

Original Article - Year 2021 - Volume 36 -
Psychological implications for patients with bromhidrosis
Implicações psicológicas nos pacientes com bromidrose
ABSTRACT
Introduction: Bromhidrosis or osmidrosis is a problem that leads many patients to seek specialized medical treatment. This work aims to show that the bromhidrosis disease is also related to the emotional one, which can trigger serious psychological disorders.
Methods: Patients of both genders, predominantly aged between 22 and 42 years, were submitted to consultations and psychological assessments in the preoperative period and psychological follow-up in the postoperative period.
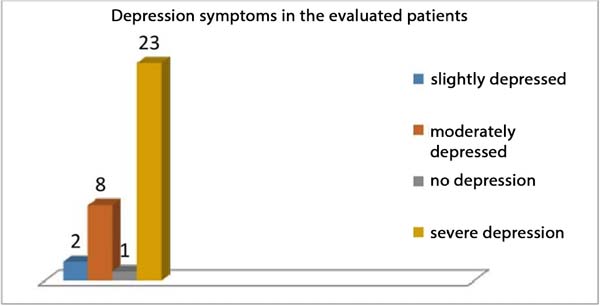
Results: Of the 34 patients evaluated who had a diagnosis of bromhidrosis, 23 had symptoms of severe depression.
Conclusion: Patients diagnosed with bromhidrosis are emotionally vulnerable, depressed and anxious. Without proper treatment, it can lead to serious personality disorders.
Keywords: Depression; Psychological anguish; Sweat gland diseases; Sweat; Reconstructive surgical procedures.
RESUMO
Introdução: A bromidrose ou osmidrose é um problema que leva inúmeros pacientes a procurar tratamento médico especializado. O objetivo deste trabalho é mostrar que a doença bromidrose está também relacionado com o emocional, podendo desencadear transtornos psíquicos graves.
Métodos: Pacientes de ambos os gêneros, com idade predominante entre 22 e 42 anos, foram submetidos a consultas e avaliações psicológica no pré-operatório e o acompanhamento psicológico no pós-operatório.
Resultados: Dos 34 pacientes avaliados que tinham o diagnóstico da bromidrose, 23 apresentaram sintomas de depressão grave.
Conclusão: Os pacientes que apresentam o diagnóstico da bromidrose, são emocionalmente vulneráveis, depressivos e ansiosos. Sem o tratamento adequado pode ocasionar transtornos de personalidades graves.
Palavras-chave: Depressão; Angústia psicológica; Doenças das glândulas sudoríparas; Suor; Procedimentos cirúrgicos reconstrutivos.
INTRODUCTION
Bromhidrosis or osmidrosis is a problem that leads many patients to seek specialized medical treatment. Removing sweat glands from the axillary region through excision and complementary liposuction is a small procedure that is technically simple and with few complications1.
Axillary osmidrosis is caused by excessive apocrine secretion, which causes an arid odor and extreme social embarrassment2.
The disease is also related to the patient’s emotions, leading to psychic changes that interfere in these people’s lives.
Bromhidrosis and its interference with self-esteem
According to Oliveira (2019)3, self-esteem is one of the elements that guide human behavior, enabling healthy and functional intra- and interpersonal relationships.
Individual who suffers from bromhidrosis disease has a great negative impact on their self-esteem. Many out of shame, fear, especially insecurity, move away from family and friends, leave their jobs, and socially isolate themselves.
They end up living only in their world. They become insecure due to people’s opinions, which hurt them many times with words, debauchery and jokes, making their self-esteem more and more destroyed. Low self-esteem can develop several psychological disorders.
Bromhidrosis and its relationship to depression
Depression is classified as a mood disorder; it comes to govern the subjects’ attitudes, modify their perception, and start to see their problems as major catastrophes4.
In the diagnostic and statistical manual of mental disorders (DSM-5), depressive disorders are the presence of sad, empty or irritable mood, accompanied by somatic and cognitive changes that significantly affect the individual’s ability to function. What differs between them are aspects of duration, timing or presumed etiology5.
Lack of self-esteem can lead to depression; bromhidrosis causes great psychological distress in people who have this disease.
They question all the time if they are being punished or if they did something wrong in life to deserve it. They feel anguished, bitter; many want to die to end this suffering, triggering depression for not knowing how to deal with this situation.
OBJECTIVE
The main objective of this work is to evaluate how bromhidrosis emotionally affects patients who have this diagnosis and what are the psychological disorders presented in them.
METHODS
The study consisted of 34 patients diagnosed with bromhidrosis, of which 27 were women (aged 22 to 42 years old), and 7 were men (aged 21 to 32 years old).
All patients received an application/response sheet from the Beck Depression Inventory (BDI-II) by e-mail. After being answered and resent, an analysis of the inventory responses was made. Patients who presented the level of severe symptoms are in psychological follow-up.
The following procedures were used to assess the severity of depression in patients.
The Beck Depression Inventory (BDI-II) is used worldwide to detect depressive symptoms. It is an instrument that aims to measure the intensity of symptoms of depression, has achieved a prominent role in the clinical and research environment for being able to assess subjective feelings and self-perception, important aspects of assisting in the formal diagnosis of depression and which are more difficult to be observed only by clinical evaluation, facilitating the referral of cases of depression for appropriate treatment6.
The Beck-II Depression Inventory (BDI-II) consists of 21 groups of statements about depressive symptoms that could have occurred in the past 15 days. The groups are sadness, pessimism, past failure, loss of pleasure, guilt, feeling of punishment, self-esteem, self-criticism, suicidal thoughts or desires, crying, agitation, loss of interest, indecision, devaluation, lack of energy, changes in sleep pattern, irritability, changes in appetite, difficulty concentrating, tiredness or fatigue and loss of interest in sex.
Each question in the inventory has increasing scores arranged on a Likert-type scale, from 0 to 3, allowing the sum of scores in the range between 0 and 63. In general, the application takes around 10 to 15 minutes and is well accepted by the respondents7.
Special attention should be paid to correctly score sleep pattern changes (item 16) and appetite changes (item 18). Each item contains seven options with values ordered as 0, 1a, 1b, 2a, 2b, 3a and 3b to differentiate the increase and decrease in behavior or motivation. If the respondent selects an alternative with a higher score, both the increase and decrease in any of these symptoms should be considered clinically for diagnostic purposes.
The instruments applied in their order were an informed consent form and the Beck Depression Inventory (BDI-II).
The patients were classified into four groups (mildly depressed, moderately depressed, severely depressed and without depression), following the criteria defined by the diagnostic and statistical manual of mental disorders. In the Beck Depression Inventory (BDI-II), the more intense the symptoms, the more severe or severe the manifestation of depression.
According to the diagnostic and statistical manual of mental disorders8, the level of mild intensity corresponds to the individual with few or no symptoms. They cause suffering but are manageable, and the symptoms result in little impairment of social or professional functioning.
At the moderate level, symptoms are already more present; their intensity or functional impairment are between those specified for “mild” and “severe.”
In severe intensity, the number of symptoms is substantially beyond what is required to diagnose; their intensity causes severe suffering. It is not manageable, and the symptoms strongly interfere with social and professional functioning.
RESULTS
Of the 34 patients evaluated who had a diagnosis of bromhidrosis, 23 were diagnosed with severe depression, eight moderately depressed, two mildly depressed and one without depression (Figure 1).
As shown in Figure 1, of the 34 evaluated patients diagnosed with bromhidrosis, 23 had symptoms of severe depression.
Chart 1 shows the responses of the 34 patients related to the 21 groups of symptoms in Beck’s inventory; the larger the scale that the numbers (2 and 3) are, the greater the symptom of depression.
In the manual from the Beck-II inventory, there is an alert suggesting observing in particular the items that assess pessimism and suicidal ideation that are part of the diagnosis of depression and maybe predictive of a potential for suicide.
In the 21 groups of symptoms presented in the Beck Depression Inventory (BDI-II), the most prevalent statements about depressive symptoms were: Chart 2.
Most of the patients in the pessimism item answered that they have no hope related to the future, with a tendency to worsen. In the item of suicidal thoughts or desires, most have thoughts of killing themselves, but they wouldn’t take it further. Patients are socially isolated due to bromhidrosis; out of fear, they cannot find a solution to the problem, they have tried everything, such as medication, dermo-cosmetics, and others. Due to this pessimism, most begin to have suicidal thoughts to get rid of this anguish.
They feel like failures and punished, losing the pleasure of living. They care about the opinions of people, friends, family and co-workers. They end up criticizing themselves, becoming fragile, anxious, insecure, with their self-esteem destroyed and vulnerable.
The diagnostic hypotheses of patients with bromhidrosis disease, based on the results of the BDI-II depression inventory answered, and the psychological follow-up with them are:
• Major depressive disorder
Diagnostic criteria:
Five(or more) of the following symptoms were present in the same two-week
period and represented a change from previous functioning; at least one
of the symptoms (1) depressed mood or (2) loss of interest or pleasure.
Symptoms of criteria for major depressive disorder must be present
almost every day to be considered current, except for weight change and
suicidal ideation. The depressed mood should be present most of the day,
in addition to being present almost every day [...].
Humor depressed most of the day, most days; A marked decrease in interest or pleasure in all or almost
all activities for most of the day, practically every
day;
Significant weight loss or weight gain without dieting; Insomnia or hypersomnia almost every day; Agitation or psychomotor retardation almost every day; Fatigue or loss of energy almost every day; Feelings of excessive or inappropriate worthlessness or
guilt;
Decreased ability to think or concentrate, or indecision
almost every day;
Recurring thoughts of death.
• Persistent depressive disorder (dysthymia)
The essential feature of persistent depressive disorder (dysthymia) is a depressive mood that occurs most of the day, most days, for at least two years.
“I have difficulty accepting this disease; it messes with my mind a lot.” (MS, 32 years old).
Presence, while depressed, of two (or more) of the following characteristics:
Symptoms cause clinically significant suffering or impairment in social, professional or other important areas of life.
| SYMPTOMS | Affirmations about depressive symptoms |
|---|---|
| 1-Sadness | 0 I don’t feel sad. (3 patients) 1 I feel sad a lot of the time. (27 patients) 2 I am sad all the time. (2 patients) 3 I am so sad or so unhappy that I cannot bear it. (2 patients) |
| 2- Pessimism | 0 I am not discouraged about my future. (10 patients) 1 I feel more discouraged about my future than usual. (8 patients). 2 I don’t expect things to work out for me. (5 patients) 3 I feel there is no hope for my future. I think it will only get worse. (11 patients) |
| 3- Past failure | 0 I don’t feel like a failure. (6 patients) 1 I have failed more than I should. (7 patients) 2 When I think about the past, I see many failures. (15 patients) 3 I feel that as a person, I am a total failure. (6 patients) |
| 4-Loss of Pleasure | 0 I continue to feel the same pleasure I used to get from the things I like. (5 patients) 1 I don’t get as much pleasure from things as I used to. (16 patients) 2 I take very little pleasure in the things I used to enjoy. (10 patients) 3 I no longer enjoy the things I used to like. (3 patients) |
| 5-Feeling of guilt | 0 I don’t feel particularly guilty. (7 patients) 1 I feel guilty about many things I have done and/or should have done. (12 patients) 2 I feel guilty most of the time. (11 patients) 3 I feel guilty all the time. (4 patients) |
| 6-Feeling of punishment | 0 I don’t feel like I’m being punished. (7 patients) 1 I feel I can be punished. (8 patients) 2 I think I will be punished. (4 patients) 3 I feel like I’m being punished. (15 patients) |
| 7-Self-esteem | 0 I feel the way I always felt about myself. (6 patients) 1 I lost confidence in myself. (11 patients) 2 I’m disappointed in myself. (9 patients) 3 I don’t like me. (8 patients) |
| 8-Self-criticism | 0 I don’t criticize or blame myself more than usual. (7 patients) 1 I’m being more critical of myself than I used to be. (5 patients) 2 I criticize myself for all my mistakes. (13 patients) 3 I blame myself for everything bad that happens. (9 patients) |
| 9-Suicidal thoughts or desires | 0 I have no thoughts of killing myself. (14 patients) 1 I have ideas of killing myself, but I wouldn’t go through with it. (17 patients) 2 I would like to kill myself. (1 patient) 3 I would kill myself if given a chance. (5 patients) |
| 10-Cry | 0 I don’t cry any more than I used to cry. (5 patients) 1 I cry more now than I used to. (4 patients) 2 cries for anything. (15 patients) 3 I feel like crying, but I can’t. (10 patients) |
| 11-Agitation | 0 I don’t feel any more restless or agitated than I used to feel. (5 patients) 1 I feel more restless or agitated than I felt before. (10 patients) 2 I feel so restless or agitated that it’s hard to sit still. (11 patients) 3 I’m so restless or agitated that I always have to be moving or doing something. (6 patients) |
| 12-Loss of interest | 0 I haven’t lost interest in other people or my activities. (3 patients) 1 I am less interested in other people or things than I used to be. (7 patients) 2 I have lost almost all interest in other people or things. (18 patients) 3 It’s hard to get interested in anything. (6 patients) |
| 13-Indecision | 0 I make my decisions as well as before. (4 patients) 1 I find it harder to make decisions now than before. (4 patients) 2 I have a lot more difficulty making decisions now than I did before. (3 patients) 3 I have difficulty making any decision. (23 patients) |
| 14- Devaluation | 0 I don’t feel worthless. (7 patients) 1 I don’t consider myself as useful today or value myself as I used to. (4 patients) 2 I feel less valuable when I compare myself to other people. (15 patients) 3 I feel completely worthless. (8 patients) |
| 15-Energy | 0 I have as much energy today as I ever had. (4 patients) 1 I have less energy than I used to have. (10 patients) 2 I don’t have enough energy to do much. (17 patients) 3 I don’t have enough energy for anything. (3 patients) |
| 16-Change in sleep pattern | 0 I didn’t notice any change in my sleep. (5 patients) 1a I sleep a little longer than usual. (9 patients) 1b I sleep a little less than usual. (2 patients) 2a I sleep a lot more than usual. (5 patients) 2b I sleep much less than usual. (9 patients) 3a I sleep most of the day. (3 patients) 3b I wake up 1 or 2 hours early and can’t go back to sleep. (1 patient) |
| 17-Irritability | 0 I’m not angrier than usual. (5 patients) 1 I am angrier than usual. (3 patients) 2 I am much angrier than usual. (14 patients) 3 I get irritated all the time. (12 patients) |
| 18-Appetite changes | 0 I didn’t notice any change in my appetite. (3 patients) 1a My appetite is a little less than usual. (8 patients) 1b My appetite is a little bigger than usual. (5 patients) 2nd My appetite is much smaller than before. (1 patient) 2b My appetite is much bigger than before. (7 patients) 3rd I have no appetite. (9 patients) 3b I want to eat all the time. (1 patient) |
| 19-Difficulty concentrating | 0 I can concentrate as well as before. (4 patients) 1 I can’t concentrate as well as usual. (2 patients) 2 It is very difficult to stay focused on something for a long time. (27 patients) 3 I don’t think I can concentrate on anything. (1 patient) |
| 20- Tiredness or fatigue | 0 I am no more tired or fatigued than usual. (2 patients) 1 I get tired or fatigued more easily than usual. (11 patients) 2 I feel too tired or fatigued to do many of the things I used to do. (7 patients) 3 I feel too tired or fatigued to do most of the things I used to do. (14 patients) |
| 21-Loss of interest in sex | 0 I haven’t noticed any recent changes in my interest in sex. (6 patients) 1 I’m less interested in sex than I used to be. (11 patients) 2 I’m much less interested in sex now. (17 patients) 3 I completely lost interest in sex. |
| BDI-II DEPRESSION INVENTORY | |
|---|---|
| SYMPTOMS | ANSWERS RELATED TO THE SYMPTOMS THAT MOST PREVAILED |
| Sadness | I feel sad a lot of the time. |
| Difficulty in Concentration | It's very difficult to stay focused on something for a long time. |
| Indecision | I have difficulty making any decision. |
| Loss of interest | I almost lost interest in other people or things. |
| Suicidal thoughts or wishes | I have thoughts of killing myself, but I wouldn't go through with it. |
| Lack of energy | I don't have enough energy to do much. |
| Loss of interest in sex | I'm much less interested in sex now. |
| Loss of pleasure | I don't get as much pleasure from things as I used to. |
| Past failure | When I think about the past, I see many failures. |
| Cry | I cry for anything. |
| Devaluation | I feel less valuable when I compare myself to other people. |
| Feelings of punishment | I feel like I'm being punished. |
| Irritability | I'm much angrier than usual. |
| Tiredness or fatigue | I feel too tired or fatigued to do most of the things I used to do. |
| Self-criticism | I criticize myself for all my mistakes. |
| Guilt | I feel guilty about a lot of things I've done and/or should have done. |
| Pessimism | I feel there is no hope for my future. I think it will only get worse. |
| Self-esteem | I lost confidence in myself. |
| agitation | I feel so restless or agitated that it's hard to sit still. |
| Change in sleep pattern | -I sleep a little longer than usual. -I sleep less than usual. |
| Appetite change | I have no appetite. |
BDI-II: Beck Depression Inventory
• Anxiety Disorders
Anxiety disorders include disorders that share characteristics of excessive fear and anxiety and related behavioral disturbances. Fear and emotional response, and real or perceived imminent threat, while anxiety is the anticipation of future threat9.
“I get very anxious because of bromhidrosis, sometimes I have thoughts of cutting my wrist. I want to cry, but I can’t.” (RS, 25 years old).
“Since the first year of college, my classmates made fun of me. The more nervous I was, the greater the smell.” (AG, 22 years old).
“Anxiety is like a portal for bromhidrosis to attack.” (AL, 30 years old).
“When I start studying, I get very nervous, the smell increases, but when I’m taking a walk, or playing video games, the smell disappears.” (FA, 31 years old).
• Generalized Anxiety Disorder
Second Zuardi (2017)10, persistent and excessive worry is the main feature of a generalized anxiety disorder (GAD), but these worries are accompanied by physical symptoms related to autonomic hyperactivity and muscle tension. Among these symptoms, tachycardia, sweating, insomnia, fatigue, difficulty in relaxing and muscle pain are common, which can cause suffering and damage to the individual’s performance.
• Somatic Symptoms Disorder
Arenales et al. (2014)11 cite in the article the illness of suffering from illness, which the DSM-5 manual (diagnostic and statistical manual of mental disorders) uses as its diagnostic core the somatic complaints associated with suffering and disturbance in the patient’s daily life. These complaints can be specific like pain, or not as specific as fatigue. The diagnosis is made when we observe excessive thoughts, feelings or behavior related to somatic symptoms or associated with health concerns.
Diagnostic criteria
A. One or more somatic symptoms that cause distress or result in significant disruption of daily life.
B. Excessive thoughts, feelings or behavior related to somatic symptoms or associated with health concerns expressed by at least one of the following:
“I was sitting talking to my friend, who knows about bromhidrosis, everything was calm.... an acquaintance of hers arrived, I started to feel tense, I felt a heat as if my blood pressure was rising and the odor started to increase too much, it ended up with me.” (AL, 30 years old).
• Social Anxiety Disorder (Social Phobia)
Individuals with social anxiety disorder (SAD) manifest an excessive and persistent fear of one or more social or performance situations. They fear being seen to behave in a humiliating or embarrassing way, and a consequent disapproval or rejection by others. It is observed in these patients a fear of negative evaluation by people, generating feelings of embarrassment, humiliation and shame. They are also characterized by being extremely inhibited and self-critical in social situations that generate anxiety, behaving in a tense and rigid manner, with difficulties in verbally articulating, causing damage to the social performance.12
“I suffered bullying from teachers, they said I was stinking. Laugh at me. I ended up deciding to leave the college.” (AG, 22 years old).
“I was always isolated from my group of friends or distanced myself in conversations for fear of people smelling it.” (RS, 33 years old).
• Obsessive-compulsive disorder
Obsessive-compulsive disorder is characterized by obsessive ideas and/or recurrent compulsive behaviors and has been recognized for its chronic and disabling course. Such ideas and behaviors are very disturbing and consume time in the subject’s life, interfering occupationally and socially13.
“I take a shower several times a day; I even take five showers a day. And I feel the odor doesn’t come out. The more nervous I get, the more the smell increases, I get very distressed, I get out of control.” (GJ, 30 years old).
“I lost count of how many deodorant packages I have at home. I practically work to buy products to get rid of this horrible smell.” (ME, 38 years old).
“Sometimes I think I’m getting paranoid, I start to notice the people around me, and I feel like they’re looking at me, scratching their nose and making a bad face.” (AL, 30 years old).
“In the classroom, I go out almost all the time to go to the bathroom to wash under my arms. It makes me upset people are looking at me all the time.” (GJ, 30 years old).
DISCUSSION
The results show that patients diagnosed with bromhidrosis present psychological distress, which manifests itself through sadness, existential emptiness, causing anxiety, mood swings and social isolation, leading the individual to have depression and other psychological disorders.
Bromhidrosis is a disease that, in addition to treatment, dermatological and surgical, requires specific monitoring of these patients. Psychological support is necessary, considering that people diagnosed with the disease feel psychologically fragile.
This monitoring aims to work on all their emotional and behavioral issues, aiming to minimize the causes that cause the emergence of the odor of bromhidrosis.
CONCLUSION
Through this work, we conclude that patients diagnosed with bromhidrosis are emotionally vulnerable, depressed, impulsive, and have low self-esteem, which causes them to suffer great psychological distress.
Psychological support throughout the surgical process will help the patient with bromhidrosis to feel better, guiding them to seek alternatives to alleviate the feeling of sadness, pessimism and discouragement, and especially, to avoid a future obsession on the part of the patient after the surgery of bromhidrosis.
REFERENCES
1. Kataoka A. Tratamento cirúrgico da bromidrose. Rev Bras Cir Plást. 2017;32(3):377-82.
2. Park YJ, Shin MS. Qual é o melhor método para tratar osmidrose? Ann Plast Surg. 2001 Sep;47(3):303-9. DOI: http://dx.doi.org/10.1097/00000637-200109000-00014
3. Oliveira B. Autoestima, qualidade de vida e saúde. São Paulo: Pimenta Cultura; 2019.
4. Cavalcante EF, Galvan AL. Depressão numa contextualização contemporânea. Aletheia [Internet]. 2006 Dez; [citado 2020 Mai 20]; 1(24):127-35. Disponível em: http://pepsic.bvsalud.org/scielo.php?script=sci_arttext&pid=S1413-03942006000300012&lng=pt
5. American Psychiatry Association. Diagnostic and Statistical Manual of Mental disorders - DSM-5. Porto Alegre:Artmed;2014.p.155.
6. Wendt SMA, Welter G, Lima AII. Inventário de depressão de Beck II: análises pela teoria do traço latente. Aval Psicol [Internet]. 2018 Jul/Set; [citado 2020 Jun 01]; 17(3):339-50. Disponível em: http://dx.doi.org/10.15689/ap.2018.1703.14651.07
7. Beck AT, Steer RA, Brown GK. Manual for the Beck depression inventory BDI-II. San Antonio: Psychological Corporation; 1996.
8. American Psychiatry Association. Diagnostic and Statistical Manual of Mental disorders - DSM-5. Porto Alegre:Artmed;2014.p.188.
9. American Psychiatry Association. Diagnostic and Statistical Manual of Mental disorders - DSM-5. Porto Alegre:Artmed;2014.p.189-190.
10. Zuardi A. Características básicas do transtorno de ansiedade generalizada. Medicina (Ribeirão Preto). 2017 Jan/Fev;50(Supl 1):51-5.
11. Arenales L, Botti N, Machado T. A doença de sofrer de doença. Psychiatry Online. 2014;19(1).
12. Muller JL, Trentini CM, Zaninni AM, Lopes FM. Transtorno de ansiedade social: um estudo de caso. Contexto Clin. 2015;8(1):67-78.
13. Scholl CC, Tabaleão VP, Stigger RS, Trettim JP, Mattos MB, Pires AJ, et al. Qualidade de vida no transtorno obsessivo-compulsivo: um estudo com usuários da atenção básica. Ciênc Saúde Colet. 2017;22(4):1353-60. DOI: https://doi.org/10.1590/1413-81232017224.02062015
1. Hospital Ruben Berta, São Paulo, SP,
Brazil.
AK Analysis and/or data interpretation, Conceptualization, Final manuscript approval, Investigation, Methodology, Supervision, Writing - Original Draft Preparation, Writing - Review & Editing.
CCSM Analysis and/or data interpretation, Conception and design study, Conceptualization, Data Curation, Final manuscript approval, Investigation, Methodology, Validation, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing.
Corresponding author: Alexandre Kataoka, Rua Av. Paulista, nº 2494 cj 14, São Paulo, SP, Brasil, Zip Code 01310-300, E-mail: drkataoka@hotmail.com
Article received: January 28, 2021.
Article accepted: July 14, 2021.
Conflicts of interest: none.
Institution: Hospital Ruben Berta, São Paulo, SP, Brasil.






 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter