

Original Article - Year 2021 - Volume 36 -
Enlarged blepharoplasty: treating the upper two-thirds of the face
Blefaroplastia ampliada: tratando os dois terços superiores da face
ABSTRACT
Introduction: Patients may show signs of facial aging still in the early stages of life when complex surgical procedures are not sought, especially if they result in larger scars. These signals should be detected and treated appropriately for effective rejuvenation.
Methods: In the last 23 years,338 patients have undergone upper blepharoplasty associated with transpalpebral elevation of the eyebrows and myectomies of corrugators. They also received a mid-facial facelift through a lower blepharoplasty incision, with a detachment of the retaining orbital ligaments and repositioning an extensive flap of the orbicularis muscle in the superolateral direction. Canthopexy was routinely performed.
Results: Simultaneous rejuvenation of the upper two-thirds of the face is performed through simple blepharoplasty incisions, and this systematization is not found in the current literature. Patients were satisfied with the results, and routine canthopexy effectively prevented lower eyelid positioning defects. The most common complications were temporary paraesthesia (frontal and scalp regions) and chemosis in the lateral and lower aspects of the conjunctiva. In a retrospective review of 139 procedures performed between 2010 and 2019, the temporary scleral show was observed in 15 cases (10.8%) and a mild ectropion in 1 case (0.72%), treated conservatively. Two cases of chemosis (1.44%) and one hematoma (0.72%) required surgical treatment.
Conclusion: Enlarged blepharoplasty is safe, allows direct vision of manipulated periorbital structures, does not require long or expensive instrumental training. The authors achieve aesthetic results that impress by the rejuvenation of the upper 2/3 of the face and the lasting effect.
Keywords: Blepharoplasty; Ritidoplasty; Plastic surgery; Myocutaneous flap; Oculomotor muscles.
RESUMO
Introdução: Os pacientes podem apresentar sinais de envelhecimento facial ainda em fases iniciais da vida, quando procedimentos cirúrgicos complexos não são procurados, especialmente se resultarem em cicatrizes maiores. Estes sinais devem ser detectados e tratados adequadamente para um rejuvenescimento eficaz.
Métodos: Nos últimos 23 anos, 338 pacientes foram submetidos à blefaroplastia superior associada à elevação transpalpebral das sobrancelhas e miectomias dos corrugadores. Eles também receberam um lifting médio-facial através de uma incisão de blefaroplastia inferior, com descolamento dos ligamentos retentores orbitais e reposicionamento de um extenso retalho do músculo orbicular em direção superolateral. Cantopexia foi realizada rotineiramente.
Resultados: O rejuvenescimento simultâneo dos dois terços superiores da face é realizado através de incisões simples de blefaroplastia e essa sistematização não é encontrada na literatura atual. Os pacientes ficaram satisfeitos com os resultados e a cantopexia de rotina efetivamente preveniu defeitos de posicionamento da pálpebra inferior. As complicações mais comuns foram parestesia temporária (regiões frontal e escalpo) e quemose nos aspectos lateral e inferior da conjuntiva. Em uma revisão retrospectiva de 139 procedimentos realizados entre 2010 e 2019, scleral show temporário foi observado em 15 casos (10,8%) e um leve ectrópio em 1 caso (0,72%), tratados de forma conservadora. Dois casos de quemose (1,44%) e um hematoma (0,72%) necessitaram de tratamento cirúrgico.
Conclusão: A blefaroplastia ampliada é segura, permite a visão direta das estruturas periorbitais manipuladas, não requer treinamento longo ou instrumental caro. Os autores alcançam resultados estéticos que impressionam pelo rejuvenescimento dos 2/3 superiores da face e pelo efeito duradouro.
Palavras-chave: Blefaroplastia; Ritidoplastia; Cirurgia plástica; Retalho miocutâneo; Músculos oculomotores
INTRODUCTION
Gravitational forces and facial mimicry cause anatomical changes that result in aging1. For example, the action of the corrugator muscles favors the ptosis of the eyebrow, which causes a pseudo cutaneous excess of the upper eyelid1. Classic blepharoplasty, without eyebrow elevation, can make your ptosis more evident, as the frontal muscle will not be stimulated for suspension1,2.
On the aged face, the skin of the lower eyelid stretches, exposing the lower orbital margin and herniations of orbital fat3. The elongated and excavated lower eyelid combines with the deepening of the nasojugal and nasolabial line3,4 and with the decrease in skin vitality1,3, resulting in senile physiognomy. These changes should be addressed to achieve better aesthetic results.
There are many techniques described for eyebrow elevation: direct skin excisions in supraorbital, temporal, or frontal areas, coronal lifting, frontal endoscopic elevation and transpalpebraal approaches4-6. The middle third of the face approach is usually done by time incisions, before and after the ear, to tract the skin and the Superficial Musculoaponeurotic System (SMAS), which can result in visible scars, hairline displacement, or alopecia.
The treatment of the structures mentioned here is described only with the incisions of the upper and lower blepharoplasties.
OBJECTIVE
Describe a surgical procedure of the periorbital region, which allows the management of the upper two-thirds of the face in a single surgical procedure, using only blepharoplasty incisions.
Present a 10-year review of complications related to the technique.
METHODS
From 1996 to 2019, 338 patients with signs of aging in the upper two-thirds of the face (11.8% men and 88.2% women) underwent upper blepharoplasties associated with the transpalpebral suspension of the eyebrows and myectomy of the glabella muscles. Also, lower blepharoplasties associated with a mediofacial survey with a detachment of orbital ligaments, repositioning and fixation of the orbicularis muscle of the eyes in the superolateral direction7,8. In addition, canthopexy was routinely performed, and canthoplasty was performed when necessary.
All patients underwent standard preoperative evaluation. The surgeries were invariably bilateral and photographic records were performed before surgery and 6 and 12 months later.
This study was submitted to the research ethics committee (COEP) from Hospital Felício Rocho/MG, via Plataforma Brazil, on 07/31/2021, with CAAE designated 50441821.4.0000.5125.
Markings
With the patient lying down, the frontal dissection area is marked as an arch over the eyebrow, 2.5cm long. A medial triangle delimits the area corresponding to the supraorbital and supratrochlear nerves (Figure 1).

The upper eyelids' lower margin of skin resection is marked following the upper eyelid groove, from the medial corner to approximately 0.5cm of the lateral palpebral fissure, where a periorbital wrinkle is followed by about 2.0cm laterally. The upper margin of skin resection is estimated by pinching after manually positioning the eyebrows at the desired height (Figure 1). The five points in Figure 2 show the fixation locations of the eyebrows.
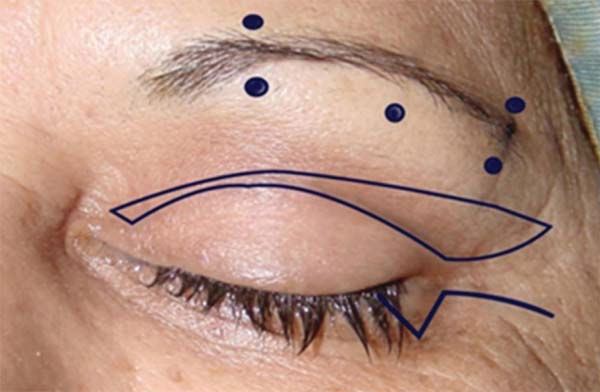
The incision of the lower eyelid is subciliary, and after the lateral corner leans slightly down, following a periorbital rhythm. An equilateral triangle is marked in the side corner, with sides of 0.5cm and a vertex pointing down. Half of its base will be medial to the lateral eyelid fissure and the other half lateral to it9,10. The lateral incisions for upper and lower blepharoplasties should be 0.5 to 1.0 cm apart and slightly divergent10 (Figure 2).
Surgical technique
The procedure can be performed under sedation combined with local anesthesia or general anesthesia. Local anesthesia involves supraorbital, supratrochlear, and infraorbital nerve blocks using 1% ropivacaine. An 80ml solution consisting of 55ml of saline, 20ml of ropivacaine 1%, 1ml of a deposit steroid and 4ml of diluted epinephrine (totaling a concentration of 1:200,000) is prepared. This will be used to infiltrate the eyelids, the upper detachment area and around the lower orbital margin, in a range of 2.0cm.
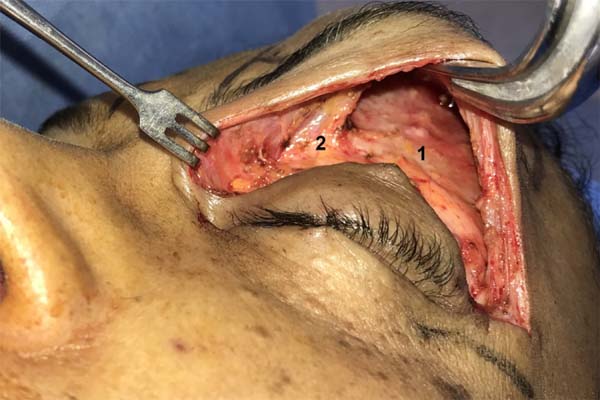
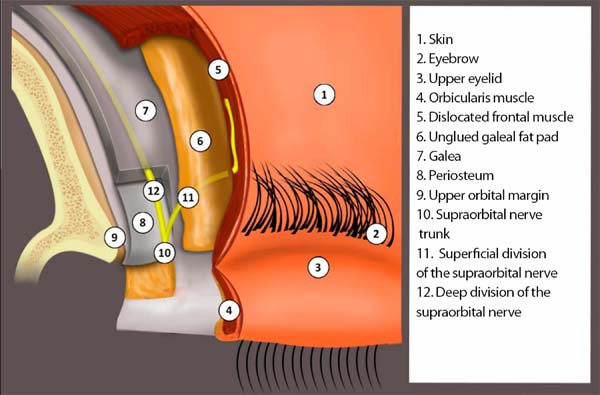
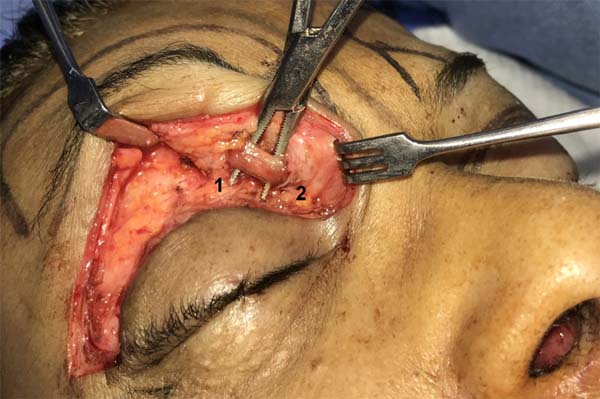
A tarsorrhaphy is performed with nylon 6.0 before resection of skin and orbicularis muscle in the upper eyelid. The fat bags are treated, saving them for use as grafts. The blunt dissection towards the upper orbital margin is performed through the blepharoplasty incision, forming three tunnels: the first at the midpoint of the incision and the other two near the lateral and medial ends. The orbital margin is exposed by fusing the dissection tunnels with scissors, allowing the marked area to be dissected in the supragaleal plane10 (Figure 3). The aponeurotic galea is a strong tissue, preserved in this case to receive the fixation sutures and protect the deep branch of the supraorbital nerve, which is found between the deepest layer of the galea and the periosteum, to which it adheres anatomically in the first 2.0 cm superior to the edge orbit1,10 (Figure 4).
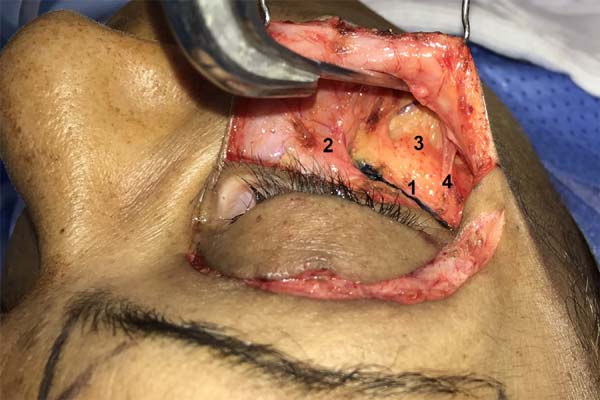
Dissection is laterally limited by the projection of the orbital ligament and its upper extension, the support zone. Adhesions to the galeal adipose cushion and frontal muscle are released in approximately 2.5cm1.10 (Figure 4). Medially, supraorbital, and supratrochlear nerves are identified, and corrugating muscles are individualized between them (Figure 5) for minor resection and cauterization10,11. Fat grafts are positioned in muscle resection areas, avoiding depressions2,10,12,13.
The eyebrows are fixed with nylon sutures 5.0 (Figure 2), connecting the cool soft tissues (the needle is passed from its inner surface to near the dermis and returned to the inner surface) to the galea. The sutures should be firm, without excessive tension. The first suture is positioned laterally to the supraorbital nerve and the subsequent one, just below it. The following two sutures are similar but in the projection of the tail of the eyebrow. The fifth and last suture is central10 (Figure 2). The ideal fixation of the eyebrows in women varies from 0.5 to 1.0 cm above the orbital margin; in men, it is along this orbital margin. The sutures form fixation loops that naturally descend with the patient standing; therefore, a higher galeal suture area is marked (1.5 cm from the orbital margin in women) for proper final positioning of the eyebrows (Figure 6).
The incision of the lower eyelid begins laterally, reaching the marked triangle. The blunt dissection under the orbicularis muscle is performed with a wide craniocaudal opening of Kelly tweezers, supported on the orbital rim. The pre-tarsal part of the muscle should be preserved along the incision, which proceeds on the subciliary skin, from this triangle up to approximately 2.0 mm from the tear point (Figure 2). Lateral orbicular insertions lower than the bone margin (orbital retention ligaments - ORL) are taken off, while fibers connected to the medial half of the orbital margin should be preserved (Figure 7). The objective is to expose suborbicular fat (SOOF) inferiorly and laterally and orbital thickening (LOT)14,15. The lower and lateral dissections mentioned extend for approximately 1.5 cm in the thickness of the medial facial fat compartments15, dividing two thin layers of fat: one to be preserved on the periosteum (SOOF) and the other adhered to the orbicularis muscle (medial fat of the cheek and lateral orbital fat)15,16. Dissection is kept superficial to LOT for about 1.0cm laterally). During dissection, branches of the zygomatic-facial nerve are individualized14 (Figure 7).
The fat pockets of the lower eyelid are treated, and a modified canthopexy, inspired by the Lessa9 technique, is routinely performed: a nylon thread 5.0 crosses the fascia and the periosteum of the upper orbital margin, just above the lateral cantal tendon. Next, the needle is passed caudally under the skin and the muscle flap that sequesters upper and lower blepharoplasty incisions, being externalized in the latter. Then, the suture includes the superolateral part of the lower tarsal plate, where it joins the lateral cantal tendon. Finally, the needle returns to the upper incision, repeating the anchorage in the periosteum to complete the node without excessive tension. In secondary surgeries or patients with significant horizontal eyelid laxity, especially the elderly, canthopexy is replaced with a tarsal strip lateral canthoplasty technique.
The skin of the lower eyelid to be resected is calculated, extending the lower vertex of the marked triangle (Figure 2) a few millimeters lower, with medial obliquity. Care should be taken at this stage, calculating to remove a smaller amount of skin than is believed to be excisable. Over the years, this skin has been caudally distended by the weight of the soft tissues of the middle third of the face, which will be repositioned and fixed in a superolateral area. Initially, one may think that all this skin is surplus, but it will retract later, which can contribute to possible complications, such as scleral show and ectropion.
At the end of this incision in the lower eyelid, the skin is temporarily fixed to the medial part of the marked triangle (Figure 2) for medial skin excision. The excised skin strip is always asymmetrical, with a wider lateral part than the medial. Lateral to the triangle fixation, the orbicularis muscle is dissected from the skin7 and resected in its redundant cranial portion (Figure 8). The remaining muscle flap will be fixed with four to five nylon 5.0 sutures in the LOT located immediately under the lateral incision of the skin, starting at a level just below the lateral cantal ligament at the lateral orbital margin.
These sutures efficiently pull the lower eyelid in a superolateral direction, providing the desired mid-third lift with satisfactory support for mediofacial tissues. (Figure 9).
Excess superolateral skin is carefully resected at this time. The lateral incisions of the upper and lower blepharoplasties are 0.5 to 1.0 cm from each other and are slightly divergent (Figure 2). This allows large skin resections in the region with skin flaps of the upper and lower eyelids anchored in these two almost parallel margins. This fact makes it unnecessary to use peripheral incisions to consume this excess skin.
The same surgical steps are performed on the contralateral eyelid, and the skin closure is completed with monofilament nylon 6.0. Postoperative care is like conventional blepharoplasty, except for the greater edema. It is recommended to use cold compresses for 10 minutes, several times in the first 36 hours and then moderately heated bags and lymphatic drainage after the fifth day. We removed the stitches on the fourth or fifth postoperative day.
RESULTS
The procedure successfully achieves rejuvenation of the forehead and middle third of the face. With corrugator myectomy, the glabella wrinkles are attenuated, and the eyebrows move away. Depressions where the corrugator muscles were resected, were avoided with grafts from resected fat bags. There were no complaints about open palpebral fissures.
Eyebrow lifting was effective and was maintained in the long term. The most common intercurrence was bilateral paraesthesia in the frontal and parietal scalp, spontaneously resolved after a few months. In most cases, temporary paralysis of the frontal muscle was observed to varying degrees10.
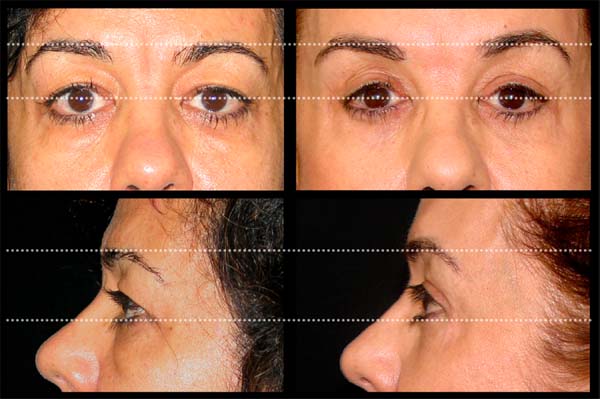
The elongation of the lower eyelids, the skeletonized infraorbital appearance, the prominent nasojugal sulcus, and the malar fat pad ptosis17,18 were adequately treated as the eyelid/cheek junction was raised (Figures 10 to 16). In addition, the repositioning of the orbicularis muscle creates a belt8, which, together with the canthopexy 9,17, avoids complications such as scleral show or ectropion.

There is greater edema in the immediate postoperative period when compared to classical blepharoplasties due to greater dissection and tissue mobilization.
The results were observed in a 23-year follow-up and were stable long-term (Figures 10 to 16).
Intercurrences and complications
We reviewed 139 medical records of operated patients from January 2010 to December 2019. We observed as intercurrence the temporary disconnection of the lateral part of the lower eyelid of the globe treated conservatively. Complications were considered when associated with the scleral show, observed in 15 cases (10.8%); the treatment consisted of elevating the skin from the zygomatic region with Micropore® to the frontal area, on average for 41 days, leading to the proper positioning of the structures during healing. A case of mild ectropion (0.72%) was recorded and thus treated for 180 days. In these 16 complications, we identified as predisposing factors: 4 secondary blepharoplasties, two patients with exophthalmia and associated conjunctivitis in two patients. Chemosis was observed, treated with eye drops with corticosteroids and usually presenting rapid resolution. In 19 patients (13.7%), the chemosis persisted for more than ten days (mean of 47 days), and only two cases (1.44%) required tarsorrhaphy and conjunctival perforations for complete treatment19. The final scars needed revision by lateral retractions in 5 cases (3.6%). A small hematoma (0.72%) on the left lower eyelid was surgically drained.
DISCUSSION
Dermatochalasis is often associated with frontoparietal soft tissue ptosis1,2 and mediofacial tissues17. The aesthetically ideal female eyebrow is arched, located 0.5 to 1.0cm above the upper orbital margin. The male eyebrow is flatter and positioned on or just above this orbital margin20.
Transpalpebral elevation was initially described in 198221, followed by numerous articles2,5,6,10,20,22-25. In 1990, McCord and Doxanas6 described a blepharoplasty associated with the transpalpebral suspension of the eyebrow and the galeal adipose cushion treatment. They recommended less detachment (limiting eyebrow elevation) and no treatment of depressive muscles, favoring ptosis recurrence.
Other techniques proposed this treatment2,11-13,22, allowing less downward traction in the eyebrows. However, they needed other incisions, such as the2,26.
The orbicularis muscle flap showed efficiency in treating the lower eyelid and the middle third of the face7,27,28. The risks are mispositioning of the eyelid and scleral show. A lateral canthopexy, without the lateral cantal ligament section9, helps prevent such complications.
McCord et al. (1998) 8 Combined repositioning of the orbicular is repositioning to subperiosteal detachment of the malar area to treat the middle third of the face. Hester et al. (1998) 3 also treated the middle third by a subciliary incision. After a 5-year experience, the authors described the use of canthopexy in 90% of patients, avoiding poor positioning of the lower eyelid17.
The technique described here treats the upper two-thirds of the face using only upper and lower blepharoplasty incisions. The lower margin of skin excision made in the upper eyelid fold ensures sufficient skin coverage to the eyeball (Figure 2). In addition, the upper orbital margin can be easily accessed through this incision, without injury to any important structure. Next, dissection is performed in the galeal plane, releasing the galeal adipose cushion and the frontal muscle (Figures 3 and 4)1,10.
The described transpalpebral elevation uses a modified McCord and Doxanas (1990)6 technique, with wider dissection of the frontal area in the galeal plane and more fixation sutures, for a more effective ascent. Myectomy of corrugator muscles is associated2,11-13, resulting in smoothed glabella wrinkles and preventing ptosis recurrence. The supraorbital nerve trunk is observed in direct vision, having the superficial branches preserved over the frontal muscle and the deep branches under the galea, which receives the eyebrow fixation sutures. Eyebrow elevation allows reduced excision of the upper eyelid skin, safely achieving good results.
The mediofacial structures are effectively elevated with the repositioning of the orbicularis muscle since the lower fat compartments are connected to it through the SMAS8,14. As a result, the aspect of rounded and aged face changes to an inverted triangle shape, with volumization of the zygomatic regions, leading to a rejuvenated facial expression.
Long-term glucocorticoid infiltrated with anesthetics in the dissection area and postoperatively, oral prednisolone, 40mg/day, five days, provides less edema and more comfort to the patient 29.
CONCLUSION
Enlarged blepharoplasty, as we call it, can contribute to the surgical aesthetic and functional improvement of the periorbital region by managing the upper two-thirds of the face in a single surgical procedure and using only incisions of upper and lower blepharoplasty.
It presented reduced rates of complications, and the outcomes were gratifying and were maintained in the long term.
REFERENCES
1. Knize DM. Anatomic concepts for brow lift procedures. Plast Reconstr Surg. 2009 Dez;124(6):2118-26.
2. Cintra HPL, Basile FV. Transpalpebral brow lifting. Clin Plastic Surg. 2008 Jul;35(3):381-92.
3. Hester TR, Codner MA, McCord CD, Nahai F. Transorbital lower-lid and midface rejuvenation. Oper Tech Plast Reconstr Surg. 1998;5:163-85.
4. Quatela VC, Davis KG. Rejuvenation of the brow and midface. Oper Tech Otolaryngol Head Neck Surg. 1999;10:160-8.
5. Paul MD. The evolution of the brow lift in aesthetic plastic surgery. Plast Reconstr Surg. 2001 Out;108(5):1409-24.
6. McCord CD, Doxanas MT. Browplasty and browpexy: an adjunct to blepharoplasty. Plast Reconstr Surg. 1990 Ago;86(2):248-54.
7. Furnas DW. The orbicularis oculi muscle: management in blepharoplasty. Clin Plast Surg. 1981 Out;8(4):687-715.
8. McCord Junior CD, Codner MA, Hester TR. Redraping the inferior orbicularis arc. Plast Reconstr Surg. 1998 Dez;102(7):2471-9.
9. Lessa S, Sebastiá R, Flores E. Uma cantopexia simples. Rev Soc Bras Cir Plast. 1999;14(1):67-70.
10. Chiari Junior A, Alves TA, Laia PHS, Casali TG, Fleury DPC. Blefaroplastia: elevação transpalpebral das sobrancelhas. Rev Bras Cir Plast. 2014;29(1):44-9.
11. Knize DM. Transpalpebral approach to the corrugator supercilii procerus muscles. Plast Reconstr Surg. 1995 Jan;95(1):52-62.
12. Guyuron B, Michelow BJ, Thomas T. Corrugator supercilii muscle resection through blepharoplasty incision. Plast Reconstr Surg. 1995 Abr;95(4):691-6.
13. Guyuron B. Corrugator supercilii resection through blepharoplasty incision. Plast Reconstr Surg. 2001 Fev;107(2):606-7.
14. Zide BM. The lower lid and beyond. In: Zide BM, Jelks GW, eds. Surgical anatomy around the orbit: the system of zones. Philadelphia: Lippincott Williams & Wilkins; 2006. p. 43-57.
15. Gierloff M, Stöhring C, Gassling V, Açil Y, Wiltfang J. Aging changes of the midfacial fat compartments: a computed tomographic study. Plast Reconstr Surg. 2012 Jan;129(1): 263-73.
16. Rohrich RJ, Pessa JE. The fat compartments of the face: anatomy and clinical implications for cosmetic surgery. Plast Reconstr Surg. 2007;119(7):2219-27.
17. Hester TR, Codner MA, McCord CD, Nahai F, Giannopoulos A. Evolution of technique of the direct transblepharoplasty approach for the correction of lower lid and midfacial aging: maximizing results and minimizing complications in a 5-year experience. Plast Reconstr Surg. 2000 Jan;105(1):393-406.
18. McCord CD, Boswell CB, Hester TR. Lateral cantal anchoring. Plast Reconstr Surg. 2002 Jul;112(1):222-39.
19. Weinfeld AB, Burke R, Codner MA. The comprehensive management of chemosis following cosmetic lower blepharoplasty. Plast Reconstr Surg. 2008 Ago;122(2):579-86.
20. Codner MA, Kikkawa DO, Korn BS, Pacella SJ. Blepharoplasty and brow lift. Plast Reconstr Surg. 2010 Jul;126(1):1-17.
21. Sokol AB, Sokol TP. Transblepharoplasty Brow Suspension. Plast Reconstr Surg. 1982 Jun;69(6):940-4.
22. Langsdon PR, Metzinger SE, Gllickstein JS, Armstrong DL. Transblepharoplasty brow suspension: an expanded role. Ann Plast Surg. 2008 Jan;60(1):2-5.
23. Niechajev I. Transpalpebral browpexy. Plast Reconstr Surg. 2004 Jun;113(7):2172-80.
24. Tyers AG. Brow lift via the direct and trans blepharoplasty approaches. Orbit. 2006 Dez;25(4):261-5.
25. Zarem HA. Browpexy. Aesth Surg J. 2004;24:368-72.
26. Knize DM. Limited-incision forehead lift for eyebrow elevation to enhance upper blepharoplasty. Plast Reconstr Surg. 2001 Ago;108(2):564-7.
27. Adamsom JE, McCraw JB, Carraway JH. Use of a muscle flap in lower blepharoplasty. Plast Reconstr Surg. 1979 Mar;63(3):359-63.
28. Labandter HP. Use of the orbicularis muscle flap for complex lower lid problems: a 6-year analysis. Plast Reconstr Surg. 1995 Ago;96(2):346-53.
29. Lai I, Batra RS. Blepharoplasty. In: Murad A, ed. Evidence-based procedural dermatology. 2nd ed. Amsterdam: Springer; 2019. p. 419-42.
1. Federal University of Minas Gerais, Belo Horizonte, MG, Brazil.
Corresponding author: Armando Chiari Júnior, Rua Herculano de Freitas, nº 58, Conj. 110 - Gutierrez, Belo Horizonte, Minas Gerais, Brazil, Zip Code 30441-039. E-mail: chiari@chiari.com.br / drsergiorodrigues@gmail.com
Article received: November 17, 2020.
Article accepted: May 18, 2021.
Conflicts of interest: none.



























 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter