

Original Article - Year 2021 - Volume 36 -
Augmentation mammoplasty by subfascial technique
Mamoplastia de aumento pela técnica subfascial
ABSTRACT
Introduction: The implantation technique of subfascial silicone prostheses described by Graf in 2003 has advantages over submuscular and subglandular techniques. Unlike the techniques already described, the prosthesis is implanted in the aponeurosis of the pectoral muscle, providing better aesthetic results and fewer complications in the postoperative period.
Objectives: The present study aims to describe the use of breast implants in the subfascial plane and analyze the rates of complications of patients undergoing this procedure.
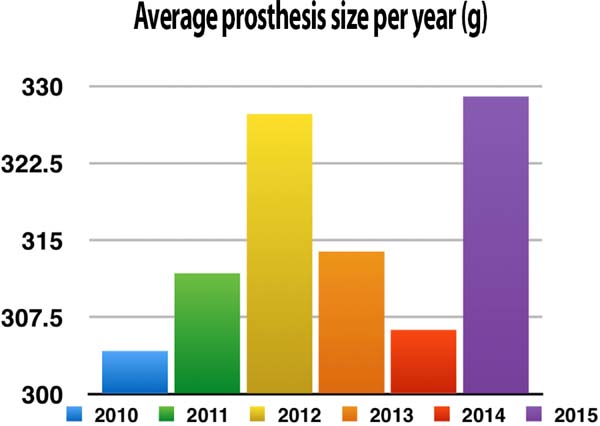
Methods: A retrospective study by analyzing electronic medical records of 233 patients who underwent augmentation mammoplasty with subfascial detachment. Patients who underwent other implantation techniques of prostheses, mastopexy and who used different sizes of prostheses were excluded. Results: Most patients opted for the incision performed in the inframammary groove; the size of the prostheses increased over the period studied, and only one complication was reported postoperatively.
Conclusion: Plastic surgeons have increasingly used the subfascial technique because it presents satisfactory aesthetic results and low rates of complications, as shown in the study, becoming a differentiated option for patients who will perform augmentation mammoplasty.
Keywords: Mammoplasty; Plastic surgery; Breast implant; Methods; Silicone prosthesis
RESUMO
Introdução: A técnica de implantação de próteses de silicone subfascial descrita por Graf, em 2003, apresenta vantagens em relação as técnicas submuscular e subglandular. Diferente das técnicas já descritas, a prótese é implantada na aponeurose do músculo peitoral, proporcionando melhores resultados estéticos e menos complicações no período pós-operatório.
Objetivos: O presente estudo tem como finalidade descrever o uso do implante mamário no plano subfascial, além de analisar os índices de complicações de pacientes submetidos a este procedimento.
Métodos: Estudo retrospectivo através da análise de prontuário eletrônico de 233 pacientes que realizaram mamoplastia de aumento com descolamento subfascial. Foram excluídas as pacientes que realizaram outras técnicas de implantação de próteses, mastopexia e que utilizaram tamanhos diferentes de próteses.
Resultados: A maioria das pacientes optou pela incisão realizada no sulco inframamário, o tamanho das próteses sofreu aumento ao longo do período estudado e apenas uma complicação foi relatada no pós-operatório.
Conclusão: A técnica subfascial vem sendo cada vez mais utilizada pelos cirurgiões plásticos por apresentar resultados estéticos satisfatórios e baixos índices de complicações, como demostrado no estudo, tornando-se uma opção diferenciada para pacientes que realizarão a mamoplastia de aumento.
Palavras-chave: Mamoplastia; Cirurgia plástica; Implante mamário; Métodos; Prótese de silicone
INTRODUCTION
Breast augmentation plastic surgery has become increasingly frequent, stimulated by the great dissemination made by the media and by a change in cultural patterns1.
The use of silicone gel implants to increase the volume of the breasts marked a new era in the history of plastic surgery. Until then, the use of foreign materials to the body almost always resulted in extrusion, infection, or inappropriate appearance. Since 1962, when Cronin and Gerow1 developed the first prostheses, augmentation mastoplasty surgery has evolved. The position of the implant concerning the pectoralis muscle presented variations, starting from pre-pectoral, then subpectoral, more recently subfascial, being placed under the fascia and in a position anterior to the pectoralis major muscle1,2.
Surgeons have increasingly used the performance of augmentation mammoplasty by the subfascial technique. As described by Graf in 20033, it has advantages over other techniques because it provides better aesthetic results both in the short and long term. Studies4-5 state that the subfascial technique has a superior aesthetic result, as the space between the muscle and the fascia smooth the contours of the implant, the post-surgical recovery is faster and less painful, the complication rates become minimal and there are fewer cases of prosthesis displacement due to the action of the pectoral muscles. In addition, these characteristics provide the breast with a natural and homogeneous aspect and are better accepted by patients2,4,6.
OBJECTIVES
The present study aims to describe the use of breast implants in the subfascial plane and analyze the rates of complications of patients undergoing this procedure.
METHODS
This research was approved by the research ethics committee no. 40452620.6.0000.5368. This is a descriptive quantitative retrospective study of a cross-sectional nature, which evaluated the profile of 432 patients who underwent augmentation mammoplasty, through the analysis of medical records, in a plastic surgery clinic in Blumenau/SC, in the period from 2010 to 2015. We excluded from the analysis 199 patients who underwent other techniques of implantation of silicone prostheses, patients who underwent mastopexy and those who required different sizes of prosthesis. The study included 233 patients who opted for the subfascial surgical implantation technique regardless of the size of the prosthesis used and the incision site. All patients were operated on by the same surgeon and with the same surgical technique. The implants used were Allergan®.
The data used were age, prosthesis size, year in which the surgery was performed, surgical incision site, chosen prosthesis shape and occurrence of complications. A literature review was also performed comparing submuscular, subglandular and subfascial surgical techniques, based on scientific articles from the PubMed, BVC and SciELO databases.
Descriptive statistics were performed to obtain values of mean, standard deviation, and absolute and relative frequency values to analyze the data. The data were analyzed in the statistical software SPSS IBM® version 20.0.
Surgical complications were all present in the patients' medical records.
The markings were performed with the patient standing, measuring the current base of the breast and the desired base, the distance from the nipple to the inframammary groove, and the sternal furcula and midline to the nipple. The diameter of the areola, the distance between the breasts and the distance between the nipples were measured. In addition, lateral, superior and medial pinch test was performed to determine the size of the skinfold, assisting in the choice of the appropriate surgical technique for the patient.
The surgeries were performed in the hospital operating room, and the surgical marking was already performed the day before. The patients were submitted to general anesthesia, breast infiltration with 0.9% saline solution was performed, with diluted adrenaline in 1:300,000 and 5ml of Naropin 0.5%.
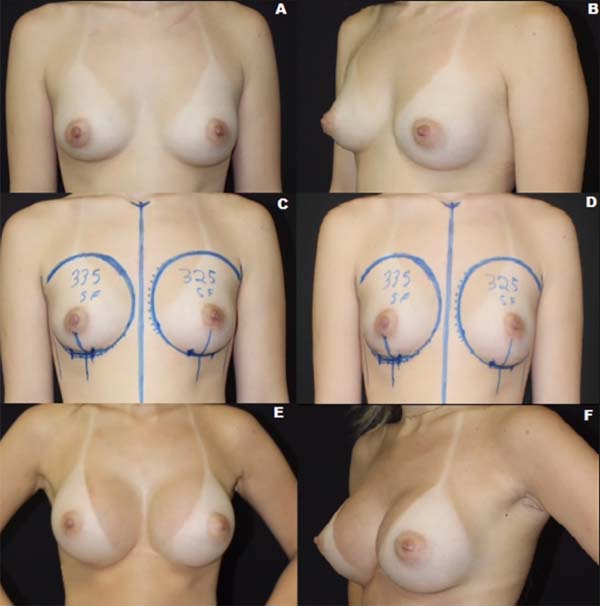
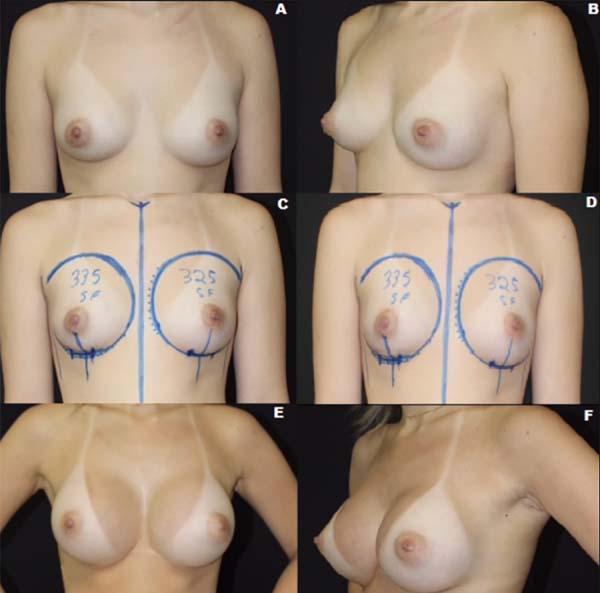
The incision performed varied as agreed in advance with the patients. The surgical technique includes subfascial detachment (Figure 1) and the making of the pocket; in homeostasis, electrocautery was used. Then, the pocket was washed with sterile serum and inserted the textured prosthesis. The appropriate positioning of the prostheses was checked, and the surgical plans were closed.
The mean time of the procedure by the subfascial technique was approximately 60 minutes.
RESULTS
The sample consisted of 233 female patients who underwent prosthesis placement procedures using the subfascial technique. The mean age of the sample was 30.08 (±6.8) years, with a minimum of 17 years and 56 years of maximum.
The choice of access route was determined by the patient with the help of the surgeon, 5 patients (2.1%) chose to access the axillary, another 4 (1.7%) chose the areolar route, the rest of the patients (96.1%) chose to make the incision in the inframammary sulcus.
The prostheses used ranged from 220g to 460g (Figure 2); according to the need evaluated by the doctor and the preference of each patient, the most chosen are between 295g and 325g with an average of 315.5g. In the observed period, there was an increase in the size of the implant chosen by the patients in approximately 24.84g. Two hundred twenty-eight patients chose the round prosthesis shape (97.9%), the anatomical one by only 3 patients (1.3%) and 2 patients (0.9%) opted for the round shape with high projection.
During this period, only one postoperative complication occurred: late seroma (0.429%), which occurred 4.5 years after the date of the procedure, and no muscle contracture, hematoma or any other complication was reported.
DISCUSSION
The breast rests on the anterolateral part of the thorax, especially on the second to the sixth ribs. It is located over the pectoralis major muscle. Its limits include the clavicle superiorly, the sternum medially, the inframammary fold inferiorly and the anterior edge of the latissimus dorsi determines its lateral extension8.
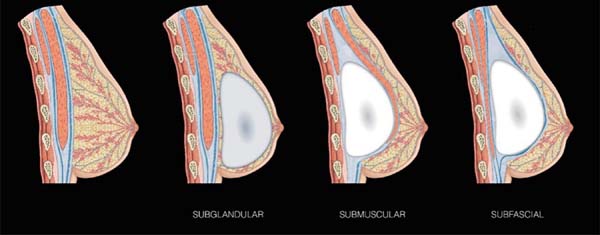
Breast implants can be placed in the subglandular, subfascial or submuscular space, as shown in Figure 3.
Graf et al. (2003)3 documented that the subfascial approach eliminates implant animation caused by contraction of the pectoral muscle with arm movement compared to the submuscular implant technique. In addition to the contour of the breasts become more rounded, because it does not suffer interference from the muscle layer3,5,7. The submuscular plane may cause distortion of the implant due to the reaction of muscle fibers to the capsule or skin, which may cause traction, curling or asymmetry9,10. Postoperative recovery is faster and less painful, as there are no large areas of muscle dissection3,7,10. According to Benito-Ruiz (2003),11 patients with subfascial increase return to normal activities approximately four days before.
The subfascial technique provides a greater aesthetic result when compared to the subglandular technique by masking the contour of the prosthesis, reducing the visibility of the edge and providing a more gradual transition from the parenchyma to the implant, resulting in a more natural form of the breast5,12 (Figures 4 and 5). One of the main characteristics of subfascial breast augmentation is creating a stronger support system for the upper implant pole. The displacement of the implant in the upper direction is avoided because the upper pole is placed between the muscle and the fascia, which constitutes a stronger support system than only the breast parenchyma and/or subcutaneous tissue in the conventional subglandular approach12. The implant remains firmly in place, and a natural result is reinforced because the skin and subcutaneous tissue in the upper third of the pocket are not directly in contact with the implant12,13.
The indexes published by Vucovich and Khosla (2013)7 show that the incidence of late seroma is rare, ranging from 0.1%-1.7%, which is confirmed by our study, where they presented only one case (0.429%) after 4.5 years from the date of the procedure. In addition, they describe that the hematoma index varies from 0.5%-0.9%. In the present study, no hematoma was identified postoperatively; the risk of hematoma is small since bleeding is negligible11. In the long run the risk of ptosis occurring is reduced due to the lower rupture of the connective fibers between the deep layer of the surrounding fascia surrounding the breast and the fascia of the pectoralis7. The complications of the subfascial technique were lower when compared to the submuscular and subglandular techniques (18.3%)7.
The upper pinch test smaller than 2cm is the only relative contraindication to perform this procedure. However, in this situation, it may be suggested for the patient to reduce the size of the chosen prosthesis to perform the subfascial technique because the implant has better coverage in the upper pole requiring a greater amount of tissue in this location, thus provides better aesthetic results and avoids the artificial visibility of the prosthesis, besides assisting the coverage of adjacent tissue5,7.
CONCLUSION
The subfascial technique has been increasingly used by plastic surgeons because it presents satisfactory aesthetic results and low rates of complications, as shown in the study, becoming a differentiated option for patients who will perform augmentation mammoplasty.
REFERENCES
1. Garcia AMC, Garcia BGBC, Silva M. Mastoplastia de aumento periareolar com descolamento subfascial rombo. Rev Bras Cir Plást. 2010 Jul/Set;25(3):478-83.
2. D'Ávila AK, Gonçalves GA, Accioli ZV, Accioli JJ, Vieira JV, Bins-Ely J, et al. Mamaplastia de aumento: revisão dos resultados em 352 pacientes. Arq Catarin Med. 2007;36(Supl 1):S169-S72.
3. Graf R, Bernardes A, Rippel R, Araujo LR, Damasio RC, Auersvald A. Subfascial breast implant: a new procedure. Plast Reconstr Surg. 2003 Fev;111(2):904-8.
4. Ali A, Eleathy E, Abdo-Fotouh S, Frag M. Subfascial breast augmentation: review of a 2-year experience with 100 cases. Egypt J Plast Reconstr Surg. 2011 Jan;35(1):41-6.
5. Hunstand JP, Webb LS. Subfascial breast augmentation: a comprehensive experience. Aesthet Plast Surg. 2010 Jul;34(3):365-73.
6. Carreirão S, Cardim V, Goldenberg D. Cirurgia Plástica - Sociedade Brasileira de Cirurgia Plástica. São Paulo: Atheneu; 2005.
7. Vucovich M, Khosla RK. Breast augmentation. Plast Surg. 2013;11(4):1-73.
8. Neligan P. Cirurgia plástica. 3a ed. Rio de Janeiro: Elsevier; 2015.
9. Jinde L, Jianliang S, Xiaoping C, Xiaoyan T, Jiaqing L, Qun M, et al. Anatomy and clinical significance of pectoral fascia. Plast Reconstr Surg. 2006 Dez;118(7):1557-60.
10. Barbato C, Pena M, Triana C, Zambrano MA. Augmentation mammoplasty using the retrofascia approach. Aesthetic Plast Surg. 2004 Mai/Jun;28(3):148-52.
11. Benito-Ruiz J. Transaxillary subfascial breast augmentation. Aesthet Surg J. 2003 Nov/Dez;23(6):480-3.
12. Siclovan HR, Jomah JA. Advantages and outcomes in subfascial breast augmentation: a two-year review of experience. Aesthetic Plast Surg. 2008 Jun;32(3):426-31.
13. Goés JCS, Landecker A. Optimizing outcomes in breast augmentation: seven years of experience with the subfascial plane. Aesthetic Plast Surg. 2003 Mai/Jun;27(3):178-84.
14. Standring, S. Gray's Anatomy 40 ed. Rio de Janeiro: Elsevier; 2010. Produzido e editado por Henrique Boell - Lages SC.
1. University of Planalto Catarinense, Lages, SC, Brazil.
2. Brazilian Society of Plastic Surgery, São Paulo, SP, Brazil.
3. Brazilian College of Surgeons, Rio de Janeiro, RJ, Brazil.
4. Federal University of Paraná, Curitiba, PR, Brazil.
5. Assis Gurgacz College, Cascavel, PR, Brazil.
HS Analysis and/or data interpretation, Conception and design study, Data Curation, Formal Analysis, Methodology, Project Administration, Software, Validation, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing.
LSG Conception and design study, Formal Analysis, Methodology, Software, Writing - Original Draft Preparation, Writing - Review & Editing.
TB Conceptualization, Final manuscript approval, Project Administration, Realization of operations and/or trials, Supervision.
BCH Analysis and/or data interpretation, Data Curation, Writing - Original Draft Preparation.
BBG Analysis and/or data interpretation, Final manuscript approval, Methodology, Writing - Original Draft Preparation.
Corresponding author: Heboni Sabadin, Mário Antunes da Cunha 511, 101 B, Petrópolis, Porto Alegre, RS , Brazil, Zip Code 90690-400. E-mail: heboni_sabadin@hotmail.com / heboni_sabadin@hotmail.com
Article received: December 07, 2020.
Article accepted: May 18, 2021.
Conflicts of interest: none.








 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter