

Original Article - Year 2021 - Volume 36 -
Impact of the COVID-19 virus pandemic on hospitalizations for skin cancer treatment in Brazil
Impacto da pandemia do vírus COVID-19 nas internações para tratamento de câncer de pele no Brasil
ABSTRACT
Introduction: COVID-19 virus infection was a severe health impact in 2020. The direct repercussion is easily measured through its morbidity and mortality rates. Its indirect repercussion on health is still little measured, and this is the objective of this study.
Methods: To determine the number of hospitalizations for general treatments, for the treatment of neoplasms and malignant skin cancer in the SUS, from 2008 to 2020, in the department of informatics of the SUS.
Results: The parallelism of the data referring to the three groups selected above allowed to observe a drastic reduction in the number of hospitalizations in the SUS between the same months of 2019 and 2020: a decrease of 10.60% in general hospitalizations, 58.65% in hospitalizations for neoplasia and 156% in hospitalizations for malignant skin cancer. The reduction gradually worsened in 2020 from January. In June 2020, the number of hospitalizations for skin cancer treatment reflected values from 12 years ago.
Conclusion: The follow-up of the historical series of hospitalizations in the SUS provides a tangible value that serves as a basis for understanding the direction of health measures. The indirect implications of COVID-19 may have an outcome as tragic as its mortality, as they impact specialized health services availability. Services of great specialization such as hospital cancer treatment attend complex cases, and their unavailability may reflect an increase in mortality from these causes - an indirect impact of COVID-19.
Keywords: Coronavirus infections; Skin neoplasms; Melanoma; Basal cell carcinoma; Neoplasms.
RESUMO
Introdução: A infecção pelo vírus COVID-19 é um impacto severo à saúde no ano de 2020. A repercussão direta é facilmente mensurada através de suas taxas de morbidade e mortalidade. Sua repercussão indireta na saúde ainda é pouco mensurada e este é o objetivo deste estudo.
Métodos: Determinar os números de internações para tratamentos gerais, para tratamento de neoplasias e para câncer de pele malignos no SUS, de 2008 a 2020, no departamento de informática do SUS.
Resultados: O paralelismo dos dados referentes aos três grupos acima selecionados permitiu observar uma redução drástica no número de internações no SUS entre os mesmos meses de 2019 e 2020: queda de 10,60% nas internações gerais, 58,65% nas internações por neoplasia e 156% nas internações por câncer de pele maligno. A redução agravou-se gradativamente no ano de 2020 a partir do mês de janeiro. No mês de junho de 2020, os números de internações para tratamento de câncer de pele refletem valores de 12 anos atrás.
Conclusão: O acompanhamento da série histórica de internações no SUS fornece um valor palpável que serve como base para se compreender o direcionamento das medidas de saúde. As implicações indiretas da COVID-19 podem ter um desfecho tão trágico quanto a sua mortalidade, pois repercutem na disponibilidade de serviços de saúde especializados. Serviços de grande especialização como o tratamento de câncer em caráter hospitalar atendem casos complexos e sua indisponibilidade pode refletir em aumento de mortalidade por estas causas - um impacto indireto da COVID-19.
Palavras-chave: Infecções por coronavírus; Neoplasias cutâneas; Melanoma; Carcinoma basocelular; Neoplasias
INTRODUCTION
Skin neoplasms are a broad group of diseases, and malignant neoplasms receive greater clinical emphasis due to their epidemiology and outcomes that are largely preventable with early treatment. Skin cancers are the most common neoplasms globally, with an estimated 2 to 3 million incidences in the non-melanoma type and 132,000 in melanoma per year1. It is estimated that 1 in 3 diagnosed cancers occurs on the skin1.
Brazil mirrors global epidemiology and has an estimated annual incidence of 185,380 cases by 2020, with 4,120 deaths in 2018. In this scenario, skin cancer is the neoplasm with the highest annual incidence2,3.
Neoplasms are the second leading cause of mortality in Brazil, but most skin cancers have a good prognosis when diagnosed and treated early2. This is why maintaining and improving cancer approach programs is important.
The year 2020 is being marked by the fatalities and changes required to cope with the COVID-19 virus. Therefore, this study’s importance is justified since it is necessary that, given the impact on skin neoplasms’ treatment due to the influence of the COVID-19 pandemic, it is important to look for means that minimize its consequences.
OBJECTIVES
This work aims to measure the evolution of hospitalizations in general for neoplasms and skin cancer in the period 2008-2020 and, from these data, quantify the impact on the number of hospitalizations for skin cancer treatment.
METHODS
An epidemiological study was conducted in the DATASUS database (TABNET) covering Brazilian municipalities from January 2008 to June 2020 regarding hospital admissions, elective and urgent hospitalizations, for the treatment of chapters ICD-10, “malignant neoplasm of the skin,” and “other malignant neoplasms of the skin”4.
This was followed by normative resolution number 510 of April 7, 2016, of the Ministry of Health, which defines the researches that use public access information, made in databases, whose information is aggregated, without the possibility of individual identification and do not need to go through the research ethics committee (CEP)5.
The information system of the Ministry of Health has already published data for the first six months of 2020 and, for this reason, was the period of choice determined to create parallelism with previous years regarding the number of hospitalizations in the chosen groups, the character of hospitalization (elective x urgency) and percentage evolutions. These data were analyzed by the authors of this study in meetings at Santa Casa de Montes Claros.
RESULTS
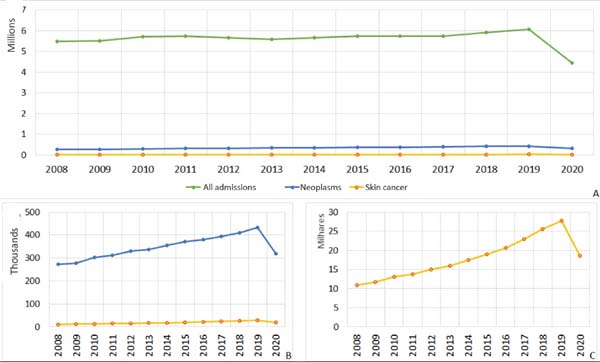
The hospitalizations performed in the Unified Health System, between January and June 2008 and 2020, were tabled and analyzed, resulting in figures 1A, 1B and 1C and Table 1. There was an increase in the total number of hospitalizations for all causes from 2008-2019: the total number of hospitalizations increased 10.60%, the number of hospitalizations for neoplasms increased 58.65%, and the total number of hospitalizations for skin cancer increased by 156.24%.
| Year | All admissions | Neoplasms | Skin cancer |
|---|---|---|---|
| 2008 | 5.495.649 | 272.415 | 10.820 |
| 2009 | 5.518.042 | 278.240 | 11.639 |
| 2010 | 5.717.400 | 302.015 | 13.095 |
| 2011 | 5.730.321 | 310.662 | 13.702 |
| 2012 | 5.666.376 | 330.234 | 14.947 |
| 2013 | 5.596.107 | 335.941 | 16.000 |
| 2014 | 5.654.255 | 354.641 | 17.426 |
| 2015 | 5.747.574 | 371.718 | 18.954 |
| 2016 | 5.746.614 | 380.344 | 20.680 |
| 2017 | 5.747.733 | 393.835 | 22.933 |
| 2018 | 5.921.025 | 411.028 | 25.592 |
| 2019 | 6.077.975 | 432.190 | 27.725 |
| 2020 | 4.455.777 | 319.297 | 18.567 |
The first six months of 2020 showed a numerical reduction in hospitalizations in the three groups compared to the same months of 2019: general hospitalizations reduced by 26.69%, hospitalizations for all neoplasms reduced by 26.12%, while malignant skin neoplasms reduced by 33.03%.
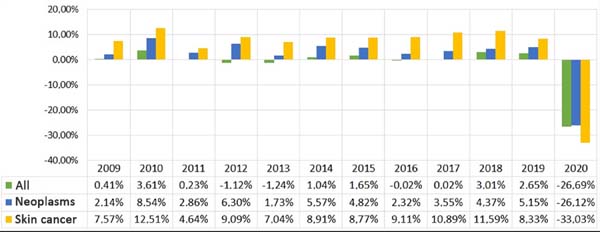
The percentage changes over the previous year, in the first six months of each year, 2008-2020, are recorded in figure 2.
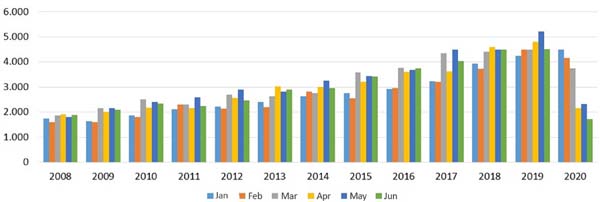
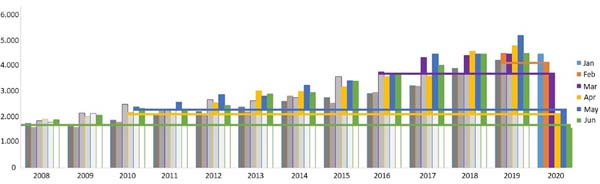
The number of hospitalizations for skin cancer studied in the first six months of the period is shown in Figure 3 and Table 2.
| Year 2008 |
January 1.750 |
February 1.591 |
March 1.867 |
April 1.917 |
May 1.800 |
June 1.895 |
|---|---|---|---|---|---|---|
| 2009 | 1.638 | 1.591 | 2.155 | 2.017 | 2.149 | 2.089 |
| 2010 | 1.877 | 1.798 | 2.510 | 2.177 | 2.395 | 2.338 |
| 2011 | 2.119 | 2.294 | 2.310 | 2.165 | 2.581 | 2.233 |
| 2012 | 2.222 | 2.128 | 2.690 | 2.561 | 2.889 | 2.457 |
| 2013 | 2.409 | 2.200 | 2.640 | 3.027 | 2.821 | 2.903 |
| 2014 | 2.627 | 2.821 | 2.760 | 3.003 | 3.257 | 2.958 |
| 2015 | 2.764 | 2.551 | 3.588 | 3.199 | 3.442 | 3.410 |
| 2016 | 2.918 | 2.970 | 3.774 | 3.593 | 3.683 | 3.742 |
| 2017 | 3.234 | 3.214 | 4.336 | 3.619 | 4.490 | 4.040 |
| 2018 | 3.923 | 3.714 | 4.412 | 4.585 | 4.478 | 4.480 |
| 2019 | 4.235 | 4.492 | 4.491 | 4.800 | 5.205 | 4.502 |
| 2020 | 4.482 | 4.150 | 3.738 | 2.156 | 2.328 | 1.713 |
Source: DATASUS, 20201.
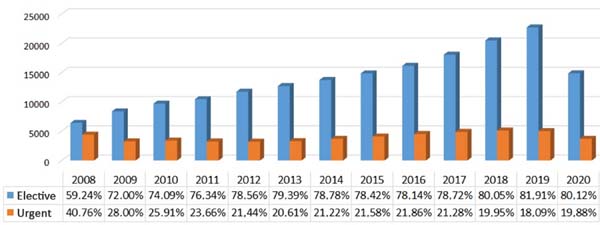
Figure 4 shows the evolution of elective and urgent hospitalizations for skin cancer treatment from January to June 2008 to 2020.
DISCUSSION
The direct and indirect impact of COVID-19 infection is not yet fully known. The possible theorized indirect results are reduced hospitalizations to other diseases due to the scarcity of SUS resources or its contingency. Another French study, still in progress, confirms in its preliminary reports a similar trend, with a drastic reduction in terms of screening (-86%), diagnosis (-39%) treatment (-30%) when compared to the same period of 20196.
The analysis of figures 1 and 2 and table 1 revealed that there was an increase in hospitalizations in the three groups from 2008 to 2019: general hospitalizations increased by 582,326 (10.60%), hospitalizations for cancer in general increased by 159,775 (58.65%), and hospitalizations for skin cancer increased by 16,905 (156.24%).
The comparison of the first six months of 2019 and 2020 revealed a reduction in the total and the proportional number of hospitalizations: general hospitalizations decreased by 1,622,198 (26.69%), cancer in general in 112,893 (26.12%) and skin cancer in 9,158 (33.03%).
The drop in the number of hospitalizations shows how skin cancer treatment may have been affected, similar to what occurred in England, where there was a statistically significant reduction in skin cancer diagnoses of 68.61%7.
Monthly hospitalizations for skin cancer in 2020 gradually reduced. January 2020 still increased compared to 2019, while February, March, April, May and June 2020 were equivalent to the number of hospitalizations with the same months of 2019, 2016, 2010 and before 2008. The impact of this change is best understood in Figure 5.
In line with other international projections, this trend in reducing the number of cases treated may lead to a late diagnosis, with a worse prognosis in this cancers8.
Figure 4 shows that the rates of elective and urgent surgeries maintained their general downward trend from 2008 (40% of urgent surgeries) until 2020 (19.88%), with small variances, which shows no change to urgency in elective cases.
Given the absence of adequate diagnosis and treatment, there can be a considerable increase in severity cases, according to studies by Tejera-Vaquerizo et al. (2020) 9, which estimated increased size and depth of squamous cell carcinoma and melanomas in Spain during the pandemic. It was noticed in this study when there is a delay of 3 months in the diagnosis the projection and reduction of the survival in 5 years of 5.2% for squamous cell carcinoma (SCC) and up to 30.2% months for the melanoma.
CONCLUSION
This study shows that SUS resources’ contingency led to a reduction in the total number of hospitalizations, returning to lower monthly levels than 12 years ago. This isolated data is an important indication of the indirect impact of the COVID-19 pandemic, as it represents real, measurable and up-to-date data on the change of approaches to other pathologies in this particular period.
Due to the delay in the various stages of approach to skin cancers, efforts should be made to minimize the pandemic’s impact. In this context, we can highlight the standardization of conducts, according to guidelines developed by institutions, such as the National Comprehensive Cancer Network10. Besides, it is necessary to facilitate the patient’s access to the health system, and telemedicine, cited in several sources as a facilitator of the follow-up of these cases, is necessary 7,11,12.
In the specific case of skin cancer requiring reconstruction in a hospital environment (and not just outpatient), these are patients with complex lesions. A few months may undoubtedly represent the difference between curative surgery or just oncological (palliative) hygiene. Due to acute and chronic diseases, the mortality curves presented in the coming years will attest to the meaning of this fall in hospitalizations.
COLLABORATIONS
|
IFV |
Analysis and/or data interpretation, Data Curation, Formal Analysis, Investigation, Project Administration, Writing - Original Draft Preparation, Writing - Review & Editing |
|
TRWC |
Analysis and/or data interpretation, Conception and design study, Conceptualization, Data Curation, Final manuscript approval, Formal Analysis, Investigation, Methodology, Project Administration, Resources, Supervision, Validation, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing |
|
LRS |
Analysis and/or data interpretation, Conceptualization, Final manuscript approval, Formal Analysis, Writing - Review & Editing |
|
LAT |
Conceptualization, Data Curation, Final manuscript approval, Formal Analysis, Writing - Original Draft Preparation, Writing - Review & Editing |
|
OJDM |
Analysis and/or data interpretation, Conceptualization, Final manuscript approval, Writing - Original Draft Preparation, Writing - Review & Editing |
|
DFS |
Data Curation, Formal Analysis |
|
DSR |
Data Curation, Formal Analysis, Resources, Writing - Review & Editing |
|
PCA |
Data Curation, Formal Analysis, Methodology |
REFERENCES
1. World Health Organization (WHO). INTERSUN: the Global UV project [Internet]. Geneva: WHO; 2020; [acesso em 2020 Ago 20]. Disponível em: https://www.who.int/uv/resources/FAQ/skincancer/en/index1.html
2. Ministério da Saúde (BR). Instituto Nacional de Câncer José Alencar Gomes da Silva (INCA). Câncer de pele não melanoma [Internet]. Rio de Janeiro (RJ): Ministério da Saúde/INCA; 2020; [acesso em 2020 Ago 20]. Disponível em: https://www.inca.gov.br/tipos-de-cancer/cancer-de-pele-nao-melanoma
3. Ministério da Saúde (BR). Instituto Nacional de Câncer José Alencar Gomes da Silva (INCA). Câncer de pele melanoma [Internet]. Rio de Janeiro (RJ): Ministério da Saúde/INCA; 2020; [acesso em 2020 Ago 20]. Disponível em: https://www.inca.gov.br/tipos-de-cancer/cancer-de-pele-melanoma
4. Ministério da Saúde (BR). Departamento de Informática do SUS - DATASUS. Informações de saúde, epidemiológicas e morbidade: banco de dados [Internet]. Brasília (DF): Ministério da Saúde; 2020; [acesso em 2020 Ago 20]. Disponível em: http://tabnet.datasus.gov.br/cgi/deftohtm.exe?sih/cnv/nibr.def
5. Ministério da Saúde (BR). Resolução nº 510, de 7 de abril de 2016. Conselho Nacional de Saúde. O Plenário do Conselho Nacional de Saúde em sua Quinquagésima Nona Reunião Extraordinária, realizada nos dias 06 e 07 de abril de 2016, no uso de suas competências regimentais e atribuições conferidas pela Lei n o 8.080, de 19 de setembro de 1990, pela Lei n o 8.142, de 28 de dezembro de 1990, pelo Decreto n o 5.839, de 11 de julho de 2006. Brasília (DF): Ministério da Saúde; 2020; [acesso em 2020 Ago 20]. Disponível em: https://bvsms.saude.gov.br/bvs/saudelegis/cns/2016/res0510_07_04_2016.html
6. Brugel M, Carlier M, Essner C, Debreuve-Theresette A, Beck MF, Merrouche Y, et al. Dramatic changes in oncology care pathways during the COVID-19 pandemic: The French ONCOCARE-COV study. Oncologist [Internet]. 2020 Out; [citado 2020 Nov 10]; 26(2):e388-e41. Disponível em: https://theoncologist.onlinelibrary.wiley.com/doi/10.1002/onco.13578
7. Andrew TW, Alrawi M, Lovat P. Reduction in skin cancer diagnoses in the UK during COVID-19 pandemic. Clin Exp Dermatol [Internet]. 2020 Ago; [citado 2020 Nov 11]; 46(1):145-6. Disponível em: https://onlinelibrary.wiley.com/doi/full/10.1111/ced.14411
8. Earnshaw CH, Hunter HJA, McMullen E, Griffiths CEM, Warren RB. Reduction in skin cancer diagnosis, and overall cancer referrals during the COVID-19 pandemic. Br J Dermatol [Internet]. 2020 Out; [citado 2020 Nov 08]; 183(4):792-4. Disponível em: https://onlinelibrary.wiley.com/doi/10.1111/bjd.19267
9. Tejera-Vaquerizo A, Cañueto J, Toll A, Santos-Juanes J, Jaka A, Ferrandiz-Pulido C, et al. Estimated effect of COVID-19 lockdown on skin tumor size and survival: an exponential growth model. Actas Dermosifiliogr [Internet]. 2020 Out; [citado 2020 Nov 09]; 111(8):629-38. Disponível em: https://pubmed.ncbi.nlm.nih.gov/32513393/
10. National Comprehensive Cancer Network (NCCN). Advisory statement for non- melanoma skin cancer care during the COVID-19 pandemic [Internet]. Plymouth Metting, PA: NCCN; 2020 Mai; [acesso em 2020 Nov 07]. Disponível em: https://www.nccn.org/covid-19/pdf/NCCN-NMSC.pdf
11. West H. Telemedicine for oncology: delivering on an overdue promise in the COVID-19 era. Front Oncol [Internet]. 2020 Set; [citado 2020 Nov 09]; 10:578888. Disponível em: https://www.frontiersin.org/articles/10.3389/fonc.2020.578888/full
12. Rodin D, Lovas M, Berlin A. The reality of virtual care: Implications for cancer care beyond the pandemic. Healthcare [Internet]. 2020 Ago; [citado 2020 Nov 09]; 8(4):100480. Disponível em: https://www.sciencedirect.com/science/article/pii/S2213076420300798
1. FAMINAS-BH, Faculty of Medicine, Belo Horizonte, MG, Brazil.
2 . Hospital Santa Casa de Caridade de Montes Claros, Plastic surgery, Montes Claros,
MG, Brazil.
3 . Socor Hospital, Plastic Surgery, Belo Horizonte, MG, Brazil.
4 . Faculdades Integradas do Norte de Minas - FUNORTE, Faculty of Medicine, Montes
Claros, MG, Brazil.
5 . Dilson Godinho Hospital, Department of Plastic Surgery, Montes Claros, MG, Brazil.
Corresponding author: Isabella de Fátima Vilela, Avenida Raja Gabaglia , 1123, Luxemburgo, Belo Horizonte, MG, Brazil. Zip Code: 30380-403. E-mail: isaffarma@gmail.com
Article received: September 15, 2020.
Article accepted: November 19, 2020.
Conflicts of interest: none










 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter