

Articles - Year 1997 - Volume 12 -
Critical Analysis of the Rotation Arc and Aesthetical Positioning of the Tram-flap in Breast Reconstructions
Análise Crítica do Arco de Rotação e Posicionamento Estético Funcional do Tram-Flap nas Reconstruções Mamárias
ABSTRACT
This study aims at facilitating the understanding of the torsion process applied to the whole vascular pedicle which nourishes the island of abdominal dermal-adipose tissue at the moment in which it is shaped in the thoracic compartment of the previous mastectomy to create a new breast. Since the original works published about the utilization of myocutaneous flaps in breast reconstructions, we have not observed any references to the care which must be taken to apply the least aggressive possible approach to the unipedicle or bipedicles which warrant the arterial and venous circulation of this flap. By means of foam models, we have displayed exactly what happens in vivo, and their visual correlation with the corresponding surgical times. The bilateral flap presents a tridimensional behaviour quite different from the unilateral one, with more limited possibilities for a good shaping. All positions were easily identified, permitting a better understanding of those which present greater or smaller circulatory risk for the flap. We have finally understood the reason for some superficial losses in flaps which seemed so well nourished, frequently of a venous nature. This study purpose was sedimentating the tram-flap safest positions in breast reconstructions, by means of agreater understanding of the muscular pedicle rotation are and torsions.
Keywords: Abdominal Flap, Breast Reconstruction, Rectoabdominal
RESUMO
A apresentação deste estudo visa tornar mais claro o entendimento do processo de torção a que é submetido todo o pedículo vascular que nutre a ilha de tecido dermo-adiposo abdominal no momento em que esta é modelada no compartimento torácico da antiga mastectomia, com a finalidade de criarmos uma neo-mama. Desde os trabalhos originais do uso de retalhos miocutâneos nas reconstruções mamárias que não observamos qualquer referência aos cuidados que devemos tomar para agredir o menos possível o pedículo (uni) ou os pedículos (bi) que garantem a circulação arterial e venosa desse retalho. Conseguimos demonstrar através de modelos em espuma exatamente o que se passa in vivo, e a sua correlação visual com os tempos cirúrgicos correspondentes. O retalho Bilateral tem um comportamento tridimensional bastante diferente do unilateral com possibilidades mais limitadas para uma boa modelagem. Todas as posições foram facilmente identificadas e daí o melhor entendimento daquelas consideradas de maior ou menor circulatório para o retalho. Passamos a compreender o porquê de certas perdas superficiais em retalhos que pareciam tão bem nutridos e com frequência de natureza venosa. A finalidade deste estudo foi sedimentar as posições de maior segurança com o tram-flap nas reconstruções mamárias, através da maior compreensão tridimensional do arco de rotação e das torções do pedículo muscular.
Palavras-chave: Retalho abdominal; Reconstruções mamárias; Reto abdominal
Since the original works first published by authors like HOLMSTRÖM, HARTRAMPF, DREAVER, VIEIRA, CHVEID and KOGUT (1, 2, 3, 4), we have not found any references in the literature about circulatory problems caused by possible torsions of the rectoabdominal vascular pedicle at the moment of the shaping to which this whole assemblage is submitted so that we can obtain a new breast. Complications are always associated to vascular problems possibly caused by excessive devascularization of the muscle, inadequate sectioning of the upper epigastric artery, hematomas and infections, or even to unexpected anatomical variations. These causes can reallylead to some form of unsuccessful outcome, but quite frequently we can observe some immediate degree of cyanosis on the flap, which alerts us about some abnormality at the vascular territory, especially the venous one, without any specific cause. Putting the flap back to its original position on the abdomen, we verify that the microcirculation stabilizes and the flap is preserved. Observing such a phenomenon, we started to believe that the complete turn of 1800 plus two torsions of the muscular vascular pedicle at the level of the perforating vessels could contribute in some way to this structural blood flow interruption. This fact could depend on some factors related to the muscular anatomy itself, like its width and length, as well as on some patients' own characteristics as brevitypes or longitypes or a receptor area more or less damaged by the previous mastectomy.
MATERIAL AND METHODS
We have prepared three basic foam molds. The first represents the whole abdominal island with the two muscles; the second represents the hemiabdomen with its corresponding muscle for contralateral transposition and the third the hemiabdomen with its muscle for homolateral transposition. Based on widely discussed criteria about vascular territories and their dominances, we have numbered the abdominal island cutaneous areas as follows:
- Area 1 - the one which corresponds to the periumbilical perforating vessels;
- Area 2 - the one which corresponds to the homolateral neighbouring area;
- Area 3 - the one which corresponds to the contralateral neighbouring area;
- Area 4 - the one which corresponds to the contralateral extremity.
Such a numerical sectorization corresponds to the vascular importance in the cutaneous island relative to the perforating vessels of the unilateral rectoabdominal. When we use the bilateral flap, this sectorization will present only areas 1 and 2 for each muscle.
Bilateral Mold
We have submitted this assemblage to an upward motion at 180º exactly as it happens during the surgical procedure, verifying the first torsion. Next, we positioned the foam island (abdomen) outward with the navel transversally upward (position 2112), detecting the second torsion. We started to submit the whole island to a clockwise rotation motion, bringing it to an oblique and vertical position and identifying the effect on the pedicle. From this moment on, we proceeded the motion bringing the island back to an horizontal position, but with the navel downward and the contralateral muscle passing in front of the homolateral one, which means these muscles were not parallel anymore and positioned themselves in a third torsion. This third torsion, however, may also be obtained by a motion in the opposite direction and, in this circumstance, the contralateral muscle will pass under the homolateral one. This whole process was performed for a right side mastectomy. For a left side mastectomy, the whole described process will be reversed, which means that it is with the anticlockwise rotation that the contralateral muscle passes in front of the homolateral one.
Contralateral Unilateral Mold
The first torsion is detected also at the 180º motion. The second torsion occurs when we position the island flap outward, stablishing the position 312 in which the navel turns downward. This position can be obtained with a rotation both in one direction and in the opposite one. However, if we position the navel upward, the transversal position 213 is obtained. We may obtain several intermediary positions moving obliquely the island clockwise (right side mastectomy) or anticlockwise (left side mastectomy).

Fig. 1. Foam model for contralateral rotation.
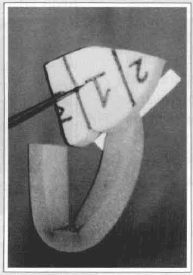
Fig. 2. Upward rotation for position 312. Internai rotation.
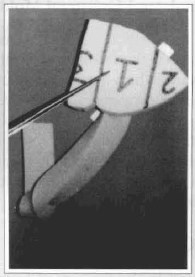
Fig. 3. Upward rotation for position 312. Externai rotation.
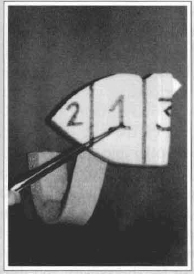
Fig. 4. Upward rotation for position 213. Transverse. Dangerous.
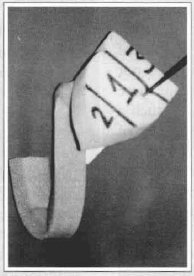
Fig. 5. Upward rotation for position 213. Oblique. It undoes the torsion behind the flap.
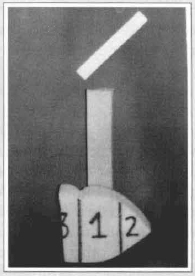
Fig. 6. Foam model for homolateral rotation. It starts on position 312.
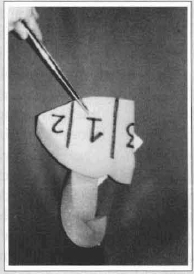
Fig. 7. Upward rotation for position 213. External or internal rotation.

Fig. 8. Visual correspondence in vivo.
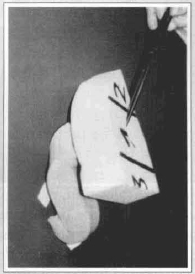
Fig. 9. Upward rotation for position 312 without torsion behind the flap.
Homolateral Unilateral Mold
The first torsion is also verifyed at the 180º motion. With the second torsion the island flap turns outward, which happens both in one direction and in the opposite one, and the navel turns downward. This is the transverse position 213. If the navel is positioned upward, the transverse position 312 is obtained. As it happens in the contralateral case, both positions may be submitted to several oblique motions.
DISCUSSION
Verifying in the foam model what happens next to the muscle, we can get a perfect tridimensional view of the whole assemblage and of the structural possibilities of the island flap several possible positions. The first torsion occurs sistematicaliy in all groups and corresponds to the muscle base next to the costal grid at the upper epigastric artery outlet. In spite of being at 180º, it is smoothly performed and do not cause any hindrance to the mold adaptation; the same phenomenon automaticaliy occurs in vivo. In such a position, when we exteriorize the island flap out of the thorax, it will be turned inward. At this rnoment we can detect clear differences between what occurs with the bilateral and the unilateral flaps. With the bilateral mold, to turn the umbilical scar downward, it is enough to turn the whole assemblage to one direction or to the other. We have observed that this can be accomplished positioning the contralateral muscle behind or in front of the homolateral one. With this procedure, the skin (foam) island is exteriorized and the navel turns downward. If the rotation positions the contralateral muscle behind the homolateral one, we achieve a better reach for the extremity, which will go to the infraclavicular and axillary area - which means a better obliquity. If the contralateral muscle passes in front of the homolateral one, however, we get a clear limitation for this reach, because the torsion imposed to the perforating vessels area is much too great. Opting to position the navel upward, we will get from the transversal position 2112 up to the complete verticalization, passing by several clockwise (in cases of right side deformities) or anticlockwise (left side deformities) obliquities. In this model, the obliquities contrary to the ones already described were extremely limited by the rotation arc of the contralateral muscle - which means the homolateral muscle presents a better reach always to the axillary and infraclavicular area with less tension. The muscles eventually adapt in a parallel position, eliminating the "elbow" in the dangerous area of the perforating vessels, an "elbow" which clearly appears in the totaliy transverse position and may cause problems of venous return by compression. Several authors like us, among them MAXWELL, prefer the almost vertical oblique position with the umbilical scar turned upward and inward, for this procedure provides an excellent infraclavicular and axillary filling and the possibility of flap excess at the lower portions of the new breast. The umbilical scar defect must be discarded as parameter for the shaping, for in the great majority of cases it will be buried under the thoracic skin. The position 2112 with the navel downward, on its turn, will present the strong limiting factor of the contralateral muscle passing in front of the homolateral one; therefore, its positioning behind the homolateral muscle is preferable.
Using the contralateral unilateral mold, we observe that, exteriorizing the skin with the navel turned downward, the position 312 is obtained without any muscular "elbow" at the perforating vessels area, and we can perform clockwise and anticlockwise oblique positionings, depending on the case (for the left side deformities). The same principle applies to the right side defects, but for them the position must be the 213 one. With the contralateral muscle, we observe that the areas 3 and 1 are always medialiy positioned on the thorax and may easily fill the new breast lower portions which will provide the whole mammary cone, without loosing height for the axillary and infraclavicular area. These positions 312 and 213 are obtained by the mere complete rotation of the island flap which was turned inward, both to the left and to the right. The area 2 remains compulsorily turned upward and/or outward. However, if we exteriorize the skin (foam) island with the navel positioned upward, it will mean the position 213 for a left side deformity and 312 for a right side defect. Thus we once more obtain a dangerous muscular "elbow" next to the perforating vessels, but this "elbow" may be undone by oblique motions in accordance with the case characteristics. In the case of a right side homolateral muscle, exteriorizing the island flap with the navel turned downward we get the position 213, without any "elbow", but with the largest tissue volume at the lateral portions of the new breast. As the reach is much greater, however, we may apply oblique motions to obtain several possible positionings. If we opt for the navel turned upward we get the position 312, in which the muscular "elbow" occurs again and has to be undone; in this case, the oblique motion must be performed with the area 2 turned upward and outward. This is an excellent position which provides easy shaping; however, the flap reach is slightly reduced, which does not represent a limiting factor. With the unilateral flaps, we must consider the umbilical scar positioning as an important factor in the future shaping of the new breast; in such cases, we often work with less tissue and eventually leave the scar exposed, which means we do not bury it under the thorax skin similarly to what occurs with the bilateral flaps. In such contingencies it is always preferable to leave the scar turned downward, aiming at a future refinement.

Fig. 10. In vivo.

Fig. 11. In vivo.
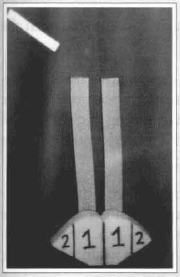
Fig. 12. Foam model for bilateral rotation. It starts on position 2112.
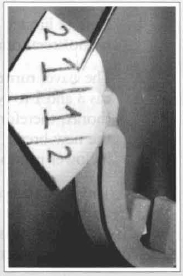
Fig. 13. Vertiealized upward rotation. Muscles in a parallel position without torsion.
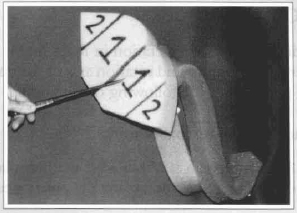
Fig. 14. Oblique upward rotation. Muscles in a parallel position without torsion.
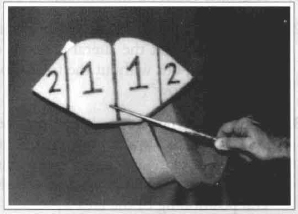
Fig. 15. Transverse upward rotation with the navel turned upward. Dangerous. Pedicle torsion in "knee" behind the flap.
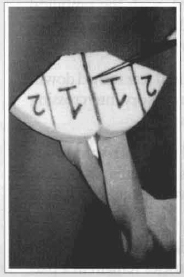
Fig. 16. Upward rotation with the navel turned downward. The contralateral muscle passes behind the homolateral one. Greater reach at the armpit.
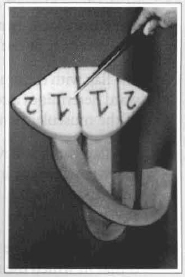
Fig. 17. Upward rotation with the navel turned downward. The contralateral muscle passes in front of the homolateral one. Reduced reach at the armpit.
CONCLUSION
The tridimensional interpretation in foam molds for the several positionings and rotation ares of the tram-flap has provided us the following observations:
For the bilateral rectoabdominal:
1. A greater reach is obtained if the homolateral extremity is superolaterally positioned;
2. The contralateral muscle must pass behind the homolateral one when the option is for the umbilical scar turned downward;
3. When the contralateral muscle passes in front of the homolateral one, with the umbilical scar turned downward, it limits the reach of the extremity at the armpit;
4. The flap with the umbilical scar turned downward determines a compulsory intercrossing of the muscular bands;
5. The flap with the navel turned upward, when transverse, determines a dangerous muscular "elbow" at the level of the perforating vessels;
6. The most adequate tridimensional position is that in which the muscles remain in a parallel positioning with an obliquity of the perforating vessels area, and the navel is superointernally positioned, with the homolateral extrernity turned upward;
7. The umbilical scar must not be considered by itself in the choice of the best aesthetical position, for it may result in the pedicle strangling and future venous suffering;
8. The option for the umbilical scar turned downward must be performed with the contralateral muscle passing behind the homolateral one;
9. The first and second muscle torsions are not enough to cause vascular insufficiency; what causes it is the "elbow" formation at the perforating vessels area, or the forced crossing of the muscular bands.
For the contralateral unilateral rectoabdominal:
1. A more limited reach as compared with the homolateral one;
2. The navel turned downward causes the areas 3 and 1 to be medially positioned on the thorax, therefore facilitating the shaping of the new breast, which needs more tissue at its lower portions;
3. The navel turned downward provides a better reach to the flap with no "elbow" at the perforating vessels area - exactly the opposite of what occurs when it is turned upward;
4. In addition to limiting the flap, the navel turned upward positions the areas 3 and 1 laterally, impairing the shaping.
For the homolateral unilateral rectoabdominal:
1. A greater reach on the thorax;
2. The navel turned downward positions the areas 3 and 1 at the lateral portions of the new breast, but without the formation of a vascular "elbow";
3. The navel turned upward positions the areas 3 and 1 at the lower portions of the new breast, but with an "elbow" which must be undone by an oblique motion and the lateral positioning of the area 2;
4. Even with the navel turned upward - which determines the formation of a vascular "elbow" and shortens the reach - the shaping is always possible;
5. With the unilateral flaps in general, the navel turned downward must be considered at the shaping, for we often do not count on a sufficient tissue amount to bury it under the thoracic skin. In such circumstances the contralateral flap presents more advantages, in spite of a shorter reach.
REFERENCES
1. DREAVER, M. J. - Total Breast Reconstruction. Ann. Plast. Surg. 7:54, 1981.
2. HARTRAMPF, C. R.; SCHEFLAN, M. and BLACK, P. W. - Breast Reconstruction With a Transverse Abdominal Island Flap. Plast. and Reconstruct. Surg. 69:216, 1982.
3. VIEIRA, R.; CHVEID, M. and KOGUT, J. - Breast Reconstruction With a Rectoabdominal Flap. Simpósio de Abdominoplastia em São Paulo, Anais 1982.
4. HOLMSTRÖM, H. - The Free Abdominoplasry Flap and Its Use in Breast Reconstruction: An Experimental Study and Clinical Case Report. Scand. J. Plast. Reconstruct. Surg. 13:423, 1979.
5. ROBBINS, T. H. - Rectus Abdominis Myocutaneous Flap for Breast Reconstruction. Austr. N. Z. J. Surg. 49:527, 1979.
I - Plastic Surgeon and Mastologist, National Cancer Institute (INCa) - Rio de Janeiro, Brazil
Plastic Surgeon and Mastologist, "Hospital Israelita Albert Sabin"
Titular Member, Brazilian Sociery of Plastic Surgery
Titular Member, Brazilian Mastology Society
National Cancer Institute - Rio De Janeiro, Brazil
Reconstructive Plastic Surgery Service
Address for Correspondence:
Mauricio Chveid, MD
Praça da Cruz Vermelha, 23 - Centro
20230-130 - Rio de Janeiro - RJ - Brazil


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter