

Original Article - Year 2022 - Volume 37 -
Dermolipectomies after bariatric procedures in the Public Health System: a long way to go
Dermolipectomias após procedimentos bariátricos no Sistema Público de Saúde: um longo caminho a percorrer
ABSTRACT
Introduction: Obesity is one of the main health problems faced by the population, and its incidence has gradually increased in recent decades. Amid the global obesity epidemic, bariatric procedures have increased significantly and, despite the growing number of post-bariatric procedures, these are not equivalent to the number of bariatric surgeries.
Methods: Data were collected from the public health registry (DATASUS) between 2008 and 2019 to analyze the selected parameters, with an assessment of the main post-bariatric dermolipectomy techniques, their distribution in the national territory, their length of stay, their mortality, costs for the Public System, the comparison between post-bariatric dermolipectomies and the distribution of bariatric procedures in the national territory. Furthermore, dermolipectomies and the distribution of plastic surgeons in Brazil were compared.
Results: An increase of 164% was evidenced in the number of postbariatric dermolipectomies during the studied period. Post-bariatric abdominal dermolipectomy was the most performed procedure, accounting for 65% of the procedures, followed by brachial (14.8%), crural (14.7%) and circumferential (4.7%) dermolipectomy. There was an inequality in the distribution of post-bariatric procedures among Brazilian macro-regions, with the Southeast Region having the highest percentage (49.8%) of dermolipectomies.
Conclusions: Despite the progressive increase in post-bariatric dermolipectomies, they did not follow the number of bariatric procedures in the national territory. Therefore, there is a need for a parallel growth between both so that there is complementation in treating these patients. Then, there might be an improvement in the distribution of dermolipectomies in the national territory, allowing more patients to benefit.
Keywords: Abdominoplasty; Obesity; Unifield Health System; Bariatric surgery; Lipectomy.
RESUMO
Introdução: A obesidade é um dos principais problemas de saúde enfrentados pela população e sua incidência cresce gradativamente nas últimas décadas. Em meio à epidemia global de obesidade, os procedimentos bariátricos aumentaram expressivamente e, apesar do crescente número dos procedimentos pós-bariátricos, esses não se equivalem ao número de cirurgias bariátricas.
Métodos: Foram coletados dados do registro de saúde pública (DATASUS) entre 2008 e 2019 para análise dos parâmetros selecionados, com avaliação das principais técnicas de dermolipectomia pós-bariátrica, sua distribuição em território nacional, seu tempo de internação, sua mortalidade, os custos para o Sistema Público, a comparação entre as dermolipectomias pós-bariátricas e a distribuição dos procedimentos bariátricos no território nacional. Além disso, comparou-se as dermolipectomias e a distribuição de cirurgiões plásticos no Brasil.
Resultados: Um aumento de 164% foi evidenciado no número de dermolipectomias pós-bariátricas durante o período estudado. A dermolipectomia abdominal pós-bariátrica foi o procedimento mais realizado, sendo responsável por 65% dos procedimentos, seguido da dermolipectomia braquial (14,8%), crural (14,7%) e circunferencial (4,7%). Observou-se uma desigualdade na distribuição dos procedimentos pós-bariátricos entre as macrorregiões brasileiras, sendo a Região Sudeste com o maior número percentual (49,8%) de dermolipectomias.
Conclusões: Apesar do aumento progressivo do número de dermolipectomias pós-bariátricas, elas não acompanharam o número de procedimentos bariátricos em território nacional. Por isso, há necessidade de um crescimento paralelo entre ambas, para que haja uma complementação no tratamento desses pacientes. Sendo assim, poderá existir melhora na distribuição das dermolipectomias no território nacional, fazendo com que mais pacientes possam ser beneficiados.
Palavras-chave: Abdominoplastia; Obesidade; Sistema Único de Saúde; Cirurgia bariátrica; Lipectomia
INTRODUCTION
Obesity is defined by the World Health Organization (WHO) as the abnormal or excessive accumulation of body fat in the form of adipose tissue. It is considered a disease of multifactorial etiology, encompassing genetic, behavioral, metabolic and environmental factors. Today, the consequences related to obesity are considered one of the most serious problems faced in Brazilian public health and other countries. The WHO currently considers that, in developed countries, they are the main health problems to be faced. The increase in the incidence and prevalence of obesity is mainly due to the lifestyle, the consumption of foods rich in fats and sugars, the sedentary lifestyle, and the reduction of fiber consumption1.
Currently, in Brazil, data from the Brazilian Institute of Geography and Statistics (IBGE - Instituto Brasileiro de Geografia e Estatística - in portuguese) show that overweight and obesity have a prevalence of approximately 50%, both for men and women, in the population with a range age above 20 years2.
Initially, the recommendation for the treatment of obesity is based on nutritional monitoring, physical activity, and medications, when indicated. However, when it reaches grade III (body mass index - BMI>40), the clinical treatment results are unsatisfactory in 95% of patients. Those end up regaining the initial pre-nutritional weight in up to two years3.
Bariatric surgeries are various procedures aimed at weight reduction and treating diseases associated with or aggravated by excess weight4. Thus, bariatric surgery (BS) constitutes the most effective alternative for treating morbid obesity and its complications in the group of refractory patients5. According to the resolution of the Federal Council of Medicine (CFM)6,7 and the Brazilian legislation, the indications are for adult patients with BMI>40 or BMI>35 and life-threatening comorbidities, refractory to medical treatment for at least two years. Adolescents aged 16 and under may be operated on, but, in addition to the above requirements, a pediatrician must be present in the multidisciplinary team. In addition, it is necessary to be observed consolidation of the cartilages of the wrist growth epiphyses.
The last resolution (nº 2.172/2017) of this Council added the use of BS in patients with diabetes as an adequate technique for the treatment of this disease, for individuals between 30-70 years old with diabetes type 2 diabetes and BMI between 30-34.9 as long as the disease has not been controlled with clinical treatment. The patient must have a definite diagnosis of type 2 diabetes for less than 10 years and not have contraindications for the proposed surgical procedure. In addition, the individual must have undergone other attempts to treatment by conventional methods (nutritional and physical activity) and have the psychological conditions to follow the new diet imposed after the surgery.
Weight loss occurs in the period of 12 to 18 months, leading to excess skin and sagging, and the best time to perform body contouring procedures is between 18 and 24 months.8. Thus, as a form of repair, the search for plastic surgery has been growing to correct the secondary consequences of bariatric surgery, especially for abdominal dermolipectomy. This may improve the quality of life of surgically treated patients. The abdomen is an important point of deformity after major weight loss, causing difficulties in daily life, such as personal hygiene, social interaction, and intimate life9.
Dermolipectomy for the treatment of excess skin in ex-obese patients began at the beginning of the 20th century, with Kelly10. Several authors have made variations in the technique: in the 1960s, Castañares & Goethel11 proposed vertical and horizontal resection, giving the final scar an anchor aspect; in the 1970s, Regnault12,13 advocated the removal of excess skin with a “fleur-de-lis” marking. The transverse abdominoplasty was proposed by Pitanguy14, performing a large detachment of the abdominal flap and plication of the rectus abdominis muscles to correct the diastasis. These techniques are still in use by most surgeons.
Post-bariatric plastic surgery gained strength amid the global epidemic of obesity in the 1990s. It attracted the attention of specialists from all over Brazil in the first course of the Post-Bariatric Chapter, at the 42nd Brazilian Congress of Plastic Surgery, held in 2005, in Belo Horizonte, Minas Gerais. This procedure evolved gradually in the important task of restoring self-esteem to patients recently submitted to bariatric surgery15.
The WHO projects that by 2025, about 2.3 billion adults worldwide will be overweight (today, more than 700 million people are obese). The estimate considers that, in 2017 alone, according to the Brazilian Society of Bariatric and Metabolic Surgery, 105,642 bariatric surgeries were performed throughout the national territory. Our team assumes that the post-bariatric patient needs, on average, at least two post-bariatric surgeries, abdominal dermolipectomy and torsoplasty. However, they may need mammoplasty, thighplasty, brachioplasty, among others. Considering that each patient requires more than one surgical intervention, based on 2017, the demand for surgeries would reach about 200 thousand per year across the country. These numbers would generate a demand of approximately 550 post-bariatric plastic surgeries per day in Brazil15.
OBJECTIVE
This study aims to analyze the current level of reconstructive surgical treatment provided to post-bariatric patients performed by the Brazilian Public Health System, given the increase in bariatric surgeries performed.
It aims to question the managers and professionals involved in combating obesity to formulate public policies for treating obese patients in their entirety, establishing strategies so that post-bariatric surgeries (PBS) can be instituted for a greater number of patients, tracing physical and psychological benefit.
METHODS
A cross-sectional study was carried out to analyze the prevalence of post-bariatric dermolipectomy procedures between January 2008 and December 2019. Data were extracted from DATASUS (Brazilian Public Health Registry Database). The affiliated hospitals that are part of the Unified Health System (SUS) issue a Hospital Admission Authorization (AIH), which identifies the procedure performed, the proposed treatment, and the transfer carried out later by the government. In the DATASUS system, data are pre-selected and organized into tables that allow cross-referencing information on the period, region, and other interest data.
For the study, data were collected from post-bariatric abdominal dermolipectomies, brachial dermolipectomy, crural dermolipectomy and circumferential dermolipectomy, the first three computed from 2008 to 2019, while circumferential dermolipectomies from the year 2013. They were then compared respective frequencies in the Brazilian regions with the number of bariatric surgeries also collected through DATASUS, and regarding the number of plastic surgeons in the national territory, in the same period.
The number of plastic surgeons in the country was obtained in the Medical Demography study (2018), coordinated by Dr. Mário Scheffer, from the Department of Preventive Medicine, Faculty of Medicine, University of São Paulo (FMUSP). Considering that there was no contact with patients during this work, there were no ethical problems in this research, eliminating the need for release by the ethics committee.
RESULTS
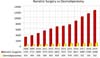
The main dermolipectomy techniques and their respective frequencies are shown in Table 1. There is a predominance of the abdominal dermolipectomy technique in the years evaluated, being responsible for 65.6% of the procedures compared to other techniques: brachial dermolipectomy (14.8%), crural dermolipectomy (14.7%), and circumferential dermolipectomy (4.7%). The graphic representation of the increase in surgeries in the evaluated period, year by year, is shown in Figure 1.
| Technique | Frequency |
|---|---|
| Post-bariatric abdominal dermolipectomy | 6242 |
| Post-bariatric brachial dermolipectomy | 1409 |
| Post-bariatric crural dermolipectomy | 1399 |
| Post-bariatric circumferential abdominal dermolipectomy | 455 |
There was a progressive increase in the number of procedures performed between the years 2008-2019, with 425 dermolipectomies performed in 2008, while in 2019, there were 1124 surgeries performed, an increase of 164%. Abdominal dermolipectomy was the most performed surgery in all country regions during this period, representing 80% of the total surgeries performed in 2008 and 66% of the total in 2019. The Southeast Region had the highest absolute number of surgeries performed during the period, with 4739 (49.8%) surgeries, followed by the South Region, with 2988 (31.4%) procedures. The Northeast, Midwest and North regions carried out, respectively, 986 (10.3%), 655 (6.8%) and 137 (1.4%) surgeries. The region that showed the greatest increase in the number of procedures in the period was the Southeast Region, with 224%, followed by the Northeast Region (160%), South (142%) and Midwest (65%). The North Region showed a decrease of 60% in the number of procedures during the period evaluated. The number of procedures per region can be seen in Table 2.
| Abdominal | Brachial | Crural | Circumferential | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2008 | 2013 | 2019 | 2008 | 2013 | 2019 | 2008 | 2013 | 2019 | 2013 | 2019 | ||||
| North | 10 | 9 | 4 | 0 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| North East | 38 | 32 | 77 | 7 | 17 | 31 | 8 | 9 | 26 | 4 | 4 | |||
| Southeast | 113 | 286 | 377 | 27 | 82 | 60 | 26 | 64 | 75 | 7 | 26 | |||
| South | 149 | 191 | 239 | 0 | 24 | 42 | 7 | 24 | 54 | 1 | 43 | |||
| Midwest | 31 | 38 | 52 | 6 | 15 | 8 | 3 | 11 | 6 | 0 | 0 | |||
When analyzing the distribution of the number of plastic surgeons (PS), it can be observed that between 201116 and 201817, the Southeast Region maintained the highest absolute numbers, with 2653 PS in 2011 and 3956 in 2018 (representing 62.7% of the total PS in the last year), followed in 2018 by the regions: South with 1031 (16.3% of the total), Northeast 753 (11.9%), Midwest 402 (6.3%) and North with 162 PS (2.5%).
As for the percentage increase in PS by region, the Central-West Region presented the most expressive growth, with 88% (213 in 2011 to 402 PS in 2018), followed by the North regions 84% (88 to 162 PS), South 68% (611 to 1031), Northeast 66% (451 to 753 PS) and Southeast 49% (2653 to 3956). The comparison between the number of plastic surgeons and dermolipectomies can be seen in Figure 2. The analysis between the number of post-bariatric dermolipectomies and bariatric surgeries can be seen in Figure 3.
DISCUSSION
In the last five decades, the change in eating habits, the increase in sedentary lifestyle, the increase in income of classes C and D, the presence of genetic factors and the consumption of less healthy products, among others, have been contributing to the increase in overweight and obesity in Brazil. A survey carried out in 2017 by the Surveillance of Risk Factors and Protection for Chronic Diseases sector of the Ministry of Health showed that 19% of the population is obese and that more than half of this population (54%) is overweight18. In absolute numbers, there are more than one million people with severe obesity in the country, mainly affecting women19.
In this context, the number of bariatric procedures has been growing dramatically in the national territory and, therefore, there is a greater demand for aesthetic and functional surgery20,21. Thus, both must be treated together, or the treatment will be compromised. There is still no consensus on the psychiatric and psychological consequences of not removing excess skin or waiting time until these procedures are carried out.
This search can be clearly assessed by the 164% increase in post-bariatric plastic procedures in the last decade alone (2008-2019). However, the demand for BS in the same decade increased by 339%22, demonstrating the lack of continuity in treating these patients undergoing BS. These patients usually present considerable distortion in the body contour, with excess skin, flaccidity, difficulty in movement and personal hygiene, which can cause skin infections. Our service perceives that the estimated demand after the patient undergoes bariatric surgery is, on average, two post-bariatric surgeries (abdominal dermolipectomy and torsoplasty with or without mammoplasty). In this way, we analyze that this national gap has increased annually.
The Brazilian territory presents enormous disparity between the large regions in the number of BSs carried out, with the majority of the procedures being the most developed, concentrating in the South and Southeast 94.5% of the entire amount of BSs in the public system in Brazil22. When analyzing the dermolipectomies, it can be seen that both regions together also present the majority of post-bariatric plastic surgeries, with 81.2%, concentrating mainly in the Southeast Region, with 49.8% of the procedures, which contrasts with a greater number of BS in the South Region, with 56%. While the South Region had the biggest increase in BS, 505% in the last decade, it had only the third biggest increase in PBS, with 142%. The other Brazilian regions also did not follow the demand for BS, with the previous increase having been higher in all regions of Brazil. The discrepancy in the increase in procedures can be evaluated in Figure 3.
Analyzing the number of PBS, it is observed that in 2018 Brazil had one plastic surgeon for every 33,312 inhabitants17,19, a number considered high compared to other countries. After analyzing the distribution of PS in the national territory, it was evaluated that there is a discrepancy in the number of professionals, corresponding to a disparity in PBSs in Brazil. The Southeast Region, which has the highest number of plastic surgeons, 62.7%, also had the highest number of procedures, with 49.8%, followed by the southern regions, with 16.3% of PS and 31.4% of procedures; Northeast, with 11.9% of PS and 10.3% of PBS; Midwest, 6.3% PS and 6.8% of PBS; and North, with 2.5% of PS and 1.4% of PBS.
According to the Ministry of Health data, the average length of hospital stay for PBS was two days23, with the average value of each hospitalization being R$ 887.96. When evaluating the average value of post-bariatric abdominal dermolipectomies, the most performed procedure, the average cost of hospitalization was R$ 879.56. The amount invested in the last decade was R$ 8,440,057.57 in all PBS.
Amid the presented scenario, important discussions must be raised. The first is about the relevant but still deficient increase in the number of PBSs compared to CBs. Given the increasing number of obese people and the public system’s investments in BS, it is analyzed that they are not being satisfactory to carry out the complete treatment of the ex-obese patient. The waiting list and waiting time for dermolipectomies in the national territory are unknown, but based on the service where the study was carried out, it is estimated to be approximately 30 years.
The second point is the inequality in the distribution of PSs, which, despite the large number per inhabitants, are concentrated in the most developed centers of the country, which contributes to the fact that part of the population is not favored in this complementary treatment.
CONCLUSION
Analyzing that the number of bariatric surgeries has increased considerably in the last decade, we understand that dermolipectomies must, in turn, accompany such growth so that there is complementation in the treatment of patients. In this way, we assess that the level of post-bariatric procedures is outdated. We also point out that the approach to other dermolipectomy procedures in addition to the abdominal should be performed more frequently. Likewise, these procedures must be better distributed in the national territory so that more patients can be covered.
REFERENCES
1. Souza JMB, Ribeiro AN, Almondes KM, Castro MM, Maia EMC, Silva NG. Obesidade e tratamento: desafio comportamental e social. Rev Bras Ter Cogn [Internet]. 2005;1(1):59-67 [acesso 2020 Aug 15]. Disponível em: http://www.rbtc.org.br/detalhe_artigo.asp?id=7
2. Brasil. Instituto Brasileiro de Geografia e Estatística (IBGE). Uma análise das condições de vida da população brasileira. Síntese dos Indicadores Sociais: 2016. Rio de Janeiro: IBGE; 2016.
3. Segal A, Fandiño J. Indicações e contra-indicações para realização das operações bariátricas. Rev Bras Psiquiatr [Internet]. 2002 Dec [acesso 2020 Ago 15];24(Suppl 3):68-72. Disponível em: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1516-44462002000700015&lng=pt&tlng=pt
4. Mansur AEC, Balbinot P, Colpo PG, Ascenço ASK, Freitas RS. Braquio-dorso-mamoplastia: cirurgia do contorno corporal da região superior do tronco após grandes perdas ponderais. Rev Bras Cir Plást. 2016;31(3):339-46.
5. Lyra R, Oliveira M, Lins D, Cavalcanti N, Gross JL, Maia FFR, et al. Diretrizes Sociedade Brasileira de Diabetes. Volume 5. Diabetes Mellitus Tipo 1 e Tipo 2. São Paulo: Sociedade Brasileira de Diabetes; 2020. p. 709-17.
6. Conselho Federal de Medicina (CFM). CFM divulga critérios exigidos para a realização de cirurgia metabólica no País [Internet]. Brasília: CFM; 2017 [acesso 2020 Ago 15]. Disponível em: https://portal.cfm.org.br/noticias/cfm-divulga-criterios-exigidos-para-a-realizacao-de-cirurgia-metabolica-no-pais/
7. Conselho Federal de Medicina (CFM). CFM detalha lista de comorbidades que podem levar a indicação da cirurgia bariátrica [Internet]. Brasília: CFM: 2016 [acesso 2020 Ago 15]. Disponível em: https://portal.cfm.org.br/noticias/cfm-detalha-lista-de-comorbidades-que-podem-levar-a-indicacao-da-cirurgia-bariatrica/
8. Grando MC. Dermolipectomia em âncora após cirurgia bariátrica: complicações e índice de satisfação dos pacientes. Rev Bras Cir Plást. 2015;30(4):515-21.
9. Donnabella A, Neffa L, Barros BB, Santos FP. Abdominoplastia pós cirurgia bariátrica: experiência de 315 casos. Rev Bras Cir Plást. 2016;31(4):510-5.
10. Kelly HA. Excision of the fat of the abdominal wall lipectomy. Surg Gynecol Obstet. 1910;10:229-31.
11. Castañares S, Goethel JA. Abdominal lipectomy: a modification in technique. Plast Reconstr Surg. 1967 Oct;40(4):378-83.
12. Regnault P. Abdominoplasty by the W technique. Plast Reconstr Surg. 1975 Mar;55(3):265-74.
13. Regnault P. Abdominal dermolipectomies. Clin Plast Surg. 1975 Jul;2(3):411-29.
14. Pitanguy I. Abdominal lipectomy. Clin Plast Surg. 1975 Jul;2(3):401-10.
15. Oliveira L. Pós-bariátrica em foco [Internet]. São Paulo: Sociedade Brasileira de Cirurgia Plástica; 2019 [acesso 2020 Ago 15]. Disponível em: http://www2.cirurgiaplastica.org.br/blog/2019/05/15/pos-bariatrica-em-foco/
16. Scheffer M, Cassenote A, Poz MRD, Matijasevitch A, Castilho EA, Oliveira RA, et al. Demografia Médica no Brasil 2015 [Internet]. Departamento de Medicina Preventiva, Faculdade de Medicina da USP. São Paulo: Conselho Regional de Medicina do Estado de São Paulo. Conselho Federal de Medicina; 2015. 284 p [acesso 2020 Ago 15]. Disponível em: http://www.usp.br/agen/wp-content/uploads/DemografiaMedica30nov20153.pdf
17. Scheffer M, Cassenote A, Guilloux AGA, Miotto BA, Mainardi GM, Matijasevitch A, Luna Filho B, et al. Demografia médica no Brasil 2018 [Internet]. São Paulo: Departamento de Medicina Preventiva da Faculdade de Medicina da USP; Conselho Regional de Medicina do Estado de São Paulo; Conselho Federal de Medicina; 2018. 286 p [acesso 2020 Ago 15]. Disponível em: http://www.epsjv.fiocruz.br/sites/default/files/files/DemografiaMedica2018(3).pdf
18. Castilho I, Maciel V. Com obesidade em alta, pesquisa mostra brasileiros iniciando vida mais saudável [Internet]. Brasília: Ministério da Saúde; 2018 [acesso 2020 Ago 15]. Disponível em: https://www.gov.br/saude/pt-br/assuntos/noticias/2018/junho/apesar-de-obesidade-em-alta-pesquisa-mostra-brasileiros-mais-saudaveis
19. Brasil. Instituto Brasileiro de Geografia e Estatística (IBGE). Projeções e estimativas da população do Brasil e das Unidades da Federação [Internet]. Rio de Janeiro: IBGE; 2020 [acesso 2020 Ago 17]. Disponível em: https://www.ibge.gov.br/apps/populacao/projecao/
20. Vico PG, De Vooght A, Nokerman B. Circumferential body contouring in bariatric and non-bariatric patient. J Plast Reconstr Aesthet Surg. 2010 May;63(5):814-9.
21. van der Beek ES, van der Molen AM, van Ramshorst B. Complications after body contouring surgery in post-bariatric patients: the importance of a stable weight close to normal. Obes Facts. 2011;4(1):61-6.
22. Tonatto-Filho AJ, Gallotti FM, Chedid MF, Grezzana-Filho TJM, Garcia AMSV. Bariatric surgery in Brazilian Public Health System: the good, the bad and the ugly, or a long way to go. Yellow sign! Arq Bras Cir Dig. 2019 Dec 20;32(4):e1470.
23. Brasil. Ministério da Saúde. DATASUS [Internet] [acesso 2020 Ago 15]. Disponível em: http://tabnet.datasus.gov.br/cgi/deftohtm.exe?sih/cnv/qiuf.def
1. Curitiba Clinical Hospital, Plastic Surgery, Curitiba, Paraná, Brazil.
| COLLABORATIONS | |
|---|---|
| AJTF | Analysis and/or data interpretation, Conception and design study, Conceptualization, Data Curation, Formal Analysis, Investigation, Methodology, Project Administration, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing. |
| JLM | Data Curation, Methodology, Visualization, Writing - Review & Editing. |
| FGL | Analysis and/or data interpretation, Formal Analysis, Supervision, Writing - Review & Editing. |
| SHM | Analysis and/or data interpretation, Data Curation, Formal Analysis, Methodology, Supervision, Writing - Review & Editing. |
| VSO | Analysis and/or data interpretation, Data Curation, Formal Analysis, Visualization, Writing - Review & Editing. |
| CP | Analysis and/or data interpretation, Conceptualization, Formal Analysis, Methodology, Visualization, Writing - Review & Editing. |
| RSF | Conceptualization, Final manuscript approval, Supervision, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing. |
Corresponding author: Antoninho José Tonatto-Filho, Rua Ubaldino do Amaral nº 124, ap 701, Bairro Alto da Gloria, Curitiba, PR, Brasil Zip Code 80060-190, E-mail: aj.tonatto@gmail.com
Article received: May 17, 2020.
Article accepted: December 13, 2021.
Conflicts of interest: none.











 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter