

Original Article - Year 2022 - Volume 37 -
Intramuscular plane for breast augmentation with a silicone implant
Plano intramuscular para mamoplastia de aumento com implante de silicone
ABSTRACT
Introduction: Breast augmentation is a frequent aesthetic procedure in plastic surgery; the ideal plane has not yet been found. Each pocket has its indication, its advantages, and disadvantages. The intramuscular pocket technique was initially described for use in buttock augmentation surgeries with silicone implants, and later its safety was reinforced with the use of the XYZ method. This study aims to present the use of the intramuscular technique in breast augmentation with a silicone implant.
Methods: This study describes the intramuscular pocket technique in breast augmentation with a silicone implant used in 50 female patients.
Results: The intramuscular technique provides a good definition of aesthetic contour in the medial quadrants of the breasts. We had a case of seroma in the postoperative period caused by a technical error in separating the fascicles.
Conclusion: The technique is safe and has a low incidence of complications.
Keywords: Breast implant; Mammoplasty; Seroma; Implant capsular contracture Surgical flaps.
RESUMO
Introdução: O aumento mamário é um procedimento estético frequente na cirurgia plástica, o plano ideal ainda não foi encontrado. Cada loja tem sua indicação, suas vantagens e desvantagens. A técnica da loja intramuscular foi inicialmente descrita para uso em cirurgias de aumento dos glúteos com implantes de silicone, e mais tarde sua segurança foi reforçada com a utilização do método XYZ. O estudo tem a finalidade de apresentar a utilização da técnica intramuscular na mamoplastia de aumento com implante de silicone.
Métodos: Este estudo descreve em detalhes a técnica da loja intramuscular na mamoplastia de aumento com implante de silicone, utilizada em 50 pacientes do sexo feminino.
Resultados: A técnica intramuscular propicia uma boa definição de contorno estético nos quadrantes mediais das mamas. Tivemos um caso de seroma no pós-operatório, causado por erro técnico na separação dos fascículos.
Conclusão: A técnica é segura e apresenta baixa incidência de complicações.
Palavras-chave: Implante mamário; Mamoplastia; Seroma; Contratura capsular em implantes; Retalhos cirúrgicos
INTRODUCTION
Breast augmentation with silicone implants is a common aesthetic procedure in plastic surgery. The ideal plane to house the implants has not yet been found. Clinical inspection and physical examination of the breasts in the preoperative period and the choice of technique for each patient are fundamental determinants for obtaining excellent results, excluding the concept of a universal technique for treating all types of breasts.
Five breast implant pocket locations are used in breast augmentation: (1) Subglandular, (2) Subfascial, (3) Retromuscular (retropectoral, total submuscular, dual plane).
Each pocket has its indication, its benefits and its complications. In an attempt to reduce the incidence of capsular contracture, breast atrophy, seroma, implant visibility and palpability, the pockets became deeper, the implants less palpable, and the breasts with the most natural appearance (Chart 1).
| Breast plane | Complications | Benefits |
|---|---|---|
| Subglandular | 1. Capsular contracture. 2. Rippling. 3. Short and medium-term atrophy of the mammary gland. 4. Skin distension. 5. Earlier ptosis. 6. Improved visibility and palpability of implant edges. 7. Artificial appearance. |
Shorter surgical time. Greater control of bleeding. Greater control of the definition of the submammary fold. Greater control of breast shape. Faster postoperative recovery. Minimal animation with chest contraction. Periprosthetic capsule distant from the rib cage. |
| Subfascial | 1. Rippling and capsular contracture with an intermediate incidence in relation to the subglandular and retromuscular planes. | 1. Good tissue coverage of the prosthesis. 2. Periprosthetic capsule distant from the rib cage. 3. Contours in the medial quadrants with great definition. |
| Retromuscular: (Dual Plane, retropectoral and total submuscular) | 1. Implant displacement above the second intercostal space. 2. Wide pocket. 3. Capsule adhered to the rib cage. 4. Blindspot in the second intercostal space. 5. Extreme difficulty in total capsulectomy. 6. Greater animation with muscle contraction. |
1. Excellent implant coverage in the upper and medial quadrants. 2. Lower incidence of capsular contracture and rippling. 3. Naturalness of shape and contour. 4. Shorter surgical time. 5. Lesser glandular atrophy in the short and medium-term. |
| Intramuscular | 1. A case of seroma caused by excess muscle debris. 2. Less muscle coverage when compared to the retromuscular plane. 3. Longer surgical time. |
1. Periprosthetic capsule distant and free from the rib cage. 2. Intermediate coverage between the retromuscular and subfascial planes. 3. Less animation with muscle contraction (videos 1A e 1B). 4. Stability in implant positioning with less displacement. |
Source: Author (2019).
Contour beauty in the medial quadrants in the subfascial plane is slightly less in the retromuscular plane. On the other hand, the richness of coverage in the retromuscular plane reduces the incidence of rippling and presents less glandular atrophy than the subfascial and subglandular planes1,2.
Considering the anatomical principles of irrigation and innervation of the pectoralis major muscle (PMM), we concluded that it was feasible to use the intramuscular plane in breast augmentation.
The intramuscular technique for gluteal implant was published by Vergara & Marcos3 in 1996; Gonzalez described the XYZ4 technique, increasing the degree of safety in performing the procedure.
This work aims to present the use of the intramuscular plane in breast augmentation with silicone implants in thin patients who need a deep pocket.
OBJECTIVE
This work aims to present the new use of the intramuscular plane in breast augmentation with silicone implants.
METHODS
Casuistry
This is a primary and retrospective study of 50 female patients, aged between 19 and 55 years, who underwent augmentation mammaplasty with silicone implants in the intramuscular plane, from December 2018 to April 2020, carried out in the Camillo Plastic and Reconstructive Surgery Clinic in the city of Toledo, PR. After explaining the risks and benefits of the technique, the patients signed informed consent. This article was approved by the Research Ethics Committee (Centro Universitário Assis Gurgacz - CAAE 35340220.1.0000.5219).
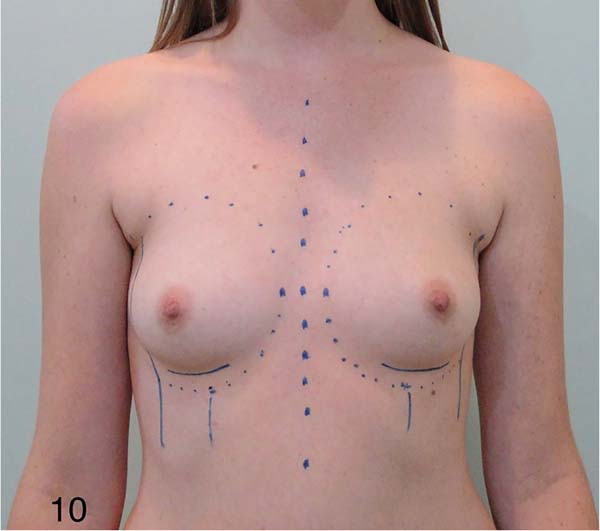
All patients were referred for laboratory evaluations, breast ultrasound, mammography in specific cases and anesthetic and cardiological evaluations. We guide physical activity for mild PMM hypertrophy in the preoperative period. The study followed the Helsinki principles.
Surgical technique
Patients underwent intravenous anesthesia and intercostal block, antibiotic prophylaxis, aseptic and antisepsis care, and minimal manipulation of the implants.
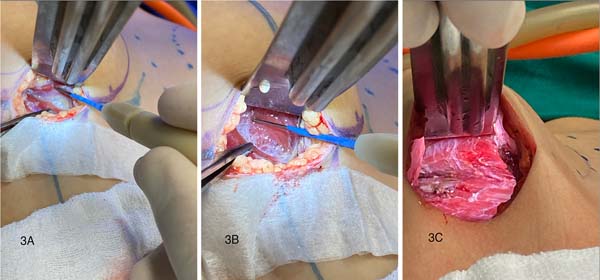
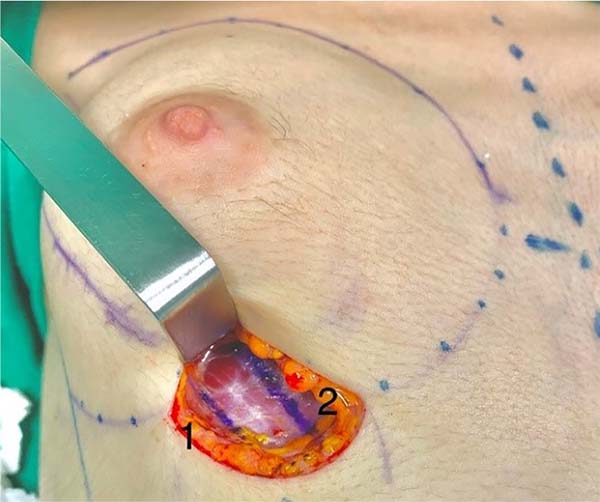
Through a 4.5 cm incision in the submammary crease, with the ends of the incision equidistant from the breast midline, the adjacent topographic surface of the pectoralis major muscle is located. In a parallel line and 2 cm medial to the lateral edge of the pectoralis major muscle, a 4 cm incision is made in the pectoral fascia, starting at the fifth intercostal space (Figure 1).
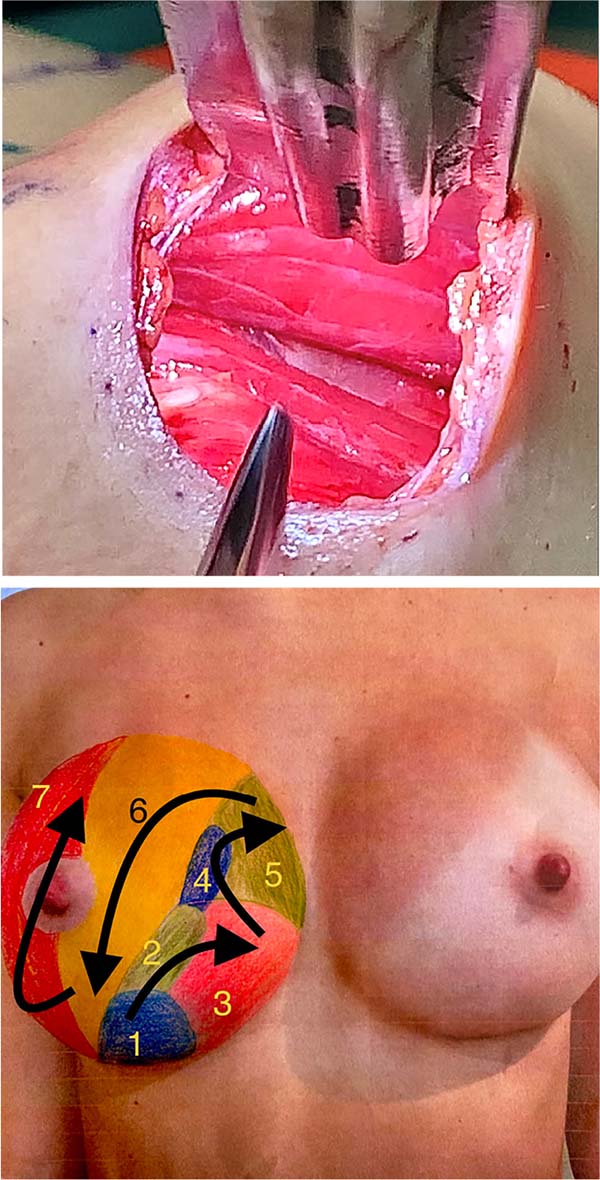
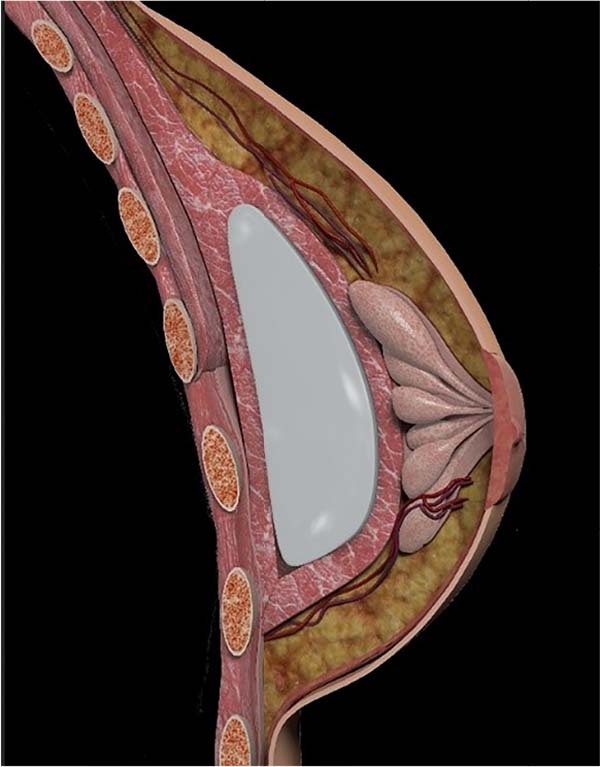
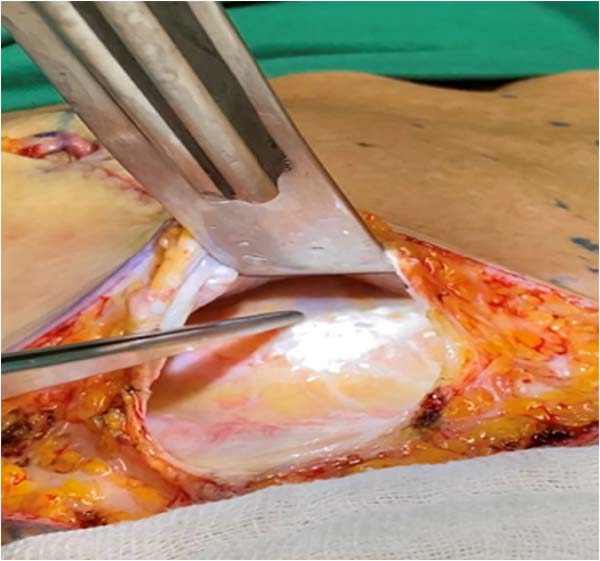
It penetrates the interior of the muscle, and the muscle fascicles are separated through the release of the perimysium (electric scalpel in cutting function, colored tip) throughout the area of the internal projection of the peripheral limits of the pocket previously demarcated on the breast skin (footprint). The deeper fascicles, when separated, are attached to the posterior layer of the deep pectoral fascia5 (Figure 2). When the separation is finished, we will have the division of the muscle in its thickness, forming two flaps, the anterior muscle flap (roof of the pocket) and the posterior muscle flap (floor of the pocket).

The mean thickness of the anterior flap on operated patients varies according to its location and degree of muscle hypertrophy. In the lower quadrants, its smallest thickness is found on the sixth rib (0.35 cm) and gains body, with the sum of new fascicles that originate on the anterior surface of the sternum, approximately 0.5 cm thick on the fifth rib, 0.75 cm over the fourth, 1.25 cm over the third, and 1.5 to 2 cm over the second rib.
The posterior flap originates from the chondral processes of the second to seventh ribs. Its thickness is fixed, approximately 0.3 to 0.5 cm, because the fascicles of each chondral process are juxtaposed and do not overlap. The decision-making process in defining the thickness of the flaps is the correct separation of the fascicles, finding the cleavage plane between the two laminae of the PMM, which is anatomically determined at its origins (posterior flap with fascicles originating from the chondral processes and anterior flap with the fascicles originating on the anterior surface of the sternum).
We ask that the patient do physical activity for 30 to 60 days, aiming to hypertrophy the pectoralis major muscle. We did not perform the synthesis of the pectoralis major muscle in the area of access to the intramuscular plane since the volumes placed are modest, respect the dimensions of each thorax, and are accommodated inside the pocket without causing bulges on the area of the muscle incision.
The upper limit of the pocket is located at the transition between the third rib and the second intercostal space. In this location, the fascicles of the pectoralis major muscle are in a position transverse to the thorax, with fibrous septa that adhere to each other, which make their separation difficult, presenting themselves as a compact and insurmountable muscle mass, which will favor the creation of a pocket with defined limits and stable in the upper quadrants, not allowing the prosthesis to ascend (Figures 3, 4A and 4B). The pedicle of the posterior flap is the thoracoacromial artery, and the pedicle of the anterior flap is formed by the perforating branches of the intercostal arteries6.
The pocket limit in the medial quadrants is 1 cm short of the conventional pre-marking of pocket dimensions on the breast skin.
The limit of the pocket in the lateral quadrants is defined by a 2-cm-wide muscular tape of the PMM, with its costal and abdominal origins preserved, together with part of the fascia covering the serratus anteroinferior muscle, which will support the prosthesis, providing support and support avoiding lateral sliding, especially in a cylindrical chest7,8. The muscular tape is reinforced by fascicles of the posterior flap, at the level of the union of the lateral quadrants, which are positioned on the lateral wall of the pocket, increasing the stabilization function and decreasing the lateral displacement. Implant stability in the pocket is inversely proportional to implant volume.
Another prevention method used to prevent displacement of the prosthesis below the submammary fold (bottoming out) is suturing at the level of the submammary fold between the deep layer of subcutaneous fascia (equivalent to Scarpa’s fascia in the abdomen) with the anterior layer of fascia pectoralis deep (equivalent to the Innominate fascia in the abdomen), eliminating the fascial cleft through which the implant slides down, crossing the submammary fold. It is important to mention that this stabilization is efficient only when the choice of implant base is defined, taking into account the measurements of the hemithorax (anterior axillary line - lateral border of the sternum), minus 2 centimeters. Therefore, we will use low-volume implants with predefined bases; large volumes distend the entire musculature, causing implant displacement.
It is believed that the vigorous muscle contraction and muscle tone of the anterior flap of the PMM on the implant causes a slight rise of the same (1 to 2 centimeters); therefore, in some situations, we can use this observation in our favor, in other situations we must avoid it. Therefore, in patients in the orthostatic position who present a measurement of the height from the nipple to the submammary crease (measurement made with a caliper, different from the measurement of skin extension under light traction of the same, using a tape measure) between 5.0 and 5.5 cm we make a muscle relaxation incision in the anterior portion of the PMM flap9, “envelope flap technique,” located at the level of the nipple projection, preventing the implant from ascending10,11.
In patients who present a measurement of the height from the nipple to the submammary fold equal to or above 6 centimeters, we do not make a muscle relaxation incision, waiting for slight traction of the muscle on the prosthesis to position the prosthesis 1 cm above the submammary fold and maintain the center of the prosthesis under the nipple-areolar complex. We will not have that long bottom pole and an empty lap. In patients with the measurement of the height between the nipple and the submammary crease less than or equal to 4.5 centimeters, or in constricted breasts, we perform the muscle dieresis 1 centimeter above its costochondral origin (in these cases, the muscle origin is high, fifth or fourth rib), in the anterior portion of the PMM flap, and we created a neosulcus more inferiorly (Videos 1A a 1K).
We will have a pocket lined by muscle fascicles of the PPM on its anterior and posterior surfaces, which is why we cannot visualize the ribs during the entire transoperative period (Figure 5).
RESULTS
Round and super high-profile implants were used in 8 cases (16%), and the high-profile was used in 42 cases (84%).
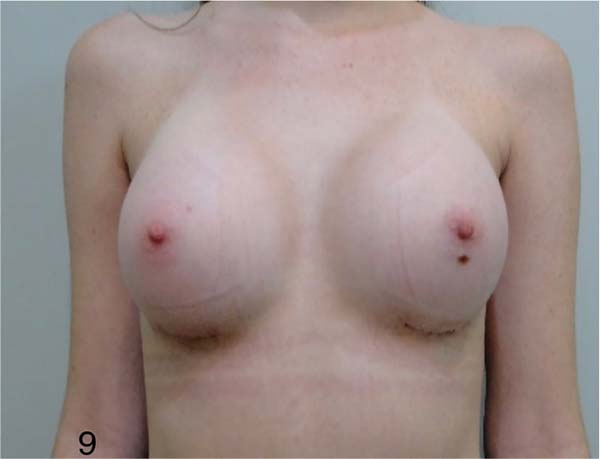
Implant volumes ranged from 250 cc to 410 cc (mean 300 cc). All surgeries were primary augmentation. The association with other surgeries occurred in 8 cases (16%), being 5 cases of rhinoplasty (10%), 2 cases of blepharoplasty (4%), and 1 case of periareolar skin removal for repositioning of the nipple-areolar complex (2%).
One patient had a late unilateral seroma (2%), with a slow and progressive onset, which became clinically evident on the 90th postoperative day, and was confirmed by breast ultrasound. The patient underwent a surgical reintervention, and we observed the presence of muscle debris inside the pocket, probably caused by a technical error in the separation of the fascicles. The procedure adopted was to change the implant and clean the pocket with a 10% polyvidone-iodine degerming solution and a solution containing antibiotics.
Another case of surgical reintervention was in a patient who presented residual ptosis (2%) one year after augmentation mammoplasty associated with periareolar skin resection, requiring mastopexy with a resulting inverted T scar. In cases of surgical reintervention, we observed that the posterior flap of the PMM presented normal color and preserved contraction function when stimulated; the distance between the posterior capsule of the pocket and the rib cage was 6 millimeters (Video 3).
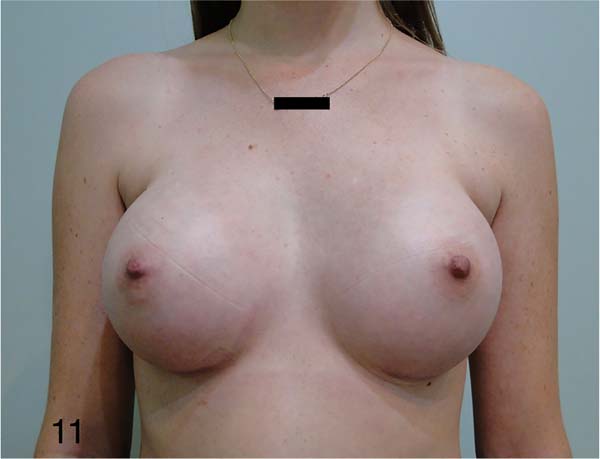
Aesthetically, the breasts present good contour definition in the medial quadrants. The patients report being satisfied with the results (92%), four patients report a small asymmetry at the height of the breasts (8%). Preoperatively, these patients’ differences in the implantation height of the breasts on the chest were identified and noted on their consultation records, with an evident gap in the height of the submammary folds and the height of the nipple-areolar complexes (Figures 6 to 11).
Surgical time increased by 30 minutes when compared to the retromuscular plane. We have not yet had complications such as hematoma and capsular contracture. We need a greater number of cases and a longer follow-up time.
DISCUSSION
The intramuscular plane is a deep plane with additional muscle coverage over the implant. Its floor is formed by the posterior flap, with approximately 0.3 to 0.5 centimeters in thickness of the PMM, located between the posterior capsule of the pocket and the rib cage. This floor increases the distance and decreases the adhesion between the posterior capsule of the pocket and the rib cage, offering safety and technical ease in performing the posterior capsulectomy (Figure 12).
The pocket is fair in its dimensions, the transverse fascicles of the PMM at the level of the third rib form the upper limit of the pocket, a physical barrier to the cranial migration of the implant (Figure 13). The intramuscular technique, in relation to the thickness of the implant’s coverage, can be compared to the hybrid technique, in which the implant is placed in a subfascial plane and fat is grafted in specific areas of the peripheral contour of the breasts (the anterior flap of the PMM would correspond to fat graft).
In the future, we will observe the degree of muscle atrophy of the flaps during reinterventions with precise indications. So far, we know that there was no muscle atrophy in the first postoperative year. The intramuscular technique, in relation to access to the pocket, through the PMM, and the stabilization mechanisms used with smooth implants (lateral tape of the PMM and fascia of the serratus anteroinferior), is very similar to the SMS technique - Splitting Muscle Support, idealized by Khan12-14. A modification of the SMS technique was proposed by Rigo et al.15, which classifies the support of the PMM and anterior serratus fascia in SMS-1,2,3 levels, used according to the specifications of each breast. In the intramuscular plane, the posterior flap prevents the implant from causing friction on the periosteum and perichondrium of the ribs, so the sensory stimuli are smaller.
The fascicles with chondral origin form the floor of the pocket (posterior flap); therefore, the barrier formed by the chondral origins of the PMM (pinnate), described by Tebbets16, is posterior to the intramuscular plane, with greater medialization of the implant, with the new limit medial muscle located at the ventral origin of the sternum.
In the retromuscular plane, the PMM is moved away from the ribs, which favors the formation of a posterior capsule that is close and adhered to the rib cage, especially at the costochondral junctions of the second to fifth ribs (Figure 14). The retromuscular plane is inside a fascial cleft, a virtual space between two fasciae formed by loose connective tissue, which does not offer resistance to tissue separation.
At the time of making the retromuscular pocket, the only points of resistance to dissection coincide with the costal and sternal origins of the PMM, therefore, during the introduction of the implant and in the first changes in the patient’s position in the immediate postoperative period, no matter how tight the pocket has been planned, there will, in some cases, be an enlargement of the pocket dimensions, and the superior and lateral displacement of the implant may occur.
Thus, the subfascial plane would be our first option in patients with a pinch test greater than or equal to 2 cm in the superomedial quadrant of the breasts, and the intramuscular plane would be the first option in thin patients with a pinch test less than 2 cm. In patients with extremely thin muscles, separating the flaps becomes impossible; the retromuscular plane is better indicated in these cases.
CONCLUSION
The intramuscular technique in breast augmentation is a safe, reproducible and technically easy procedure, with a low rate of complications.
REFERENCES
1. Tebbetts JB. Dual plane breast augmentation: optimizing implant-soft-tissue relationships in a wide range of breast types. Plast Reconstr Surg. 2006;118(7 Suppl):81S-98S.
2. Graf RM, Bernardes A, Rippel R, Araujo LR, Damasio RC, Auersvald A. Subfascial breast implant: a new procedure. Plast Reconstr Surg. 2003;111(2):904-8.
3. Vergara R, Marcos M. Intramuscular gluteal implants. Aesthetic Plast Surg. 1996;20(3):259-62.
4. Gonzales R. Augmentation gluteoplasty: the XYZ method. Aesthetic Plast Surg. 2004;28(6):417-25.
5. Goss CM, ed. Anatomy of the Human Body by Henry Gray. 29th ed. Philadelphia: Lea & Ferbiger; 1997.
6. Bongiolo Junior M, Santos DN, Bittencourt RC, Pintarelli G, Joeziorowski A, Nunes E. Uso de retalho do músculo peitoral maior para o tratamento de osteomielite de esterno. Rev Bras Cir Plást. 2010;25(3 Suppl. 1):67.
7. Ono MT, Karner BM. Four-step Augmentation Mastopexy: Lift and Augmentation at Single Time (LAST). Plast Reconstr Surg Glob Open. 2019;7(11):e2523.
8. Procópio LD, Silva DDP, Rosique R. Implante submuscular em duplo bolso para mastopexia de aumento. Rev Bras Cir Plást. 2019;34(2):187-95.
9. Leão CEG. Mamoplastia de aumento: “técnica em aba de envelope”. Rev Bras Cir Plast. 2009;24(2):202-7.
10. Sper SL, Schwartz J, Dayan JH, Clemens MW. Outcome assessment of breast distortion following submuscular breast augmentation. Aesthetic Plast Surg. 2009;33(1):44-8.
11. Pelle-Ceravolo M, Dell Vescovo A, Bertozzi E, Molinari P. A technique to decrease breast shape deformity during Muscle contraction in submuscular augmentation mammaplasty. Aesthetic Plast Surg. 2004;28(5):288-94.
12. Khan UD. Muscle-splitting breast augmentation: a new pocket in a different plane. Aesthetic Plast Surg. 2007;31(5):553-8.
13. Khan UD. Multiplane technique for simultaneous submuscular breast augmentation and internal glandulopexy using inframammary crease in selected patients with early ptosis. Eur J Plast Surg. 2011;34(5):337-43.
14. Khan UD. Revisionary Surgery Following Primary Augmentation Mammoplasty in Muscle Splitting Biplane Pocket: An Appraisal of 93 Revisionary Surgeries. Aesthetic Plast Surg. 2021;45(2):462-71.
15. Rigo MH, Piccinini PS, Sartori LDP, de Carvalho LAR, Uebel CO. MS-Split Muscle Support: A Reproducible Approach for Breast Implant Stabilization. Aesthetic Plast Surg. 2020;44(3):698-705. DOI: 10.10071500266-019-01565-5
16. Tebbets JB. Augmentation Mammaplasty - Redefining the Patient and Surgeon Experience. 1st ed. Maryland Heights: Mosby/Elsevier; 2010.
1. Clinic of Plastic and Reconstructive Surgery Camillo, Toledo, PR, Brazil.
| COLLABORATIONS | |
|---|---|
| FCC | Analysis and/or data interpretation, Conception and design study, Conceptualization, Data Curation, Final manuscript approval, Formal Analysis, Funding Acquisition, Investigation, Methodology, Project Administration, Realization of operations and/or trials, Resources, Software, Supervision, Validation, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing |
Corresponding author: Francisco Carlos Camillo, Rua Independência 2586, Toledo, PR, Brazil, Zip Code 85902015, E-mail: franciscocarloscamillo@gmail.com
Article received: February 26, 2021.
Article accepted: July 16, 2021.
Conflicts of interest: none.




























 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter