

Case Report - Year 2021 - Volume 36 -
Skin coverage of the anterior region of the knee with an anterolateral reverse flow thigh flap based on the perforating artery of the transverse branch of the lateral femoral circumflex artery: a case report
Cobertura cutânea da região anterior do joelho com retalho anterolateral da coxa de fluxo reverso, baseado na artéria perfurante do ramo transverso da artéria circunflexa femoral lateral: relato de caso
ABSTRACT
The patella is an uncommon place for the appearance of bone tumors, benign or malignant, and pseudotumoral lesions. In the literature, there is a small amount of work on this topic. This case report is about a patient with a metastatic tumor in the patella and reconstruction of the deformity with an anterolateral reverse flow thigh flap. Skin and soft tissue reconstruction in the region around the knee are often challenging for the plastic surgeon and aim to cover the exposed bone, preserving the joint function of the knee and providing a good esthetic result. There is an option for the use of free flaps, where there is a need for adequate material and trained staff. However, the vascular anastomosis region at the back of the knee makes the procedure even more complex. The anterolateral reverse thigh fasciocutaneous flap, first described in 1990 by Zhang et al., appears to be an effective and reliable option for reconstructing defects around the knee. It has a long vascular pedicle length and the availability of soft parts. There are some anatomical variations in which the cutaneous perforator does not originate from the descending branch. This report presents a patient with a skin perforator originating from the transverse branch of the lateral femoral circumflex artery, with an acceptable aesthetic result for skin coverage in the anterior region of the knee.
Keywords: Perforator flap; Lower end; Surgical flaps; Reconstructive surgical procedures; Plastic surgery; Case reports.
RESUMO
A patela é um local infrequente para o aparecimento de tumores ósseos, benignos ou malignos, assim como de lesões pseudotumorais. Na literatura existe uma quantidade pequena de trabalhos sobre esse tema. Esse relato de caso trata-se de uma paciente com tumor metastático em patela e reconstrução da deformidade com retalho anterolateral da coxa de fluxo reverso. A reconstrução cutânea e de tecidos moles na região ao redor do joelho é frequentemente desafiadora para o cirurgião plástico e tem como objetivo cobrir a parte óssea exposta, preservando a função articular do joelho e conferir um bom resultado estético. Existe a opção pela utilização de retalhos livres, onde há necessidade de material adequado e equipe treinada. Contudo, a região de anastomose vascular na parte posterior do joelho torna o procedimento ainda mais complexo. O retalho fasciocutâneo anterolateral da coxa reverso, descrito pela primeira vez em 1990, por Zhang et al., parece ser uma opção efetiva e confiável na reconstrução de defeitos ao redor do joelho, haja visto que possui um longo comprimento do pedículo vascular e disponibilidade de partes moles. Existem algumas variações anatômicas em que a perfurante cutânea não se origina do ramo descendente. Esse relato traz uma paciente com perfurante cutânea oriunda do ramo transverso da artéria circunflexa femoral lateral com resultado estético aceitável para cobertura cutânea em região anterior do joelho.
Palavras-chave: Retalho perfurante; Extremidade inferior; Retalhos cirúrgicos; Procedimentos cirúrgicos reconstrutivos; Cirurgia plástica; Relatos de casos.
INTRODUCTION
Soft tissue reconstruction of the knee and the areas adjacent to it has always been a challenging procedure. In addition to post-traumatic defects, soft tissue defects in the knee area can be caused by chronic infections, actinic lesions, or surgeries for lysis of the wounds due to burns1. The knee joint is a hinge type, mainly performing flexion and extension movements of the leg and with minimal rotation2. Reconstruction is a challenge for surgeons, having seen the need for flaps to be effective not only for coverage but also for thin enough not to impair mobility after recovery2.
Sometimes these injuries are caused by resections of bone tumors in the distal femur, patella, and proximal tibia. The patella is an uncommon site for the appearance of bone tumors, benign or malignant, and pseudotumoral lesions. In the literature, there is a small amount of work on this topic3. Most tumors are benign, with a significant incidence of giant cell tumors and chondroblastomas4. The most frequent malignant tumor is hemangioendothelioma, followed by lymphoma and osteosarcoma3.
This case report is about a patient with a metastatic tumor in the patella and reconstruction of the deformity with an anterolateral reverse flow thigh flap. In the literature, there are reports of giving up surgical planning when the main perforator of the flap does not originate from the descending branch of the lateral circumflex femoral artery (LCFA)5. However, this work aims to show that, given this anatomical change, the making of the flap does not necessarily need to be discarded.
OBJECTIVE
General
Show and discuss lower limb reconstruction based on an anterolateral reverse flow thigh flap with acceptable aesthetic results for skin coverage in the anterior region of the knee.
Ethical aspects
The present case report follows the declaration of Helsinki. The patient was given an informed consent form (ICF). The patient was consulted about using her clinical data from medical records and photographs of the surgical procedure to prepare this case report.
CASE REPORT
The case comes from the Pernambuco Cancer Hospital (HCP). Patient JFS, 39 years old, female, brown, rural worker, born in and coming from Calumbi/PE, presented an expansive formation, measuring 5.2x3.3 cm, located in the patellar region of the left knee (Figure 1). She showed clinical pain, local edema and limited limb flexion. The onset of symptoms in May 2019. As a background, she reported right nephrectomy in 2015 due to a renal tumor and histopathological examination compatible with clear cell carcinoma.
The first diagnostic hypothesis raised by the orthopedics team was the possibility that it was a benign soft tissue tumor, probably a chondroblastoma. However, magnetic resonance imaging of the left knee showed solid expansive formation in the left patella, predominantly in its centromedial region, measuring 5.2x3.3x2.9 cm, with discontinuity of the bone cortical and soft tissue component. In addition, an expansive formation with the same characteristics was also noted on the anterior margin of the medial tibial plateau, measuring 1.9x0.6cm (Figure 2).
Surgical planning performed in conjunction with plastic surgery included total resection of the patella in a bloc with the soft parts of the anterior region of the knee and curettage of the tibial plateau region. The plastic surgery initially planned reconstruction with a medial gastrocnemius flap, in case it was a small to moderate defect, and anterolateral reverse flow thigh flap or free flap in the case of a large size. However, no imaging study was carried out to evaluate vascular irrigation of the knee or the distal region of the thigh before surgery.
The plastic surgery team consisted of a plastic surgeon specializing in microsurgery, a resident in the last year of plastic surgery, and another in the second year. There was a possibility of microsurgical reconstruction; therefore, the microscope was on stand-by in the operating room; however, it was not used for reconstruction.

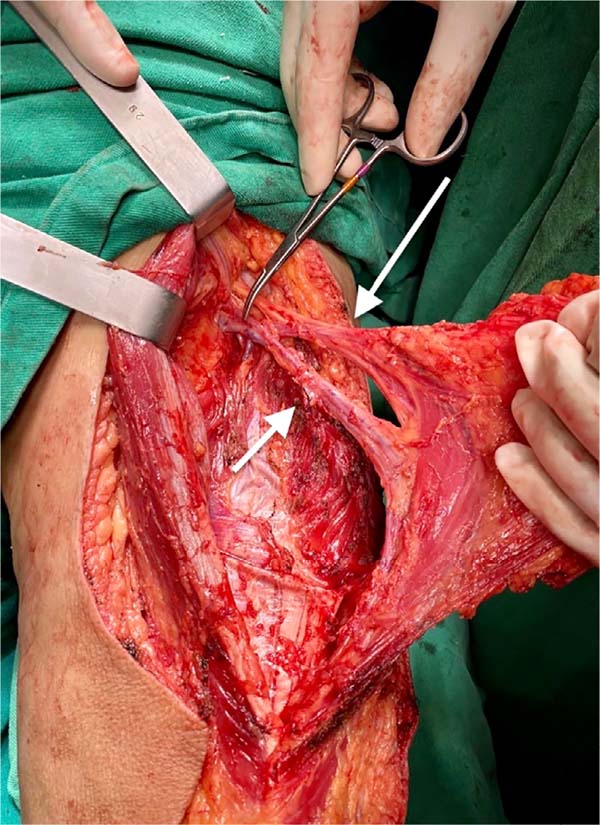
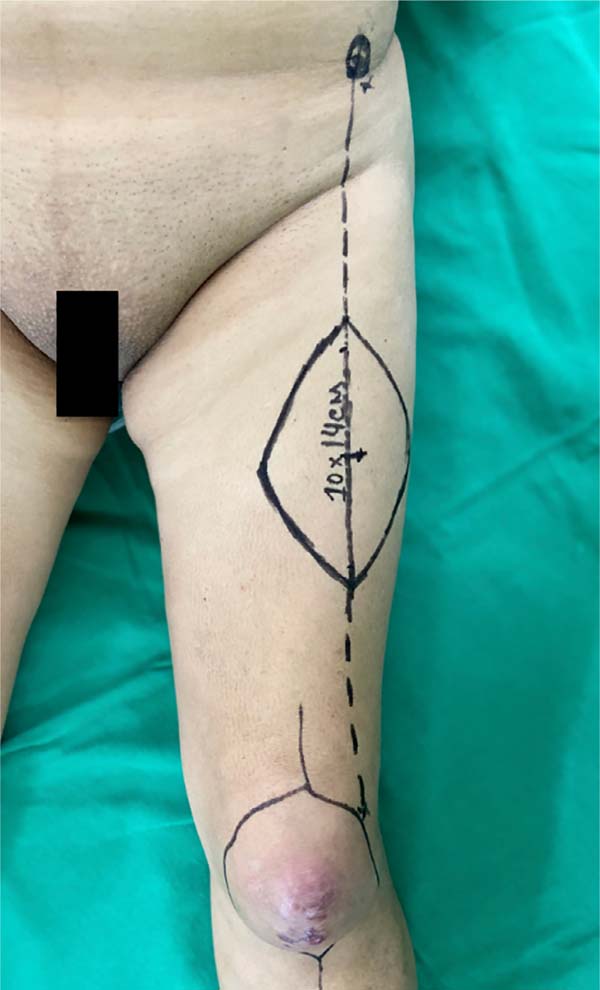
The orthopedics team operated on the patient with bone and soft tissue resection involving the regions of the patella and the distal medial fragment of the tibia (Figure 3). The reconstruction proposed by the plastic surgery team was an anterolateral reverse flow thigh flap measuring 14x10cm (Figure 4). In the perioperative period, it was observed that it was a type II flap since the main perforator of the flap did not originate from the descending branch but from the transverse branch of the LCFA5. This finding required that the dissection reach the LCFA trunk to include the main cutaneous perforator in the flap (Figure 5). Clamping was performed above the bifurcation of the descending and transverse branches with a 6cm bulldog vascular clamp to test for reverse flow patency. After certification of the flap vascularization through reverse flow, double ligation of the vessels was performed with 3-0 cotton thread and flap rotation (Figures 6 and 7). The donor area was partially closed, with an approximation of the edges using a 3-0 nylon thread and healing by third intention and subsequent skin grafting. A muscle layer protected the pedicle from the rectus femoris along its entire length. The procedure was performed under spinal anesthesia for a total of 2.5 hours (Figure 8) with an acceptable esthetic result (Figure 8 - B).
Protection was performed in the donor area with a silver foam dressing. Immobilization was performed with a plaster splint to prevent knee flexion. The primary dressing was changed daily. The patient was instructed not to walk in the first 72 hours and underwent deep vein thrombosis prophylaxis with 40mg of enoxaparin. After the first 72 hours, we advise walking with a full-length limb and protection with a plastered splint. The patient was discharged on the seventh day after surgery, with no complications during this period.

The pathology results coincided with that of the previous biopsy, resulting in clear cell carcinoma.
The patient returned to the outpatient clinic on the fifteenth and thirtieth day after surgery, showing satisfaction with the esthetic result. She also had a slight flexion of the knee. However, having performed resection of the patella and the entire knee stabilizing mechanism evolved with joint instability. Finally, however, she was able to walk with the aid of auxiliary walking devices.
DISCUSSION
Skin and soft tissue reconstruction in the region around the knee are often challenging for the plastic surgeon and aim to cover the exposed bone, preserving the joint function of the knee and providing a good esthetic result. There is an option for the use of free flaps, where there is a need for adequate material and trained staff. However, the vascular anastomosis region at the back of the knee makes the procedure even more complex. The reverse anterolateral fasciocutaneous flap of the thigh, first described in 1990 by Zhang et al.6, seems to be an effective and reliable option in the reconstruction of defects around the knee, given that it has a long vascular pedicle length and availability of soft parts7,8. The vascular base of this flap is the anastomosis between the descending branch of the LCFA and the lateral superior genicular artery (LSGA), which is located about 3 to 10 cm above the lateral edge of the patella. This connection maintains constant skin perfusion through retrograde blood flow, sufficient for the flap’s survival5. However, there are some anatomical variations in which the cutaneous perforator does not originate from the descending branch2.
In the literature, there are reports of giving up surgical planning when the main perforator of the flap does not originate from the descending branch of the LCFA5. In the case reported here, the planning was maintained, considering the good perfusion after clamping, above the bifurcation, between the descending and transverse branches. Some points should be considered for a good outcome: the non-compression and maintenance of a muscle layer around the pedicle and the confirmation of flow with vascular clamping.
CONCLUSION
Based on the perforator in the transverse branch of the LCFA, the reverse flow anterolateral thigh flap proved to be a good option, fast and with an acceptable aesthetic result for skin coverage in the anterior region of the knee.
REFERENCES
1. Gravvanis A, Kyriakopoulos A, Kateros K, Tsoutsos D. Flap reconstruction of the knee: a review of current concepts and a proposed algorithm. World J Orthop. 2014 Nov;5(5):603-13.
2. Song M, Zhang Z, Wu Y, Ma K, Lu M. Primary tumors of the patella. World J Surg Onc. 2015 Abr;13:163.
3. Bapista AM, Sargentini SC, Zumárraga JP, Camargo AF, Camargo OP. Tumores da patela: a experiência do instituto de ortopedia e traumatologia da Universidade de São Paulo. Acta Ortopéd Bras. 2016;24(3):151-4.
4. Bharathi RR, Ramkumar S, Venkatramani H. Soft tissue coverage for defects around the knee joint. Indian J Plast Surg. 2019 Jan;52(1):125-33.
5. Demirseren ME, Efendioglu K, Demiralp CO, Kilicarslan K, Akkaya H. Clinical experience with a reverse-flow anterolateral thigh perforator flap for the reconstruction of soft-tissue defects of the knee and proximal lower leg. J Plast Reconstr Aesthet Surg. 2011 Dez;64(12):1613-20.
6. Zhang G, et al. Reversed anterolateral thigh island flap and myocutaneous flap transplantation. Zhonghua Yi Xue Za Zhi. 1990 Dez;70(2):676-8.
7. Guataçara Junior SS, Freitas RS, Novais JR, Maschio AG, Paula DR, Marcante RFR, et al. Retalho anterolateral da coxa reverso: uma opção de reconstrução para os membros inferiores. Rev Bras Cir Plást. 2018;33(4):493-500.
8. Pan SC, Yu JC, Shieh SJ, Lee JW, Huang BM, Chiu HY. Distally based anterolateral thigh flap: an anatomic and clinical study. Plast Reconstr Surg. 2004 Dez;114(7):1768-75.
1. Hospital das Clínicas, Federal
University of Pernambuco, Recife, PE, Brazil.
2. Pernambuco Cancer Hospital, Recife, PE,
Brazil.
Corresponding author: Fábio Santiago de Macedo, Rua Hermogenes de Morais, 252, Apt 2901 - Madalena, Recife - PE, Brasil, Zip Code 50610-160, E-mail: fsdemacedo@gmail.com
Article received: June 08, 2020.
Article accepted: April 23, 2021.
Conflicts of interest: none.
Institution: Pernambuco Cancer Hospital, Recife, PE, Brazil.















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter