

Review Article - Year 2021 - Volume 36 -
Algorithms for the management of scars: the importance of systematizing behaviors
Algoritmos para manejo de cicatrizes: a importância da sistematização de condutas
ABSTRACT
Introduction: Pathological scars occur from the hyperproliferation of fibroblasts and can be classified into hypertrophic scars and keloids. Basically, hypertrophic scars do not grow beyond the limits of the original wound, while keloids grow horizontally in a nodular form. Despite the diversity of instruments used to guide the prevention, treatment and follow-up of pathological scars, there is a need for instruments that address local realities. The objective is to carry out a narrative review of the literature on scar management algorithms and create an updated algorithm.
Methods: Descriptive study of narrative literature review, with a search in PubMed, SciELO, LILACS, MEDLINE and Cochrane databases, from November 2010 to November 2020, published in English, Portuguese and Spanish. The descriptors used were: “cicatrix,” “keloid,” “algorithms,” and “wound healing.” The sample selection consisted of identifying the articles, reading the titles and abstracts, and selecting studies related to the topic. Subsequently, the full reading of the selected studies and classification according to the eligibility criteria were carried out. Results: 209 articles were found, and 116 were eliminated due to duplicity, resulting in 45 articles. A total of 8 articles that met the inclusion criteria were identified. Four articles were excluded after analysis and consensus meeting due to the absence of algorithms with scientific rigor; this study is composed of four articles.
Conclusion: Four algorithms were found in the literature review that resulted in the development of an updated algorithm for scars.
Keywords: Hypertrophic scar; Keloids; Algorithms; Skin abnormalities; Scar.
RESUMO
Introdução: As cicatrizes patológicas ocorrem a partir de hiperproliferaçãoo de fibroblastos, podendo ser classificadas em cicatrizes hipertróficas e queloides, basicamente as cicatrizes hipertróficas não crescem além dos limites da ferida original, enquanto os queloides crescem horizontalmente de forma nodular. Apesar da diversidade de instrumentos utilizados para orientar a prevenção, tratamento e seguimento de cicatrizes patológicas, existe a necessidade de instrumentos que contemplem realidades locais. O objetivo é realizar uma revisão narrativa de literatura sobre algoritmos para manejo de cicatrizes e criar um algoritmo atualizado.
Métodos: Estudo descritivo de revisão narrativa de literatura, sendo realizado uma pesquisa nas bases de dados PubMed, SciELO, LILACS, MEDLINE e Cochrane, no período de novembro de 2010 até novembro de 2020, publicados nos idiomas inglês, português e espanhol. Os descritores utilizados foram: “cicatrix”, “keloid”, “algorithms” e “wound healing”. A seleção da amostra consistiu da identificação dos artigos, leitura dos títulos e resumos e seleção de estudos relacionados ao tema e, posteriormente, foi realizada a leitura na íntegra dos estudos selecionados e classificação segundo os critérios de elegibilidade.
Resultados: Foram encontrados 209 artigos sendo eliminados 116 devido duplicidade resultando em 45 artigos. Foram identificados um total de 8 artigos que preencheram os critérios de inclusão e após análise e reunião de consenso foram excluídos quatro artigos devido à ausência de algoritmos com rigor científico sendo este estudo composto de quatro artigos.
Conclusão: Foram encontrados quatro algoritmos na revisão de literatura que resultaram na elaboração de um algoritmo atualizado para cicatrizes.
Palavras-chave: Cicatriz hipertrófica; Queloide; Algoritmos; Anormalidades da pele; Cicatriz.
INTRODUCTION
Skin lesions are repaired by the healing process, physiologically leading to scarring1. However, an anomalous healing process can lead to the formation of a pathological scar, causing aesthetic and functional repercussions.2. Didactically, pathological scars are classified as hypertrophic and keloid scars, phenotypic expressions of the same fibroproliferative disorder, with distinct clinical characteristics and etiopathogenesis, which also demand different therapeutic approaches3.
The challenge of managing pathological scars lies in the absence of a flowchart to guide conducts considered the gold standard, which respects practicality and reproducibility; as a result, patient management has historically been driven by personal clinical experience4. Based on this situation, we sought to establish a practical instrument to guide medical conduct in the management of pathological scars.
OBJECTIVES
Conduct an integrative literature review on algorithms for scar management and, in the end, propose an updated algorithm.
METHODS
This is a descriptive study of an integrative literature review looking for algorithms to guide actions regarding the prevention and treatment of pathological scars. The study was approved by the Federal University of São Paulo / Hospital São Paulo (UNIFESP/HSP)Research Ethics Committee nº 8030160120.
For the elaboration of this work, the following methodological proposal was followed: definition of the research question, data collection and organization, eligibility criteria, data analysis and statistical analysis. The PICo strategy was used to formulate the research question, with the letter “P” corresponding to ‘patient,’ “I” to ‘phenomenon of interest’ and “Co” to ‘context’6.
Given this concept, the following research question was elaborated: “Which instrument can more broadly guide the medical conduct for the management of pathological scars?”
A literature review was carried out through publications from November 2010 to November 2020. The search was carried out in the PubMed, SciELO, LILACS, MEDLINE and Cochrane databases. The terms used for the search were developed in three areas: hypertrophic scar, keloid, and treatment algorithms. The descriptors used were: “cicatrix,” “keloid,” “algorithms,” and “wound healing.”
The inclusion criteria for selecting articles were: a) publications in English, Spanish or Portuguese; b) articles that addressed the definition and pathophysiology of pathological healing; c) articles that presented flowcharts that guide the conducts for the prevention and treatment of pathological scars.
The non-inclusion criteria adopted were: a) expert opinions, case reports, comments, letters to the editor, works published in journal proceedings, clinical trial protocols, master’s and doctoral thesis; b) adolescent population; c) articles on the theoretical foundation of tissue healing, however, they do not cover the aspects of treatment.
Exclusion criteria were: articles that did not present organized algorithms for scar management.
Sample selection was performed in two steps. The first consisted of identifying the references and reading the titles and abstracts to finally select studies related to the topic. The second stage consisted of a full reading of the selected studies and classification according to the abovementioned criteria. A pair of examiners performed the steps.
To facilitate this process, the references were imported into the Rayyan QCRI software (https://rayyan.qcri.org/welcome)7, which helped the authors to streamline the initial screening of abstracts and titles in their reviews using a semi-automation process, in addition to allowing the sharing of information with other contributors.
RESULTS
The result of the search strategy used was transferred to the Rayyan QCRI software, which identified 164 duplicates among the 209 articles found, resulting in 45 articles, of which eight articles met the inclusion criteria, as shown in Chart 1.
| Database | Number of articles | Number of duplicate articles | Selected articles |
|---|---|---|---|
| PubMed/MEDLINE | 68 | 164 | 16 |
| LILACS | 31 | 4 | |
| SciELO | 28 | 2 | |
| Cochrane | 58 | 12 | |
| MEDLINE | 24 | 11 | |
| TOTAL | 209 | 164 | 45 |
| REFERENCE | OBJECTIVE | CONCLUSIONS |
|---|---|---|
| Ogawa R. 20108. | It presents an evidence-based review of previous articles and proposes algorithms for the treatment and prevention of hypertrophic scars and keloids. | The increase in randomized clinical trials in the last decade has greatly improved scar management, although these studies have several limitations. The currently available hypertrophic/keloid scar treatment algorithms will likely be significantly improved as our knowledge of scar biology progresses. |
| Kim S, et al. 20139. | Since the publication of a Recommendation clinic International on Scar Treatment in 2002, there have been numerous publications in scar treatment. Conduct a bibliographic search of abstracts, clinical trials, and meta-analyses evaluating scar prevention and treatment, and based on these data, formulate treatment recommendations for Asian patients. | Advances in understanding scar formation have also led to the introduction of new treatments and updated scar treatment recommendations benefiting clinicians who make evidence-based decisions about optimal treatment strategies for their patients. |
| Meaume S, et al. 201410. | Discuss key aspects of current guidelines that are relevant to dermatologists involved in scar treatment and assess the latest clinical evidence for the use of silicone therapy in which the guideline recommendations are based. | Silicone blades and gels are recommended as the current gold standard. These studies confirmed the efficacy and safety of silicone products for scar prevention and treatment. The practical advice presented in the guidelines Current measures should be combined with clinical judgment when deciding on the most effective scar management measures suitable for patients. |
| Gold MH, et al. 20143. | Provide evidence-based treatment algorithms relevant to a variety of clinical settings. | The prevention and treatment of pathological scars require individualized care, based on the principles of evidence-based medicine, and continues to evolve in line with technological and scientific. |
The selected articles were numbered from 1 to 8 and identified by title, main author and year of publication, were read in full by the pair of examiners. In the end, a consensus meeting was held where it was decided to exclude four articles from this group of 8 and maintenance of 4 articles for the composition of the study. The reason for the exclusion of 4 articles was the absence of algorithms with established scientific rigor, many of which corresponded to reports of personal experiences by their authors.
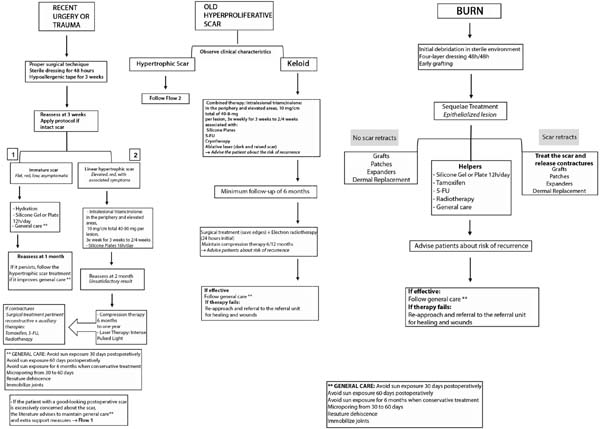
The articles’ descriptions are summarized in Chart 2. Based on the review carried out, the algorithm proposed by the authors is represented in Figure 1.
DISCUSSION
In the review performed, four algorithms were identified, which are those of Ogawa (2010)8, Kim et al. (2013)9 and Gold et al. (2014)3, which corresponds to an updated rereading of the instrument published by Mustoe et al. (2002)11. No national algorithms were found, so the protocol instrument described by Hochmann et al. (2018)12, which guides the conduct of the plastic surgery service at Federal University of São Paulo, Paulista School of Medicine (UNIFESP/EPM), was taken as a Brazilian reference for our analysis.
The “International Clinical Recommendation on Scar Management,” published by Mustoe et al. (2002)10, was the first instrument to contemplate an organizational chart for the management of scars, becoming a historic landmark. Considered a pioneer for reconciling simply and practically guidelines on the approach of pathological scars, including prophylactic measures in patients without classic risk factors, but with excessive concern regarding the scar from a surgical procedure, the instrument was updated by Gold et al. (2014)3 and still represents an important global reference for scar management.
In the algorithm by Ogawa (2010)8, the author makes the clinical differentiation between keloids and hypertrophic scars through classical characteristics, guides keloid treatments according to their extension and number of lesions, reaffirms the need for combined therapy and long follow-up. Concerning hypertrophic scars, the determining factor is the presence of contracture, which requires a surgical approach or conservative treatment. It reports the different forms of treatment of hypertrophic scars (surgery, compression therapy, silicone gel, corticosteroid, and laser) of keloid treatment (surgery, corticosteroid injections, cryotherapy, radiation, antitumor and immunosuppressive agents), emphasizing the importance of monitoring a long term of these patients.
The algorithm by Kim et al. (2013)9 stood out for addressing the management of scars focusing on the peculiarities of the skin of the Asian population, a pioneering approach since Ogawa (2010)8 and Mustoe et al. (2002)11 focused on Western and Afro-descendant people. Kim et al. (2013)9 reported that Asian skin has a thicker dermis, consequently increasing melanin and a greater number of sebaceous glands. This higher collagen density can result in hypertrophic scarring, causing prolonged erythema. All these differences were considered during the development of this flowchart. A point to emphasize is the importance given by Kim et al. (2013)9 the use of physical therapy tapping in pressure therapy in hypertrophic scars and the use of radiotherapy in the combined therapy of keloids, as well as, a fact that has been confirmed in more recent studies such as Calderón et al. (2020)13, who demonstrated that the exceptional surgical treatment of the keloid, followed by radiotherapy with electron beam did not result in recurrences in the excised area.
Meaume et al. (2014)10 conducted a review to update the main aspects of practical guidelines for the prevention and treatment of hypertrophic scars and keloids developed by an international and multidisciplinary group of experts, as well as exhaustively evaluating the most recent clinical evidence at the time for the use of silicone therapy on which the guideline recommendations are based. It was possible to make a practical and compact instrument for scar management; it is possible to infer that this is the first algorithm that values diagramming, using colors and shapes as mechanisms to draw attention to the content. It is a pioneer in preventive measures for pathological scars; it also brings as great news the insertion of botulinum toxin A in the therapeutic arsenal. Currently, studies such as the one by Carrero et al. (2019)14 have been increasingly accrediting the use of botulinum toxin A in healing, demonstrating its action under wound tension and fibroblast activity, optimizing the healing aspect.
In the study by Gold et al. (2014)3, the “International Advisory Panel on Scar Management” was convened to review the most current data available on methods of prevention and treatment of pathological scars, and thus review and update the instrument that was published by Mustoe et al. (2002)11.
Gold’s algorithm (2014)3 is more complete, although segmented. It addresses prevention and treatment, citing the conduct of scars with a good evolution in patients who demonstrate an excessive concern with their aesthetic aspect, a common fact in surgical patients, guiding in these cases the use of materials derived from silicone, in addition to conducting the microporation of the scar and emphasize the importance of proper surgical technique, has a technological focus.
Gold et al. (2014)3 highlight that using silicone plates and gels is the first choice in treating hypertrophic scars, reporting the use of micropore with hypoallergenic tape for patients at low-risk excessive concern with the appearance of a scar. An interesting point of this flowchart is to mention photoprotection to maintain the aesthetic appearance of scars, stressing that postoperative sun exposure worsens the clinical appearance of the scars. Thus, sunscreen was proposed to prevent negative outcomes for scars, acting as primary protection when the skin is exposed to direct sunlight.
No articles showed national algorithms on scars in the research carried out; however, the protocol flowchart by Hochmann et al. (2018)12 is used in the plastic surgery discipline at UNIFESP, having been used as the basis for this study. Although complex, divided into two parts, it details various procedures for scars (hypertrophic scars and keloids), including those arising from burns. This instrument prioritizes the content without a very strict demand on the layout.
After carrying out the review, it was possible to organize an updated algorithm addressing the management, from prevention to treatment, of pathological scars, demonstrating behavior clearly and objectively, considering scientific rigor, but also the form, facilitating its applicability and reproducibility in general medical practice, as shown in Figure 1.
CONCLUSION
The conduction of pathological scars is still challenging in the medical field due to several factors such as the large available therapeutic arsenal, lack of scientific rigor in the preparation of flowcharts that systematize behavior, or the existence of complex instruments difficult to reproduce. Against this background, we suggest an algorithm that balances content and form, facilitating the practice of professionals who work with scars in general.
REFERENCES
1. Balaraman B, Geddes ER, Friedman PM. Best reconstructive techniques. Dermatol Surg. 2015 Out;41(Supl 10):S265-S75.
2. Yagmur C, Akaishi S, Ogawa R, Guneren E. Mechanical receptor related mechanisms in scar management: a review and hypothesis. Plast Reconstr Surg. 2010 Ago;126(2):426-34.
3. Gold MH, McGuire M, Mustoe TA, Pusic A, Sachdev M, Waibel J, et al. Updated international clinical recommendations on scar management: part 2--algorithms for scar prevention and treatment. Dermatol Surg. 2014 Ago;40(8):825-31.
4. Fearmonti R, Bond J, Erdmann D, Levinson H. A review of scar scales and scar measuring devices. Eplasty. 2010 Jun;10:e43.
5. Ferrari R. Writing narrative style literature reviews. Med Writing. 2015;24(4):230-5.
6. Santos CMC, Pimenta CAM, Nobre MRC. A estratégia PICO para a construção da pergunta de pesquisa e busca de evidências. Rev Latino-Am Enfermagem. 2007 Mai/Jun;15(3):508-11.
7. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016 Dez;5(1):210.
8. Ogawa R. The most current algorithms for the treatment and prevention of hypertrophic scars and keloids. Plast Reconstr Surg. 2010 Fev;125(2):557-68.
9. Kim S, Choi TH, Liu W, Ogawa R, Suh JS, Mustoe TA. Update on scar management: guidelines for treating Asian patients. Plast Reconstr Surg. 2013 Dez;132(6):1580-9.
10. Meaume S, Le Pillouer-Prost A, Richert B, Roseeuw D, Vadoud J. Management of scars: updated practical guidelines and use of silicones. European journal of dermatology: EJD. 2014;24(4):435-43.
11. Mustoe TA, Cooter RD, Gold MH, Hobbs FD, Ramelet AA, Shakespeare PG, et al. International clinical recommendations on scar management. Plast Reconstr Surg. 2002 Ago;110(2):560- 71.
12. Hochmann B, Ramos RR, Isoldi FC, Ferreira LM. Queloide, cicatrizes e úlceras. In: Sato EI, Colombo AL, Borges D, Ramos LR, Ferreira LM, Guinsberg R, et al., eds. Atualização terapêutica de Felício Cintra do Prado, Jairo de Almeida Ramos, José Ribeiro do Valle: diagnóstico e tratamento. 26a ed. São Paulo: Artes Médicas; 2018. p. 739-44.
13. Calderón W, Camacho JP, Obaíd M, Subiabre R, Vinés E. Manejo de queloides mediante combinación de cirugía y radioterapia con haz de electrones. Cir Plást Iberolatinoam. 2020 Mar;46(1):57-64.
14. Carrero KLM, Ma WW, Liu HF, Yin XF, Zhou BR. Botulinum toxin type A for the treatment and prevention of hypertrophic scars and keloids: updated review. J Cosmet Dermatol. 2019 Fev;18(1):10-5.
1. Federal University of São Paulo,
Paulista School of Medicine, Master’s Degree in Science, Technology and
Management Applied to Tissue Regeneration, São Paulo, SP,
Brazil.
2. Federal University of São Paulo,
Paulista School of Medicine, Discipline of Plastic Surgery, São Paulo,
SP, Brazil.
Corresponding author: Francisco Felipe Góis de Oliveira, Rua Barão do Triunfo, nº 79, Rio Vermelho, BA, Brasil, Zip Code 40231-375, E-mail: felipegoismd@gmail.com
Article received: April 21, 2021.
Article accepted: May 18, 2021.
Conflicts of interest: none.
Institution: Universidade Federal de São Paulo, Escola Paulista de Medicina, São Paulo, SP, Brazil.






 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter