

Original Article - Year 2021 - Volume 36 -
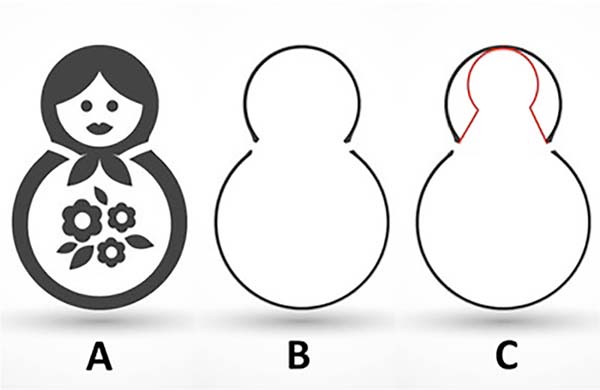
Simplified planning and marking of mastopexy and reduction mammoplasty: the circumvertical "Matryoshka" pattern
Planejamento e marcação simplificados de mastopexia e mamoplastia redutora: o padrão circunvertical "Matryoshka"
ABSTRACT
Introduction: Like most other aesthetic procedures, particularly in paired organs for which symmetry is critical, the successful outcome of mastopexy and reduction mammoplasty is greatly determined by pre-operative planning. By carefully considering the design of the skin resection and choosing and designing an appropriate pedicle, prevention of skin necrosis, unsightly scars, and shape distortion can be minimized.
Methods: We present an original skin marking technique that combines the advantages of using a Wise template as the basis for skin marking with those of the vertical mammoplasty pattern together with a limited circumareolar skin excision to shorten the subareolar vertical scar.
Results: The circumvertical skin marking design we propose mimics a Russian doll silhouette, the “Matryoshka.”
Conclusion: Incorporating a geometrically based and measurable pre-operative marking certainly offers a great degree of control and consistency.
Keywords: Breast; Ambulatory surgical procedures; Mammoplasty; Cosmetic techniques; Elective surgical procedures.
RESUMO
Introdução: Como a maioria dos outros procedimentos estéticos, particularmente em órgãos pareados para os quais a simetria é crítica, o resultado bem-sucedido da mastopexia e mamoplastia redutora é amplamente determinado pelo planejamento pré-operatório. Ao considerar cuidadosamente o desenho da ressecção da pele e escolher e desenhar um pedículo apropriado, a necrose da pele, cicatrizes inestéticas e distorção da forma podem ser minimizadas.
Métodos: Apresentamos uma técnica original de marcação de pele que combina as vantagens do uso de um template Wise como base para marcação de pele com aquelas do padrão de mamoplastia vertical junto com uma excisão periareolar limitada de pele para encurtar a cicatriz vertical subareolar.
Resultados: O design de marcação circunvertical da pele que propomos imita a silhueta de uma boneca russa, a “Matryoshka”.
Conclusão: Incorporar uma marcação pré-operatória mensurável e com base geométrica certamente oferece um grande grau de controle e consistência.
Palavras-chave: Mama; Procedimentos cirúrgicos ambulatoriais; Mamoplastia; Técnicas cosméticas; Procedimentos cirúrgicos eletivos.
INTRODUCTION
Mastopexy and reduction mammoplasty techniques represent both artistic and technical challenges. They aim to reduce the vertical and horizontal planes of the breast, reshape the parenchyma, reposition the nipple-areola complex, and resect redundant skin and breast tissue in excess1. As with any procedure that does not have one ideal method, the literature is replete with different techniques, all of which have certain advantages and definite limitations2.
With the constant reinvention of old ideas and guided by a deeper understanding of the surgical anatomy of the breast, reduction mammoplasty has evolved from primarily reducing breast bulk to reducing with emphasis on functional and aesthetic outcome2. Like most other aesthetic procedures, particularly in-paired organs for which symmetry is critical, a successful outcome is greatly determined by pre-operative planning1. Flaws in design are responsible for a large proportion of unsatisfactory results and shape distortion3.
Skin excision and the pedicle for nipple-areola complex transposition are breast lifting and reduction surgery components. Though related, these two components are independent of each other4. Currently performed techniques result from combining different skin markings for various types of skin excision patterns with a wide variety of pedicles4-9. By carefully considering the design of the skin resection, choosing, and designing an appropriate pedicle, prevention of skin and nipple-areola complex necrosis, unsightly scars, and shape distortion can be minimized3.
Key to the procedure’s success and an aesthetically pleasing outcome is a delicate “shape versus scar” balance. Various short scar periareolar reduction mammoplasty techniques have been proposed to reduce scar burden10,11. The periareolar procedure may be associated with complications, among which are persistent periareolar wrinkles, hypertrophic scarring, areolar spreading, and periareolar scar widening. Despite minimal scar burden, periareolar incision techniques result in poor projection and flattening of the breast contour12. These techniques are advisable only for minimal hypertrophies or breast ptosis13,14. The two most commonly performed skin resection approaches are the Wise keyhole and the vertical scar patterns15; only the vertical scar patterns result in reducing the scar burden at the expense sometimes of long visible vertical scars transgressing the inframammary fold and immediate post-operative unpleasant breast form distortion.
OBJECTIVES
In 2005, the senior author had proposed refinements of the vertical scar mammoplasty with a circumvertical skin excision design16 that has been used exclusively since then on all patients presenting for mastopexy or reduction mammoplasty. This report is not intended to review the outcome of this procedure over the last two decades but rather to describe the simplified skin marking method and the rationale for basing it on the well-established and familiar Wise template. A case series will be illustrated, and a review of available skin marking modalities will also be reviewed.
As such, the purpose of this paper is not to review the outcome that depends on not only the skin excision pattern but for many variables beyond the scope of this report. It is meant to describe a simplified way to perform skin markings of the circumvertical technique, a hybrid technique combining both periareolar and vertical skin excision patterns. No approval from the institutional review board was required, and there is no conflict with the principles of the declaration of Helsinki.
METHODS
Surgical technique
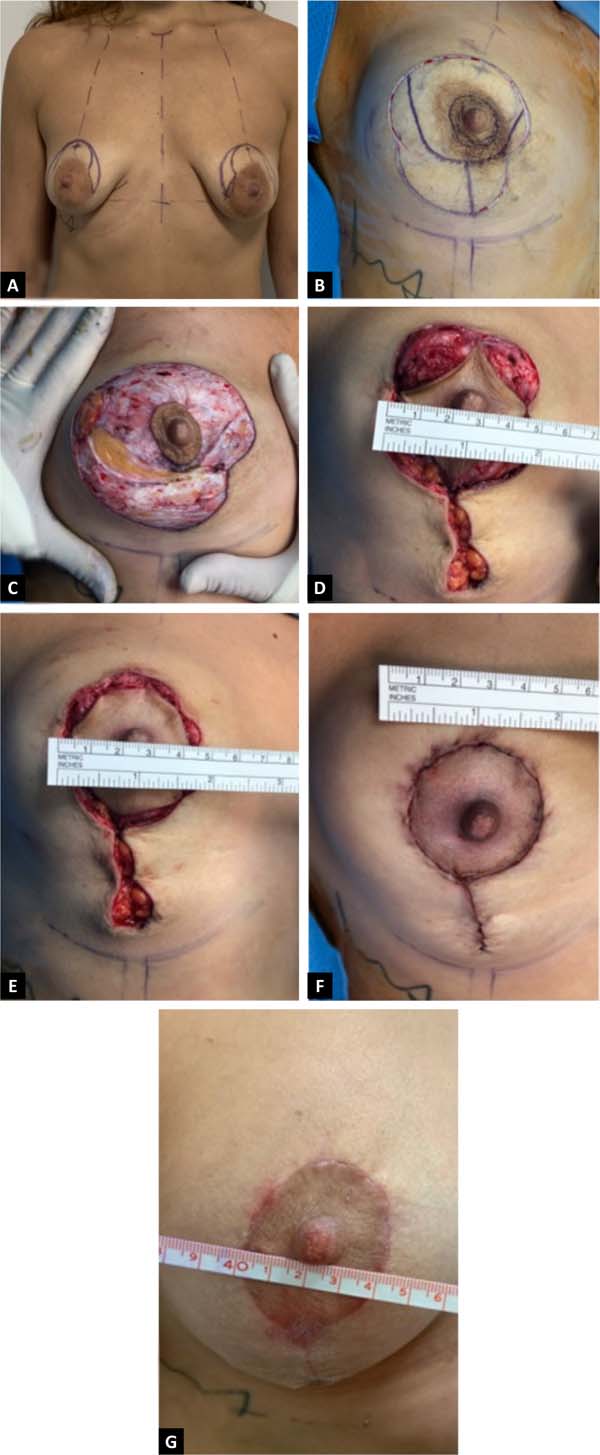
Circumvertical “Matryoshka” Russian doll silhouette skin marking pattern (Figures 1 and 2). A standard Wise keyhole pattern with standard measurements is marked without the elliptical lower component with the patient in the standing position. Initial reference markings are the mid-sternal line, the mid-clavicular point, the existing submammary creases, and the breast axis/meridian. The upper border of the wise template is positioned at the level of the anterior projection of the inframammary line at the intersection with the breast axis. The vertical limbs of the drawing are made to measure 4 cm. Their divergence is adjusted, as usual, depending on the degree of ptosis and the amount of lifting and glandular excision required. For patients with small breasts requiring only mastopexy in whom the subareolar scar length would not be too long, the vertical limbs may be made to measure 2-3 cm. A semicircular new periareolar line is then drawn connecting 3 points: the two lower ends of the vertical limbs and the top of the keyhole pattern. On average, the medial portion of this line is 9 to 11cm from the midline, and the lateral part is approximately 12cm from the anterior axillary line. Though the drawing is freehand, it is greatly facilitated by pre-determination of the three key points.
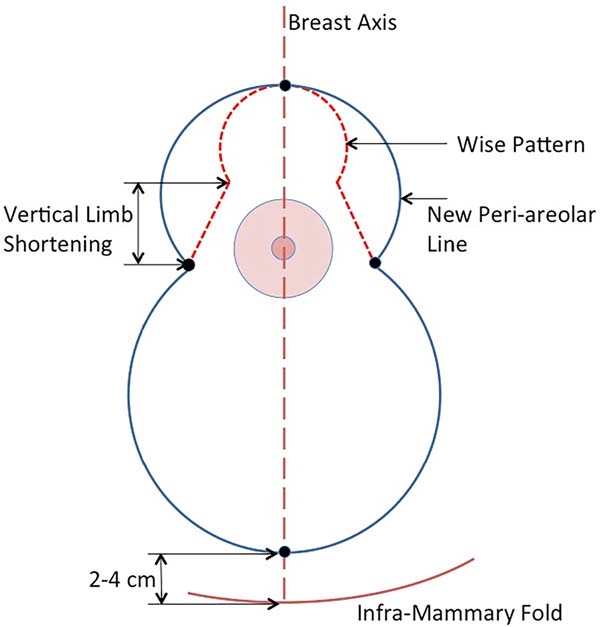
Then with regular Lejour maneuver, medial and vertical lines are dropped from the ends of the new periareolar line. Then, with the patient in the supine position, the vertical lines are connected by a semicircular line, the bottom of which at the breast axis line is two fingers (2-4cm) above the existing inframammary fold (Figure 3). The marking is finally completed at the operating table by delineating an areola 4 to 5cm in diameter as indicated.
In patients with severe gigantomastia or poor skin tone in which the vertical lines are judged to be still too long, resulting in prolonged or permanent skin pleating, vertical subareolar limbs measuring 7-8 cm are considered shortening the glandular vertical pillars. A horizontal skin excision may also be added to the marking at this level, maintaining the lower horizontal incision line 2 fingers (2-4cm) above the existing inframammary crease, thus converting the drawing to an inverted “T” design with the vertical subareolar limbs measuring 7-8cm. Alternatively, the decision to convert the design to an “L” or short inverted “T” may be made intraoperatively as required. In the eventuality of an inverted “T” design, preservation of de-epithelialized dermal flaps at the lower border of the medial and lateral pillars allows secure closure with no tension at the “T”-junction, greatly reducing the risk of wound dehiscence (Figure 4).
Post-operative care
No drains were placed during surgery. Patients were either discharged the same day or stayed one night, depending on patient preference. Post-operatively, patients were prescribed painkillers and antibiotics for one week. On follow-up appointments at one week, two weeks and every month after that, patients’ wounds were evaluated. Most patients were followed up for at least two years and were satisfied with the aesthetic result and scars. Over the study period, none of the patients required scar revision. Only one patient presenting with gigantomastia, early on when we started applying this pattern, required revision for pseudoptosis secondary to insufficient glandular tissue excision with very long vertical pillars.
RESULTS
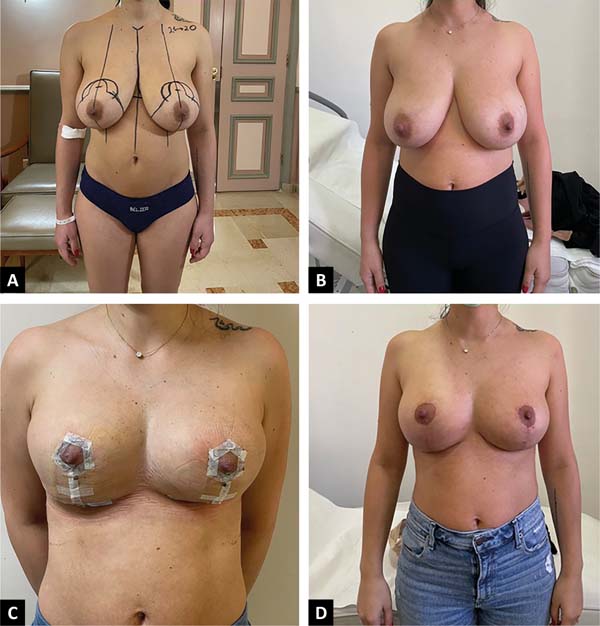
Case Report #1:
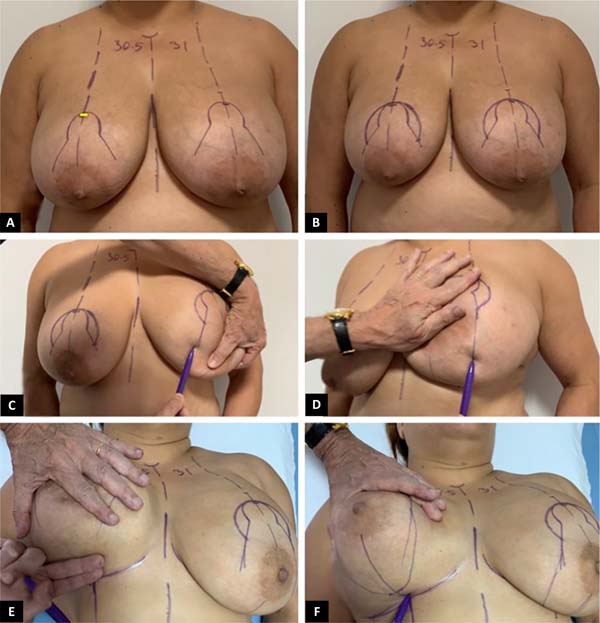
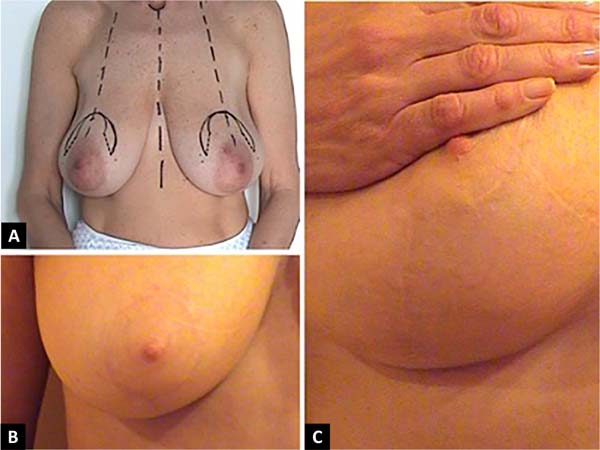
A 30-year-old healthy non-smoker patient presented 1-year post-partum complaining of large breasts and sought breast reduction (Figure 5).
A circumvertical “Matryoshka” design was planned; 160g was resected from the lower pole of each breast. The patient’s pre-operative markings are shown along with photos preoperatively and upon immediate follow-up and at six months to show the stability of the result. The patient is reportedly satisfied and pleased with the shape.
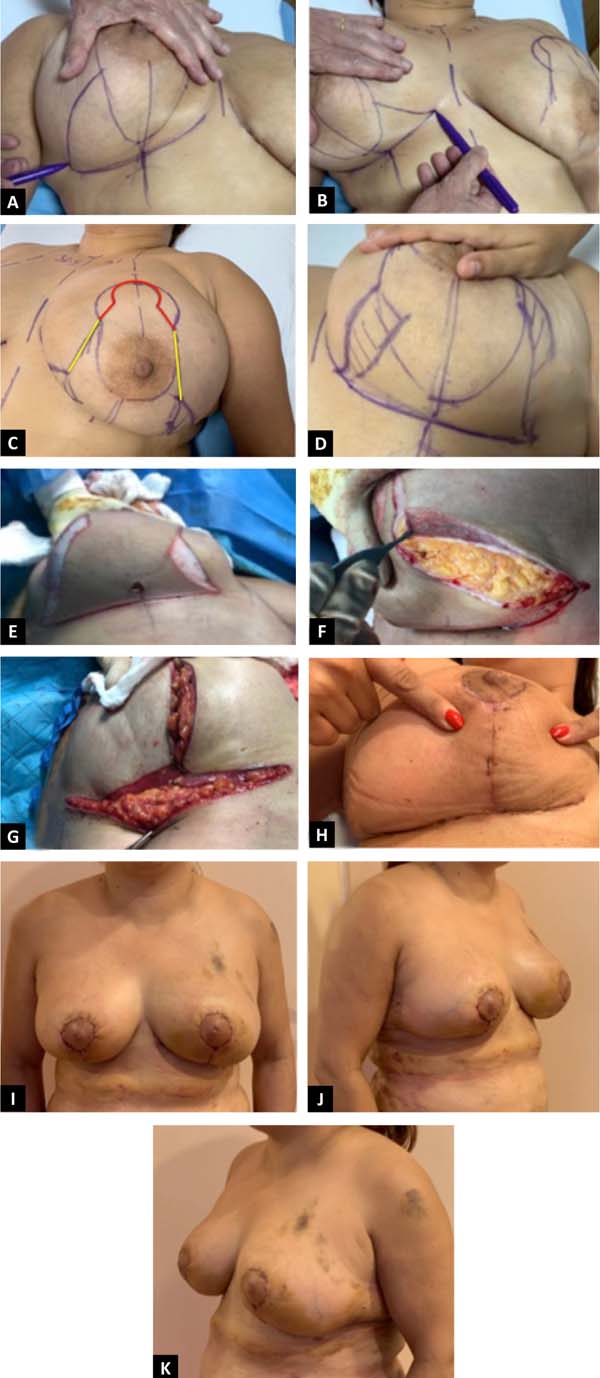
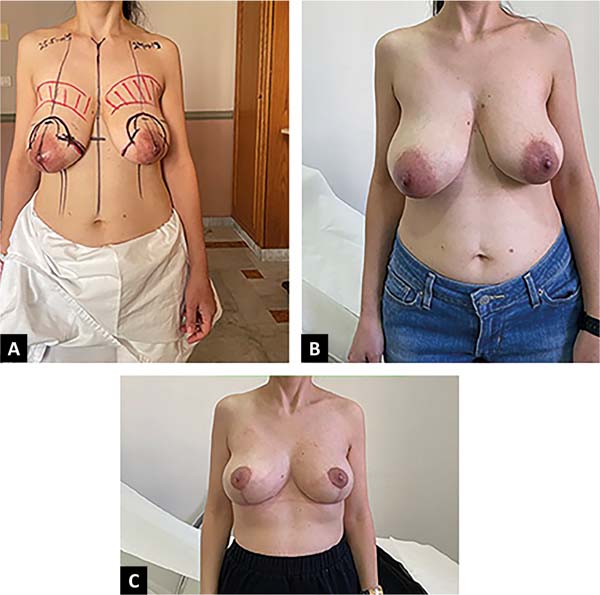
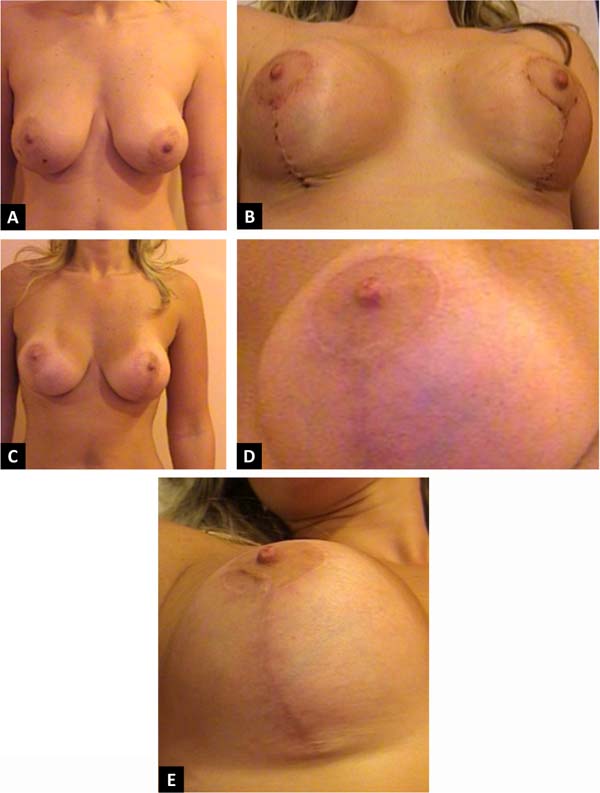
Case Report #2:
A 44-year-old healthy non-smoker multi-gravid patient presented with the complaint of breast asymmetry, as well as sagging of her breasts. She had initially specifically requested a Benelli mastopexy, as she feared the scars. Upon extensive counseling, she agreed to undergo a circumvertical “Matryoshka” mastopexy (Figure 6).
The patient’s pre-operative markings are shown along with photos preoperatively and followed up at five months. The patient is reportedly very satisfied and pleased with the scars and the shape of her breasts.
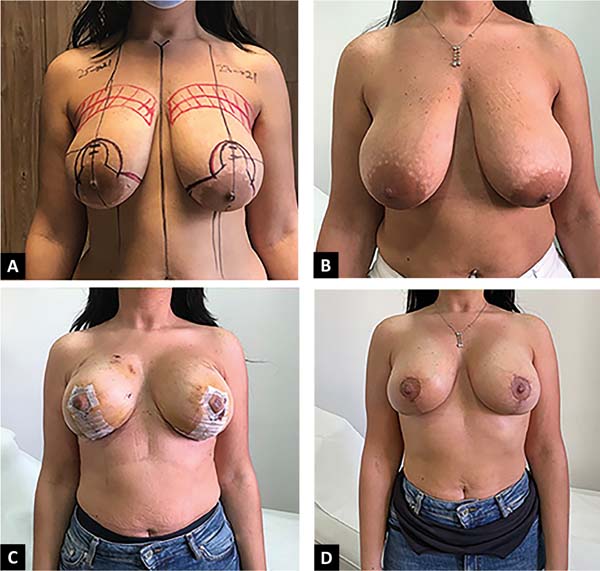
Case Report #3:
A 34-year-old healthy but heavy smoker patient presented complaining of sagging breasts and not desiring any reduction in breast shape. She was counseled about the need for smoking cessation and was offered a circumvertical “Matryoshka” mastopexy in combination with Hamdi’s volume distribution mastopexy48 (Figure 7).
The patient’s pre-operative markings are shown along with photos preoperatively, as well as upon immediate follow up and at 2 months. The patient is reportedly very satisfied and pleased with the scars as well as the shape of her breasts.
DISCUSSION
Several years ago, Penn (1955)17 and Wise (1956)18 described surgical landmarks that ensured reproducible mammoplasty aesthetic outcomes. These landmarks as well as metrics of the ideal aesthetic breast shape have been recently reviewed19. Moreover, major progress was made when, in 1956, Wise18 designed a skin resection template based on brassiere “Cordelia of Hollywood” bra cups20, which became known as the keyhole inverted “T” pattern, and when principles of breast remodeling while preserving nipple areolar complex vascularity were elaborated by numerous surgeons, each in his own way, including Skoog (ANO)5, Arie (ANO)5, Strombeck (1960)21, Pitanguy (1967)22, McKissock (1972)23, Robbins (1977)24, and Courtiss and Goldwyn (1977)25.
Not satisfied with procedures relying on skin brassiere for breast shaping and support that generally tend to deteriorate with time12, Lassus (1996)26 in the 1970s perfected and published the vertical mammoplasty that was later popularized by Lejour (1994)27,28 and modified by Hall-Findlay (2004)9. Key features of the vertical scar technique are skin excision in only one direction, which reduces scar burden16,28-31. Though fixed landmarks are taken into consideration, vertical mammoplasties have been criticized for being intuitive and difficult to learn; the most difficult aspect of the technique is lack of a simple standardized pattern to follow. In fact, free hand drawing has been a major hurdle that has prevented this modality from gaining wide acceptance32,33 in addition to long subareolar vertical scars and skin redundancy at the level of the inframammary crease constituting major drawbacks9,12,31.
Despite the generalized acceptance that short scar techniques are good options for many patients and despite the universal desire to minimize scarring, the classic inverted “T” Wise pattern skin marking remains the most commonly used technique3,7. It is the standard to which more recent limited scar techniques are judged34,35, most likely because of the comfort level that surgeons have in applying the template to all varieties and sizes of breast reductions and mastopexies3. Although this technique has endured, it has certainly evolved since was first conceived3.
Current wise pattern breast reductions are very different from the original description with widely variable design depending on the length and angle of divergence of the vertical limbs, degree of undermining, and the length of the IMF incision3. The McKissock (1972)23 keyhole marker has been proposed as a practical interpretation of the original wise template3. A template-goniometer has also been described35.
Hybrid procedures combining advantages while minimizing disadvantages of previously described techniques are common in the plastic surgery literature. Breast reduction and mastopexy are no exception. Based on the wise pattern, the superior pedicle, short horizontal scar breast reduction has been described as a hybrid procedure to redistribute excess in horizontal elliptical resection to wider vertical and periareolar resections36. However, periareolar skin excision of this technique is very limited. Ramirez (2002)37 described the “owl” reduction mammoplasty combining features of large periareolar and vertical reduction techniques. However, marking of this technique is made free hand and is somewhat complicated to execute. The circumvertical technique can be an alternative method to both the periareolar and the vertical techniques. It combines vertical mammoplasty with a wider periareolar skin excision and practically effects skin excision both vertically and horizontally38-40. Excision of wider periareolar skin diminishes the length of the vertical scar; conversely, inclusion of a vertical component to the periareolar technique reduces periareolar pleating37. Described skin marking of this technique remains however intuitive and free hand.
Though many have challenged that rigid and standard patterns may not take into account individual variations in glandular density and positioning within the skin envelope advocating more liberal and free hand drawings6, use of design templates for pre-operative skin marking is highly practical and desirable35. It can thoroughly help to simplify surgery and achieve reproducible and satisfactory results, especially for trainees or surgeons at the early days of their practice7. Basing the drawings on the well-established and familiar Wise template as we are suggesting makes the circumvertical “Matryoshka” design very attractive; it can be demonstrated and taught to trainees easily. Gumus et al. (2006)33 reported 1 year later a somewhat comparable marking pattern; however, they used the keyhole pattern as a guide to provide a consistent estimation for the amount of dermoglandular tissue to be removed from the inferior breast pole and not to determine extent of periareolar skin excision as we are proposing.
Traditionally, the circumference of the areolar skin opening is made to match the circumference of the ideal areola2. In both the wise and vertical patterns, the circumareolar incision is made 14-16cm in length matching the circumference of a circle 4.5-5cm in diameter presumably to minimize periareolar tension, avoid areola and periareolar scar stretching, areola flattening and the dreaded “starburst” appearance and “tomato breast” deformity41. Lejour (1994)28 has stressed that the periareolar incision should not exceed 16cm in length. Hall-Findlay (2004)9 suggested that it is possible to make it a bit larger, but not exceeding 20cm31. Spear et al. (1992)42 on the other hand, demonstrated that a much longer periareolar incision up to 25-28cm matching the circumference of a circle 8-9cm in diameter double that of a regular areola may be made without risking the complications Lejour (1994)28 and Hall-Findlay (2004)9 have warned against. The outer circle diameter however must not be drawn to exceed twice the size of the areola constituting the inner circle43. The method proposed for the circumvertical “Matryoshka” drawing has been effective in guiding wide periareolar excision while avoiding excessive excision as recommended by Spear et al. (1992)42. It must be noted that a wide periareolar excision adds an element of horizontal skin excision and results in an upward lift of the subareolar skin resulting in shorter vertical suture line (Figures 8, 9, and 10). The possibility to develop a wide base to the superior dermoglandular pattern that would improve NAC vascular perfusion37 would be another advantage.
To avoid a teardrop-shaped areola, Hammond and Kim (2016)10 recommended approximation of the periareolar incision with an accurately placed key-anchoring suture. Exact placement of this suture in the planning we are proposing is not intuitive. It is predetermined by pre-operative marking and corresponds to the medial and lateral ends of the periareolar incision16. Blocking triangles as described by Lista and Ahmad et al. (2006)30 are not necessary. Placement of a Benelli round-block suture claimed to be key in preventing areolar widening and scar hypertrophy and spread43 is not necessary or effective as well41 provided extent of periareolar skin excision be kept within the limits defined by the circumvertical “Matryoshka” pattern. In fact, a well-defined circular area corresponding approximately to an areola of 4-5cm in diameter becomes readily defined following placement of this key suture provided glandular mound has been properly formed.
Unlike other vertical scar techniques that take several months to achieve final breast shape, we have invariably achieved a pleasing breast shape very early with the circumvertical “Matryoshka” pattern in a wide range of breast mastopexies and reductions much like what Lista and Ahmad et al. (2006)30 have reported. This proves that the characteristically unusual appearance at the end of the procedure and the frequently described immediate exaggerated upper pole fullness and inferior pole flatness are not an inherent and unavoidable characteristic of the vertical mammoplasty technique. Balanced and well-controlled skin excision pattern when combined with well thought breast parenchyma resection and NAC pedicle transposition can achieve early and long-term pleasing aesthetic outcome.
Furthermore, in case of conversion to an inverted “T” design, several techniques have been described to minimize tension, ischemia, and wound-healing problems at the “T”-junction44-47. Unlike the narrow based triangular lipodermal flaps hinged to the musculo-aponeurotic connective tissue of the inframammary fold with 1 apical stay suture at the breast meridian44, or the three triangular dermal flaps modification in which the inferior flap width allows fixing the upper flaps with two sutures laterally to limit central tension46, or the crossed dermal flaps that lead to bulkiness and unevenness both at the “T”-junction and along the transverse suture line45, preservation of de-epithelialized dermal flaps as we are describing at the entire lower border of the medial and lateral pillars, allows secure skin closure without tension at the “T”-junction and the horizontal suture line by shifting the tension deep with even distribution using several anchoring sutures to the chest wall.
CONCLUSION
The key to a good mastopexy or breast reduction design is understanding what the chosen method can offer. Ultimately, it is based on the patient’s morphology and the surgeon’s artistry and experience. However, incorporating a geometrically based and measurable pre-operative marking certainly offers a great degree of control and consistency. Though this report is not a structured retrospective study, we can confirm with confidence that circumvertical “Matryoshka” surgical planning guided by the user-friendly Wise template is straightforward and easy to learn; it has proven to be very versatile, applicable to mastopexy, reduction mammoplasty, and augmentation mastopexy as well as to oncoplastic surgery. Though we prefer a superior dermoglandular pedicle, it can be applied as well with any type of NAC pedicle whenever deemed necessary.
ACKNOWLEDGEMENT
The authors declare that they have no conflict of interest.
EBM level IV: Evidence obtained from multiple time series with or without the intervention, such as case studies. Dramatic results in uncontrolled trials might also be regarded as this type of evidence.
REFERENCES
1. Fahmy FS, Hemington-Gorse SJ. The sitting, oblique, and supine marking technique for reduction mammaplasty and mastopexy. Plast Reconstr Surg. 2006 Jun;117(7):2145-51.
2. Hall-Findlay EJ, Shestak KC. Breast reduction. Plast Reconstr Surg. 2015 Oct;136(4):531e-44e.
3. Hansen JE. Avoiding the unfavorable outcome with wise pattern breast reduction. Clin Plast Surg. 2016 Apr;43(2):349-58.
4. Davison SP, Mesbahi AN, Ducic I, Sarcia M, Dayan J, Spear SL. The versatility of the superomedial pedicle with various skin reduction patterns. Plast Reconstr Surg. 2007 Nov;120(6):1466-76.
5. Wamalwa AO, Stasch T, Nangole FW, Khainga SO. Surgical anatomy of reduction mammaplasty: a historical perspective and current concepts. S Afr J Surg. 2017 Mar;55(1):22-8.
6. Castro CC, Coelho RFS, Cintra HP. The value of non-prefixed marking in reduction mammoplasty. Aesthetic Plast Surg. 1984;8(4):237-24.
7. Guridi R, Rodriguez JR. A step-by-step approach to a successful cosmetic breast reduction. Plast Reconstr Surg Glob Open. 2019 Apr;7(4):e2117.
8. Rohrich RJ, Thornton JF, Jakubietz RG, Jakubietz MG, Grünert JG. The limited scar mastopexy: current concepts and approaches to correct breast ptosis. Plast Reconstr Surg. 2004 Nov;114(6):1622-30.
9. Hall-Findlay EJ. Vertical breast reduction. Semin Plast Surg. 2004 Aug;18(3):211-24.
10. Hammond DC, Kim K. The short scar periareolar inferior pedicle reduction mammaplasty: management of complications. Clin Plast Surg. 2016 Apr;43(2):365-72.
11. Benelli L. A new periareolar mammaplasty: the “round block” technique. Aesthetic Plast Surg. 1990 Spring;14(2):93-100.
12. Zavrides H. The classic Pitanguy technique and its modifications in mammaplasty: ten years of experiences. Ann Plast Surg. 2017 Nov;79(5):433-7. DOI: https://doi.org/10.1097/SAP.0000000000001145
13. Baran CN, Peker F, Ortak T, Sensöz O, Baran NK. Unsatisfactory results of periareolar mastopexy with or without augmentation and reduction mammoplasty: enlarged areola with flattened nipple. Aesthetic Plast Surg. 2001 Jul/Aug;25(4):286-9.
14. Cho BC, Yang JD, Baik BS. Periareolar reduction mammoplasty using an inferior dermal pedicle or a central pedicle. J Plast Reconstr Aesthet Surg. 2008;61(3):275-81.
15. Becker DB. The Paisley pattern breast reduction. Plast Surg (Oakv). 2019 May;27(2):189-94.
16. Atiyeh BS, Rubeiz MT, Hayek SN. Refinements of vertical scar mammaplasty: circumvertical skin excision design with limited inferior pole subdermal undermining and liposculpture of the inframammary crease. Aesthetic Plast Surg. 2005 Nov/Dec;29(6):519-31.
17. Penn J. Breast reduction. Br J Plast Surg. 1955 Jan;7(4):357e-71e.
18. Wise RJ. A preliminary report of a method of planning the mammaplasty. Plast Reconstr Surg. 1956 May;17(5):367-75.
19. Atiyeh B, Chahine F. Metrics of the ideal breast. Aesthetic Plast Surg. 2018 Dec;42(5):1187-94.
20. Lazarus D. A new template-goniometer for marking the wise keyhole pattern of reduction mammaplasty. Plast Reconstr Surg. 1998 Jan;101(1):171-3.
21. Strombeck JO. Report of a new technique based on the two-pedicle procedure. Br J Plast Surg. 1960 Apr;13:79-90.
22. Pitanguy I. Surgical treatment of breast hypertrophy. Br J Plast Surg. 1967 Jan;20(1):78-85.
23. McKissock PK. Reduction mammaplasty with a vertical dermal flap. Plast Reconstr Surg. 1972 Mar;49(3):245-52.
24. Robbins TH. A reduction mammoplasty with the areola-nipple based on an inferior dermal pedicle. Plast Reconstr Surg. 1977;59(1):64-7.
25. Courtiss EH, Goldwyn RM. Reduction mammaplasty by the inferior pedicle technique. Plast Reconstr Surg. 1977 Apr;59(4):500-7.
26. Lassus C. A 30-year experience with vertical mammaplasty. Plast Reconstr Surg. 1996;97(2):373-80.
27. Foustanos A, Panagiotopoulos K, Skouras G. Intraoperative modification of Pitanguy technique of reduction mammaplasty for elevation of the nipple-areola complex in case of severe breast ptosis. Aesthetic Plast Surg. 2011 Feb;35(1):55-60.
28. Lejour M. Vertical mammaplasty and liposuction of the breast. Plast Reconstr Surg. 1994 Jul;94(1):100-14.
29. Van Thienen CE. Areolar vertical approach (AVA)mammaplasty: Lejour’s technique evolution. Clin Plast Surg. 2002 Jul;29(3):365-77.
30. Lista F, Ahmad J. Vertical scar reduction mammaplasty: a 15-year experience including a review of 250 consecutive cases. Plast Reconstr Surg. 2006 Jun;117(7):2152-65;discussion:2166-9.
31. Ahmad J, Lista F. Vertical scar reduction mammaplasty: the fate of nipple-areola complex position and inferior pole length. Plast Reconstr Surg. 2008 Apr;121(4):1084-91.
32. Poëll JG. Vertical reduction mammaplasty. Aesthetic Plast Surg. 2004 Mar/Apr;28(2):59-69.
33. Gumus N, Coban YK, Demyrkiran MS. Vertical mammaplasty marking using the key hole pattern. Aesthetic Plast Surg. 2006 Mar/Apr;30(2):239-46;discussion:247-8.
34. Hidalgo DA. Improving safety and aesthetic results in inverted T scar breast reduction. Plast Reconstr Surg. 1999 Mar;103(3):874-86;discussion:887-9.
35. Lazarus D. A new template-goniometer for marking the wise keyhole pattern of reduction mammaplasty. Plast Reconstr Surg. 1998 Jan;101(1):171-3.
36. Bitik O, Hakan U. Analysis of lower breast pole length and nipple-areola complex position following superior pedicle, short horizontal scar breast reduction Aesthetic Plast Surg. 2016;40(5):690-8.
37. Ramirez OM. Reduction mammoplasty with the “owl” incision and no undermining. Plast Reconstr Surg. 2002 Feb;109(2):512-22;discussion:523-4.
38. Gulyás G. Combination of the vertical and periareolar mammaplasty. Aesthetic Plast Surg. 1996 Sep/Oct;20(5):369-75.
39. Mottura AA. Circumvertical reduction mammaplasty. Clin Plast Surg. 2002 Jul;29(3):393-9.
40. Mottura AA. Circumvertical reduction mastoplasty: new considerations. Aesthetic Plast Surg. 2003 Mar/Apr;27(2):85-93.
41. Swanson E. Periareolar augmentation/mastopexy: how does it measure up?. Aesthetic Surg J. 2019 Oct;39(11):NP452-NP4.
42. Spear SL, Kassan M, Little JW. Guidelines in concentric mastopexy. Plast Reconstr Surg. 1990 Jun;85(6):961-6.
43. Davison SP, Spear SL. Simultaneous breast augmentation with periareolar mastopexy. Semin Plast Surg. 2004 Aug;18(3):189-201.
44. Khalil HH, Malahias M, Shetty G. Triangular lipodermal flaps in Wise pattern reduction mammoplasty (superomedial pedicle): a novel technique to reduce T-junction necrosis. Plast Surg (Oakv). 2016;24(3):191-4.
45. De la Plaza R, De la Cruz L, Moreno C, Soto L. The crossed dermal flaps technique for breast reduction. Aesthetic Plast Surg. 2004 Nov/Dec;28(6):383-92.
46. Domergue S, Ziade M, Lefevre M, Prud’homme A, Yachouh J. Dermal flaps in breast reduction: prospective study in 100 breasts. J Plast Reconstr Aesthet Surg. 2014 Jun;67(6):e147-50.
47. Akhtar S, Whittaker I, Fourie LA. A novel tension-reducing suture to protect the T-junction after reduction mammaplasty. Plast Reconstr Surg. 2007 Apr;119(4):1386-7.
48. Hamdi M, Chahine F, Alharami S, Baerdemaeker R, Hendrickx B, Zeltzer A. The 10-year experience with volume distribution mastopexy: a novel, safe, and efficient method for breast rejuvenation. Plast Reconstr Surg. 2021 May;148(1):55-64.
1. American University of Beirut Medical Center,
Beirut, Beirut, Lebanon.
2. Institute Sirio Libanês Hospital, Sao
Paulo, SP, Brazil.
3. Trad Hospital and Medical Center, Beirut,
Beirut, Lebanon.
BA Analysis and/or data interpretation, Conceptualization, Final manuscript approval, Supervision, Writing - Original Draft Preparation, Writing - Review & Editing.
RF Final manuscript approval, Supervision, Writing - Original Draft Preparation, Writing - Review & Editing.
NH Analysis and/or data interpretation, Data Curation, Final manuscript approval, Methodology, Writing - Original Draft Preparation, Writing - Review & Editing.
FC Analysis and/or data interpretation, Conception and design study, Final manuscript approval, Writing - Original Draft Preparation, Writing - Review & Editing.
Corresponding author: Fadl Chahine, Trad Hospital and Medical Center, Beirut - Lebanon, E-mail: Fadel@Chahine.md
Article received: May 17, 2020.
Article accepted: July 14, 2021.
Conflicts of interest: none.
Institution: American University of Beirut Medical Center, Beirut, Lebanon.













 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter