foram transferidos para outro serviço.
Conclusão: A queimadura é um mal evitável, sendo assim, os dados epidemiológicos são ferramentas que contribuem para a elaboração de cuidados e de prevenção voltados para esse grupo. Este estudo poderá servir no planejamento de políticas públicas de saúde voltadas para o atendimento e prevenção a queimaduras.
Palavras-chave: Queimaduras; Pacientes; Epidemiologia; Prevenção de acidentes; Políticas públicas de saúde
INTRODUCTION
Burns are skin lesions caused by heat, with different agents that can compromise muscle tissue, tendons, bones and bring risks of loss of limbs, function or even death of the patient. These are problems that can result in clinical, physical and psychological damage. Treatments involve interruption of the burn, electrolyte replacement, rehydration, pain management, debridement and grafts1.
Burns is a set of injuries that cause injury to organic tissue and are caused by an external agent, resulting from the trauma of thermal, chemical, electrical, friction or radiation, leading to the partial or total destruction of the skin and adjacent tissues2.
This type of trauma can imply, in addition to psychological repercussions, damage to the respiratory, immune, cardiovascular and renal systems, and the risk of infection followed by sepsis, considered the main cause of mortality3.
According to the World Health Organization, burns are the fourth most common type of trauma globally, second only to interpersonal violence, falls and traffic accidents2. However, despite being a traumatic entity quite present in all social groups, burns have become one of the main causes of morbidity and mortality in low- and middle-income countries, such as Brazil4.
In Brazil, it is estimated that one million individuals are burned each year, with no restrictions on sex, age or race, with a strong economic impact, given the prolonged treatment time5 and the burden inherent to the disease6.
Burns, therefore, is an important public health problem in Brazil, being costly to the health system, and requiring long-term follow-up of the patient to deal with possible psychological and physical consequences arising from the incident7,8.
OBJECTIVE
To evaluate the epidemiological profile of adult patients admitted to a burn treatment center in the Recôncavo da Bahia, from June 2019 to June 2020.
METHODS
This is a retrospective descriptive study. For the present study, the medical records of patients admitted to the Burn Treatment Unit of the Santo Antônio de Jesus Regional Hospital were evaluated from June 2019 to June 2020. The following variables were considered: gender; age; period of internment; procedures performed and the number of procedures; existence or not of complications; burned body area; causal agent of the burn; patient’s origin; burn date; date of admission; burned region; reason for the burn (accidental, aggression or self-extermination); degree of burns; ICU indication; comorbidities and deaths. The medical records of patients under 18 years of age or who were not admitted to the Burn Treatment Unit were excluded from the present study, In order to protect the physical and psychological integrity of those involved, assuring them of ethical standards, respecting the Declaration of Helsinki (2000) and the National Health Council - resolution 196/96, this project was submitted to the Ethics Committee in Research (CEP) of the Health Sciences Center (CCS) of the Federal University of Recôncavo da Bahia (UFRB) after the signature of a letter of consent by the Hospital board and data collection was only started after approval by the CEP, under CAAE number 31216820.9.0000.0056.
During data analysis, information from the research participants was cross-referenced, and the frequency and mean of the variables were calculated. Data such as age group4, body surface area burned (BBS)9 and length of stay10 were grouped according to the theoretical framework present in the literature.
RESULTS
In the 13 months analyzed at the Burn Treatment Unit, 102 adult patients were admitted, whose epidemiological data were summarized in Table 1.
| n | % | ||
|---|---|---|---|
| Sex | Masculine | 51 | 50.0 |
| Feminine | 51 | 50.0 | |
| Comorbidities | Present | 28 | 27.5 |
| Absent | 74 | 72.5 | |
| Age group | 18-25 | 22 | 21.6 |
| 26-40 | 31 | 30.4 | |
| 41-55 | 33 | 32.4 | |
| 56-65 | 9 | 8.8 | |
| 66+ | 7 | 6.9 | |
| Burn degree | 2nd-degree | 83 | 81.4 |
| 3rd-degree | 17 | 16.7 | |
| Not registered | 2 | 2.0 | |
| BBS | 0-10% | 62 | 60.8 |
| 11-20% | 15 | 14.7 | |
| 21-30% | 2 | 2.0 | |
| >31% | 3 | 2.9 | |
| Cause of burn | Accident | 92 | 90.2 |
| Aggression | 6 | 5.9 | |
| Self-extermination | 2 | 2.0 | |
| Not registered | 2 | 2.0 |
BBS: Burned Body Surface
There was a balance between male and female and, of the 102 hospitalized patients, most did not have comorbidities.
When analyzing the reason for the burn, whether of an accidental nature, aggression or self-extermination, it can be observed that the majority had burns of an accidental nature.
In addition, several causal agents of burns were observed. Scalding by hot liquids, including milk, coffee and oil at high temperatures, was the main agent, with 68 cases (66.7%). The second cause was direct contact with a flame, corresponding to 18 cases (17.6%). Four patients (3.9%) were victims of electrical burns. Four patients with unspecified burns were registered, representing 3.9% of the sample.
When looking at the time elapsed between the accident and admission to the burn center, it can be seen that 55 patients (53.9%) took up to 5 days to seek care, while 3 (2.9%) delayed up to 16 days or most.
As for the depth of the injuries, 83 (81.4%) were victims of 2nd-degree burns, 17 (16.7%) of 3rd-degree and 2 (2%) with wound depth not specified in the records. The records of the affected body regions were present in 100 medical records, with the lower limbs being the most affected, with 24.5% of the cases; followed by the upper limbs, with 19.6%; head and neck, with 16.7%; and multiple lesions, with 15.7%.
The most prevalent BBS was up to 10%, found in 62 patients (60.8%). Twenty patients had their BBS missing from the medical records.
As for the procedures performed, all patients in the sample underwent surgical debridement, 68 patients underwent debridement only (66.7%), 32 underwent debridement and grafting (31.4%), and 2 patients (2%) underwent grafting and retail.
Regarding the length of stay, 30 patients stayed 16 days or more in the hospital (29.4%), and 29 patients stayed up to 5 days.
Regarding the outcome, 96 (94.1%) were discharged from the hospital, 3 (2.9%) died, and 3 (2.9%) were transferred to another service. Regarding the ICU indication, 4 (3.9%) patients had an established indication, while 98 (96.1%) were treated in common ward beds.
When analyzing the overall mortality of patients, the result is 3 deaths (2.9%). Of all hospitalized patients, 12 (11.8%) had complications in their treatment, and 87 (85.3%) did not.
When comparing comorbidities with deaths (Table 2), it is observed that, of the three deaths that occurred, 66% had no comorbidities.
| Deaths | |||
|---|---|---|---|
| Yes | No | ||
| Presence of comorbidities | Yes | 1 | 27 |
| No | 2 | 72 | |
| TOTAL | 3 | 99 | |
When comparing deaths with complications (Table 3), it can be seen that most patients had no complications and did not die.
| Deaths | |||
|---|---|---|---|
| Yes | No | ||
| Presence of complications | Yes | 3 | 10 |
| No | 0 | 89 | |
| TOTAL | 3 | 99 | |
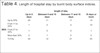
It can be seen that, when comparing BBS with the length of hospital stay (Table 4), there was a certain balance in the period spent in the hospital environment.
| length of stay | |||||
|---|---|---|---|---|---|
| Up to 5 days | Between 6 and 10 days | Between 11 and 15 days | 16 days or more | ||
| BBS | Up to 20% | 20 | 11 | 17 | 14 |
| From 11 to 20% | 1 | 0 | 4 | 10 | |
| From 21 to 30% | 1 | 0 | 0 | 1 | |
| More than 30% | 2 | 1 | 0 | 0 | |
| TOTAL | 24 | 12 | 21 | 25 | |
BBS: Burned Body Surface
DISCUSSION
According to the Ministry of Health, there were 966 hospitalizations of adults for burns and corrosion in Bahia from November 2018 to November 2019. When comparing this same period and this same age group to the Northeast Region, this number increases to 4081 admissions. In the entire national territory, in the same period and age group, there were a total of 16,231 hospitalizations11.
The epidemiological data of patients admitted to the burn treatment unit are of paramount importance as it is a way of knowing the main factors related to burns and developing preventive measures that reduce the incidence of such events12.
In the period studied, from June 2019 to June 2020, 102 medical records were analyzed, in which females and males were equally affected by burns, a prevalence that differs from other studies2,4,5. This finding can be explained by the risk of accidents offered by the residence for the occurrence of burns13.
Regarding the age group, the patients most affected by burns belonged to the 41 to 55 group. In the literature, 20 to 24 years old, followed by 35 to 39 years old, were the most prevalent, which differs from the results of this research4.
The reason for the burn is following the literature, in which most burns are accidental in nature14. The most common causal agents were hot liquids and flame, corroborating the literature3.
According to the literature, the most affected regions were lower limbs and upper limbs, which shows the limbs as the most affected; however, the present study differs from the others in terms of this involvement15. Concerning the depth of the injuries, second-degree burns were the most prevalent in this study. Similar results were found in other studies2,16.
Surgical debridement was the most performed procedure in patients, a result also obtained in the literature4, in which debridement was responsible for 58.74% of procedures performed in burn patients in Indonesia.
The length of hospital stay in this research, which averaged 11 to 15 days, agrees with the literature, which shows an average of 13.3 days3, which the reduced specialized team can justify, and not available on all days of the week, postponing some procedures in the area, and extending the length of stay.
Complications were found in 11.8% of the patients, a value that differs from that found in the literature8, which resulted in complications in 63.1% of the patients, which can again be explained by the level of complexity of the referred burn center. The smaller sample size can also explain this difference in this research (102).
In this study, there was a prevalence of hospital discharge, and only 2.9% had death as an outcome, a result also found in the literature16, with 97.1% of patients being discharged and 2.7% dying. Despite converging with results from other studies, these data can be justified by the proposal of the burn center studied, that is, because it is a care unit for small and medium burns, these numbers become biased, since large burns, the main responsible for the mortality rates of this condition, are promptly transferred to other institutions.
In this context, epidemiological studies are valuable because they create information for carrying out preventive public health policies17, thus showing the importance of carrying out this work, aiming at improving public assistance to burn victims with greater efficiency and effectiveness.
However, this work is limited by the absence of some variables in the patients’ charts or incomplete information. In addition, this research brings specific data from a region in the interior of Bahia, which may not be compatible with other regions.
CONCLUSION
In this study, in the epidemiological profile of the patients, there was an equality in prevalence between the sexes, aged between 41 and 55 years and without comorbidities. The main causal agent was scalding, followed by direct contact with flame. There was a prevalence of second-degree burns, and the main reason that led to the burn was accidental.
Burning is an avoidable evil, so epidemiological data are tools that contribute to the development of care and prevention aimed at this group to reduce burns accidents.
This study may serve to plan public health policies to care for and prevent burns.
REFERENCES
1. Nascimento SB, Soares LSS, Areda CA, Saavedra PAE, Leal JVO, Adorno J, et al. Perfil dos pacientes hospitalizados na unidade de queimados de um hospital de referência de Brasília. Rev Bras Queimaduras. 2015;14(3):211-7.
2. Arruda FCF, Castro BCO, Medeiros JF, Valadão WJ, Reis GMD. Análise epidemiológica de 2 anos na Unidade de Queimados do Hospital de Urgências Governador Otávio Lage de Siqueira, Goiânia, Brasil. Rev Bras Cir Plást. 2018;33(3):389-94.
3. Mola R, Fernandes FECV, Melo FBS, Oliveira LR, Lopes JBSM, Alves RPCN. Características e complicações associadas às queimaduras de pacientes em unidade de queimados. Rev Bras Queimaduras. 2018;17(1):8-13.
4. Wardhana A, Basuki A, Prameswara ADH, Rizkita DN, Andarei AA, Canintika AF. The epidemiology of burns in Indonesia’s national referral burn center from 2013 to 2015. Burns Open. 2017;1(2):67-73.
5. Zafani RT, Perrone RP, Vilaça DT, Faro SF, Moraes CM, Souza GCVF. Análise da evolução dos pacientes queimados de acordo com seu perfil epidemiológico na Santa Casa de Misericórdia de Santos, Brasil. Rev Bras Cir Plást. 2018;33(3):395-8.
6. Silva TBL, Oliveira CM, Felisberto D, Nigro MVAS, Kusano LDC, Mialski JR. Caracterização epidemiológica de pacientes queimados atendidos no Serviço de Queimados do Hospital Universitário Evangélico Mackenzie de Curitiba no Ano de 2017. Rev Bras Cir Plást. 2019;34(Suppl 1):70-2.
7. Marinho LP, Andrade MC, Goes Junior AMO. Perfil epidemiológico de vítimas de queimadura internadas em hospital de trauma na região Norte do Brasil. Rev Bras Queimaduras. 2018;17(1):28-33.
8. Silva JAC, Vendramin FS, Martins MM, Lima AVM, Cunha LM, Borborema CLP. Epidemiologia, principais complicações e mortalidade dos pacientes atendidos em um Centro de Tratamento de Queimados na Amazônia. Rev Bras Cir Plást. 2018;33(1):104-9.
9. Dutra JPS, Custódio SR, Piccolo N, Daher RP. Estudo clínico-epidemiológico de pacientes queimados internados em uma unidade de terapia intensiva em Goiás. Rev Bras Queimaduras. 2017;16(2):87-93.
10. Giuli AE, Itakussu EY, Valenciano PJ, Fujisawa DS, Trelha CS. Caracterização de idosos vítimas de queimaduras internados em um centro de tratamento de queimados. Rev Bras Queimaduras. 2015;14(4):253-6.
11. Brasil. Ministério da Saúde. DATASUS. Informações de Saúde. Epidemiológicas e morbidade [acesso 2020 Fev 2]. Disponível em: http://www2.datasus.gov.br/DATASUS/index.php?area=0203&id=6926
12. Soares LR, Barbosa FS, Santos LA, Mattos VCR, De-Paula CA, Leal PML, et al. Estudo epidemiológico de vítimas de queimaduras internadas em um hospital de urgência da Bahia. Rev Bras Queimaduras. 2016;15(3):148-52.
13. Gawryszewski VP, Bernal RTI, Silva NN, Morais Neto OL, Silva MMA, Mascarenhas MDM, et al. Atendimentos decorrentes de queimaduras em serviços públicos de emergência no Brasil, 2009. Cad Saúde Pública. 2012;28(4):629-40.
14. Hernández CMC, Núñez VP, Banqueris RF, Gil SRL, Suárez FAP, García MS. Caracterização epidemiológica de 4 anos dos pacientes grandes queimados no Hospital “Celia Sánchez Manduley”, 2015 - 2018. Rev Bras Cir Plást. 2020;35(1):78-82.
15. Pereira NCS, Paixão GM. Características de pacientes internados no centro de tratamento de queimados no estado do Pará. Rev Bras Queimaduras. 2017;16(2):106-10.
16. Soares ALS, Saraiva ABC, Rêgo ALC, Lima GM, Nicolau-da-Costa LR. Características clínico-epidemiológicas de pacientes internados em um hospital de referência em queimaduras na Amazônia brasileira. Rev Bras Queimaduras. 2019;18(2):102-6.
17. Lacerda LA, Carneiro AC, Oliveira AF, Gragnani A, Ferreira LM. Estudo epidemiológico da Unidade de Tratamento de Queimaduras da Universidade Federal de São Paulo. Rev Bras Queimaduras. 2010;9(3):82-8.
1. Federal University of Recôncavo da Bahia, Cruz das Almas, BA, Brazil.
| COLLABORATIONS | |
|---|---|
| ACSP | Analysis and/or data interpretation, Conception and design study, Conceptualization, Data Curation, Final manuscript approval, Formal Analysis, Investigation, Methodology, Project Administration, Writing - Original Draft Preparation, Writing - Review & Editing |
| KLNC | Analysis and/or data interpretation, Conception and design study, Conceptualization, Data Curation, Final manuscript approval, Formal Analysis, Investigation, Methodology, Project Administration, Writing - Original Draft Preparation, Writing - Review & Editing |
| PPAF | Conception and design study, Conceptualization, Final manuscript approval, Methodology, Project Administration, Supervision, Writing - Review & Editing |
| JLOJ | Conception and design study, Conceptualization, Final manuscript approval, Methodology, Project Administration, Supervision, Writing - Review & Editing |
| MNSR | Conception and design study, Final manuscript approval, Methodology, Writing - Review & Editing |
Corresponding author: Paulo Plessim de Almeida Filho, Alameda Salerno, 113, Apartment 1801A, Pituba, Salvador, BA, Brazil, Zip Code 41830-500, E-mail: pauloplessim@ufrb.edu.br
Article received: March 24, 2021.
Article accepted: April 19, 2021.
Conflicts of interest: none.







 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter