

Review Article - Year 2021 - Volume 36 -
Lipografting in breast reconstruction after breast cancer treatment: literature review
Lipoenxertia na reconstrução mamária após tratamento do câncer de mama: revisão de literatura
ABSTRACT
Introduction: The treatment of breast cancer through mastectomy greatly impacts patients' quality of life, causing an increasing number of searches for reconstructive procedures. The fat graft, also known as lipografting, was described by Neuber in 1893, and has increased its use and acceptance over the years. According to the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery), reconstructive surgeries correspond to 39.7% of plastic procedures performed in Brazil, with breast reconstructions being 6.1% of this number, constituting part of breast cancer treatment. The present study aimed to review the use of lipografting in breast reconstruction after breast cancer treatment.
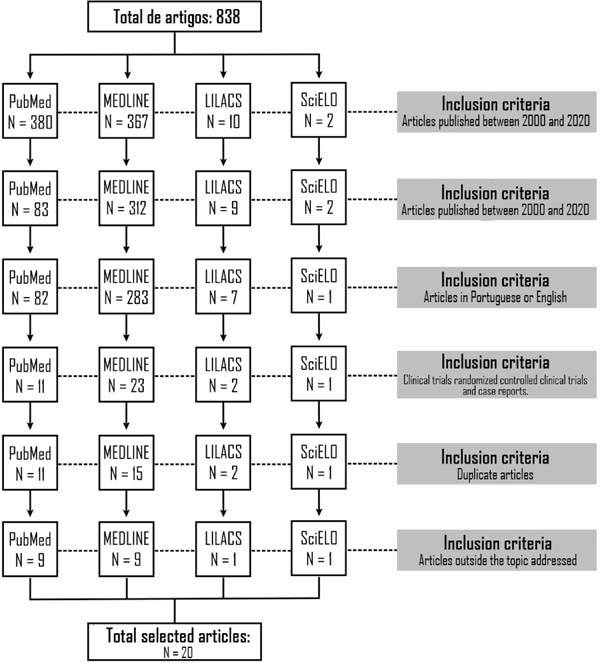
Methods: A review of the literature was carried out using the databases of PubMed, MEDLINE, LILACS and SciELO, using the descriptors: "breast reconstruction"; "fat grafting"; and "breast cancer".
Results: In total, 838 articles were found in the databases searched, of which 20 were selected for data extraction after applying the inclusion and exclusion criteria.
Conclusion: It was found that autologous fat is a well-established procedure for mammary reconstruction, despite presenting some possible complications. Furthermore, more long-term studies should be conducted to address the understanding and safety of the procedure.
Keywords: Mammoplasty; Autologous transplantation; Mastectomy; Breast neoplasms; Adipose tissue.
RESUMO
Introdução: O tratamento de câncer de mama através de mastectomia causa grande impacto na qualidade de vida dos pacientes, ocasionando um número crescente de buscas por procedimentos reconstrutivos. O enxerto de gordura, também conhecido como lipoenxertia, foi descrito pela primeira vez em 1893, por Neuber, tendo aumentado o seu uso e aceitação no decorrer dos anos. De acordo com a Sociedade Brasileira de Cirurgia Plástica, as cirurgias reparadoras correspondem a 39,7% dos procedimentos plásticos realizados no Brasil, com as reconstruções mamárias sendo 6,1% desse número, configurando parte do tratamento do câncer de mama. O presente estudo objetivou revisar o uso de lipoenxertia na reconstrução mamária após tratamento do câncer de mama.
Métodos: Foi realizada uma revisão da literatura utilizando os bancos de da-dos PubMed, MEDLINE, LILACS e SciELO, através dos descritores: "breast reconstruction"; "fat grafting"; and "breast cancer".
Resultados: No total, foram encontrados 838 artigos nas bases de dados pesquisadas, dos quais 20 foram selecionados para a extração dos dados após a aplicação dos critérios de inclusão e exclusão.
Conclusão: Constatou-se que a gordura autóloga é um procedimento bem estabelecido para reconstrução mamária, apesar de apresentar algumas possíveis complicações. Ademais, mais estudos a longo prazo devem ser realizados visando conso-lidar o entendimento e segurança do procedimento.
Palavras-chave: Mamoplastia; Transplante autólogo; Mastectomia; Neoplasias da mama; Tecido adiposo
INTRODUCTION
In Brazil, in 2020, the incidence estimated by the National Cancer Institute (INCA) concerning breast cancer in women was 66,280 cases, according to the primary location of the tumor and gender, corresponding to 29.7% of the neoplasms estimated for the year, which reinforces the position of cancer more prevalent in women. Between 2015 and 2018, there were 66,532 deaths from breast cancer nationwide, affecting 65,768 women (98.85%) and 764 men (1.15%)1.
Thus, a breast cancer diagnosis has a considerable psychological impact on patients, which can cause depressive disorders, amplification of physical symptoms, functional impairment, and decreased adherence to the proposed treatments2. Therefore, breast cancer treatment through mastectomy has an important influence on patients’ quality of life, which has caused an increasing number of searches for reconstructive procedures after mastectomy, either immediately or late(3.)
In 1893, the fat graft was described by Neuber4, having increased its use and acceptance over the years. Since 1990, together with the advancement of techniques and extensive experimental and clinical studies, there has been a growth in the number of plastic surgeons using autologous fat grafting as a technique for breast reconstruction3.
With these advances, in 1997, it was decided through the resolution of the Federal Council of Medicine No. 1,483/97 that breast reconstruction is part of the treatment of the disease when there is an indication for correction of deformities generated by mastectomy5. Moreover, in 2018, law no. 13,770 was sanctioned, ensuring to women with breast cancer the right to reconstructive plastic surgery in both breasts, even if the tumor only appears in one of them, guaranteeing the right to contralateral breast symmetrization and reconstruction of the areolopapilar complex6.
In 2005, Spear7 reported that autologous fat transplants, also known as lipografting, are a safe technique capable of correcting or improving deformities in mammary reconstructions7. Since 2007, the French Society of Plastic and Reconstructive Surgery has advised using autologous fat graft strictly. However, in 2011 they changed their position, suggesting that the procedure would become part of a clinical protocol8,9. The American Society of Plastic Surgeons, on the other, discouraged the use of fat grafting for years. However, in 2015, the society reported evidence supporting the use of fat grafting to maximize the aesthetic results of post-mastectomy breast reconstruction10.
In Brazil, between 2015 and 2019, according to the Department of Informatics of the Unified Health System (DATASUS), there were 51,269 hospitalizations for mastectomies, including radical mastectomy with lymphadenectomy, simple, radical with axillary lymphadenectomy in oncology and simple mastectomy in oncology11. Moreover, according to the census conducted in 2018 by the Brazilian Society of Plastic Surgery, reparative surgeries correspond to 39.7% of plastic procedures performed in Brazil, with breast reconstructions being 6.1%12.
Thus, because of the number of mastectomies performed in the national territory and the psychological advantages of breast reconstructions and the percentage that these surgical interventions represent within plastic surgery, it is important to understand more about the available therapeutic options.
OBJECTIVE
Conduct a review of the literature on the use of lipografting in breast reconstruction after breast cancer treatment.
METHODS
A literature review was conducted based on: 1) preparation of a question to be researched; 2) choice of data sources; 3) election of keywords for search; 4) search and storage of results; 5) selection of articles according to inclusion and exclusion criteria; 6) extraction of data from selected articles; 7) synthesis and interpretation of the data.
The main question of the search was: “what is the application of autologous fat graft in breast reconstruction after mastectomy in patients affected by breast cancer?”. The articles were surveyed using PubMed, MEDLINE, LILACS and SciELO databases in July 2020, and the descriptors were used: “breast reconstruction”; “fat grafting,”; “breast cancer”, using the Boolean operator “AND”.
The studies should contain information on the use of lipografting in breast reconstruction after mastectomy performed for cancer treatment to be included in this literature review.
The inclusion criteria used were articles published between 2010 and 2020; full articles available free of charge; articles in Portuguese or English; randomized controlled trials; and case reports. Exclusion criteria were duplicate articles and articles outside the theme addressed.
RESULTS
We found 838 articles in the databases surveyed, of which 20 were selected for data extraction, with their synthesizing and interpretation (Figure 1).
The extracted information was separated into the following topics: author, year, objective, considerations (Table 1).
| Authors | Year | Objective | Final considerations |
|---|---|---|---|
| Kolasinski13 | 2019 | Present a concept of breast reconstruction with fat graft combined with internal tissue expansion. | Breast reconstruction with fat graft combined with tissue expansion is a promising method of total breast reconstruction after mastectomy. |
| Sowa et al.14 | 2019 | Describe the case of a patient with invasive ductal carcinoma treated with mastectomy with subsequent breast reconstruction using flap and fat graft. | The fat graft removed from zone IV in a DIEP flap is an ideal option for cosmetic breast augmentation in patients who wish to achieve a natural and moderate increase of the neckline line in the upper thorax. |
| Fujiwara et al.15 | 2018 | Describe the details of a breast reconstruction case using an expander and tissue implant, combined with fat grafting, in a patient with severe depressive breast deformation after breast conservation therapy. | The results showed that the presenting method might be an option for late reconstruction after conservative breast therapy. |
| Skendelas et al.10 | 2018 | Present a case of a patient with a mutation in the T37K BRCA variant and an unusual pattern of recurrence of breast cancer after mastectomy, reconstruction and early fat grafting. | The diagnosis was complicated by the anticipated side effects of the fat graft, which is a well-established reconstructive procedure. As BRCA-positive and variant patients are generally younger patients who can seek breast reconstruction options for aesthetic purposes, we believe that the possibility of breast cancer recurrence should always remain at the forefront of the differential diagnosis in the case of an unusual clinical presentation. |
| Bennet et al.4 | 2017 | Determine whether fat grafting is associated with the results reported in patients undergoing mammary reconstruction. | Fat grafting can improve breast satisfaction, psychosocial and sexual well-being in patients undergoing breast reconstruction. |
| Stumpf et al.16 | 2017 | Evaluate local and systemic recurrence of breast cancer in patients submitted to autologous fat graft in immediate reconstruction after conservative surgery for breast cancer. | There was no significant difference for local or systemic recurrence of breast cancer in the groups studied. The immediate autologous fat graft appears to be a safe procedure. |
| Cheng et al.17 | 2016 | Describe a case of a 36-year-old woman with mucinous carcinoma in the right breast discovered two months after the fat graft. | This case again raises the question about the possible links between breast cancer and fat grafts. |
| Al-Kalla et al.2 | 2014 | Describe a case of a 68-year-old male patient submitted to unilateral breast reconstruction, successful only with the fat grafting technique. | Although the behavior of transferred fat is not well understood, fat grafting is a very powerful reconstructive modality to recreate the unique shape of the male breast after mastectomy. |
| Daye e Conant18 | 2014 | Highlight the mammographic and tomosynthetic findings observed after lipomodeling that may present diagnostic challenges in this patient population. | In conclusion, with the increasing use of autologous fat grafting in breast cancer survivors, radiologists should acquire an in-depth knowledge of the imaging changes that follow this procedure. It is recommended to perform pre-and post-lipomodeling images to restore a baseline for patients undergoing this procedure. |
| Howes et al.19 | 2014 | Evaluate the viability of breast reconstruction only by autologous fat graft in the context of RoFA mastectomy. | This case demonstrates the potential for the use of fat grafting in reconstruction. Results in larger patient populations are needed to confirm these findings. |
| Mestak et al.3 | 2013 | Describe a case of breast reconstruction after mastectomy using autologous fat transfer combined with brava external tissue expansion system. | The use of the BRAVA external expansion system to improve the fat graft is an appropriate technique for breast reconstruction after a mastectomy. This technique produces soft and natural breasts in fewer surgical sessions, with minimal risk of complications. Patient adhesion, however, is extremely necessary to achieve the desired results. |
| Alharbi et al.9 | 2013 | Discuss the possible relationship between lipografting and cancer recurrence. | The issue of breast cancer risks has again been raised and encouraged people to continue to be careful. |
| Bezerra et al.7 | 2013 | Validate a way to correct breast contour defects after the previous reconstruction through conventional techniques with fat grafting after eight years of practice. | Lipografting is a safe technique, with low morbidity and high satisfaction levels for those involved, even though it is necessary to perform multiple surgical procedures to achieve a good result. |
| Chaput et al.8 | 2013 | Report recurrence of an invasive ductal carcinoma four months after autologous fat grafting. | Atypical in its chronology and histology, this case allows us to raise questions about this procedure and its controversial characteristics about breast cancer again. |
| Hoppe et al.20 | 2013 | Describe an optimized treatment and follow-up protocol for new breast reconstruction after total mastectomy only with lipotransfer. | Complete breast reconstruction with large volume fat grafting is, alternatively, possible to standard techniques in selected cases. At least 4 to 6 lipotransfers are required over two years. Patients with prior radiotherapy may require up to 8 sessions in almost three years of treatment. |
| Kim et al.21 | 2012 | Describe bilateral liponecrotic pseudocysts after breast fat injection. | Autologous fat grafting in the breast is not a simple procedure and should be performed by well-trained and qualified plastic surgeons. During surgery, care should be taken. |
| Mojallal et al.22 | 2012 | Presenting a case of bilateral philodic tumors in a 28-year-old woman with Poland syndrome and discuss (1) the relationship between the condition and breast cancer, (2) the modes of surveillance in patients with Poland syndrome and (3) its impact on breast reconstruction. | Patients with Poland syndrome have the same risk of breast cancer or borderline tumors as the general population. Therefore, when a patient with this syndrome presents for treatment, bilateral mammography and an ultrasound should be performed before proceeding with the mammary reconstruction. The possible development of breast cancer in patients with the anomaly should influence the surgeon's choice of reconstruction techniques, including fat grafting. |
| Panettiere et al.23 | 2011 | Describe the reconstruction of an irradiated breast using lipografting after reconstruction failure with prosthesis. | Fat graft transplantation can be a reliable and safe option for body reconstruction in selected patients. |
| Rigotti et al.24 | 2010 | Compare the incidence of local and regional recurrence of breast cancer between two contiguous time windows in a homogeneous population of 137 patients submitted to adipose tissue transplantation after a modified radical mastectomy. | Although further confirmation is required from multicenter randomized clinical trials, our results support the hypothesis that autologous lipoaspirated transplantation combines impressive regenerative properties with null or marginal effects on the likelihood of post-mastectomy locoregional recurrence of breast cancer. |
| Salgarello et al.25 | 2010 | Presented the preliminary results of alternative surgical treatment in breast oncoplastic surgery, consisting of fat injections before implant placement. | Preliminary results show that fat injection into irradiated tissue before alloplastic breast reconstruction may reduce radiation-related complications in implants. The benefits of fat grafting are following the theoretical basis of this surgery. Larger studies are needed to confirm our observations. |
In addition, among the main points described in the analyzed articles, 17 pointed out benefits of the autologous fat graft procedure, 13 commented on whether there was a correlation between the procedure and cancer recurrence, 12 talked about the issue of radiological findings and their differentiation, and 2 presented special clinical cases, one of male breast reconstruction and another of reconstruction after mastectomy in a patient with Poland syndrome.
DISCUSSION
Autologous fat has revitalizing capacity in tissues affected by breast cancer treatment, favoring its biological and mechanical restoration10,25. This material has ideal properties because it naturally integrates tissues since it is autologous, being biocompatible3.
Thus, adipose tissue transplantation is a good way to treat the effects caused by breast oncologic therapies, as well as chronic diseases and cosmetic unsatisfactory, and can be done uniquely or combined with other approaches13,15,24.
In breast reconstruction by lipografting, the procedure produces soft breasts with a soft tactile sensation, improved skin texture, increased subcutaneous layer and superior symmetry, recovering the natural contour3,14,20. Its results include minimal scars and efficacy in the simultaneous restoration of multiple irregularities14.
The procedure can be performed in almost all patients since the significant contraindications are only for patients with active local neoplasms or radiodermatitis and can be done with local or general anesthesia. The technique is considered relatively easy and low cost and can be used after therapeutic failure with other types of reconstruction23.
However, like every surgical procedure, some complications may occur, being them: liponecrotic pseudocysts, infection, granuloma, hematoma, fatty necrosis and fibrosis10,20,21. Among these complications, the rates of occurrence are low, with most of them being controlled by breast imaging, evolving with spontaneous resolution18,20.
Moreover, the lipografting procedure presents estimated volume loss after grafting between 25 and 43.5%, varying the results according to several studies19. If a second session is held, the absorption rates are between 20% and 30%7. Furthermore, the advent of the Coleman technique allowed the reduction of fat resorption rates and complications4,16.
Regarding the question raised in studies on whether there is a correlation between autologous fat use and cancer recurrence, it is estimated that for every 1,000 women who undergo lipografting, 7 may develop a local relapse after one year. In contrast, for every 1,000 who do not undergo lipografting, nine may present recurrence; that is, the real impact of autologous fat graft on the resurgence of breast cancer is unknown. There is no significant evidence to link lipografting to new cases of neoplasia17,24.
After lipografting, some reports have described radiological findings that suggest the formation of calcifications and nodules in the breasts, which at first could be confused with breast cancer14,19. However, more recent studies show that radiologists should not have difficulties distinguishing between tumor calcifications and post-graft fat. It is possible to treat complications without the occurrence of post-operative deformities and concern with malignancy of the findings3,19. Moreover, USG plays an important role in the follow-up of patients after lipografting23.
Autologous fat grafting is also appropriate for restoring the breast of male patients after mastectomy to remove breast cancer. Due to the characteristics of the male chest wall, this procedure can offer more satisfactory and natural results since the prostheses are designed for female patients2.
In addition, in patients with Poland syndrome associated with breast cancer, lipografting should be reserved to restore infraclavicular and anterior axillary defects and should be performed only after careful pre and post-operative examination mammography, ultrasound and magnetic resonance imaging, if indicated22.
CONCLUSION
Through the review, it was possible to verify that the use of autologous fat in breast reconstruction is a well-established procedure, consisting of a good technique, generating good results, such as soft breasts, improvement in skin texture, increase of subcutaneous layer, symmetry and recovery of the natural contour. These results help improve the quality of life of patients undergoing the procedure since they have psychosocial benefits.
However, lipografting can cause complications such as pseudocysts, infection, granuloma, hematoma, fibrosis, fatty necrosis, and local ischemia. Thus, the plastic surgeon must have experience performing the procedure to apply the correct technique, reducing the risks of complications. In addition, it is important that radiologists who follow the case are well trained and can interpret radiographic findings with greater accuracy.
Moreover, there must be more long-term studies, with the support of the Plastic Surgery Societies, to understand if there is a real correlation between breast cancer resurgence and autologous fat in breast reconstructions, ensuring greater understanding and safety about the procedure.
REFERENCES
1. Ministério da Saúde (BR). Instituto Nacional de Câncer José Alencar Gomes da Silva (INCA). Atlas de mortalidade por câncer - tabulador [Internet]. Rio de Janeiro: Ministério da Saúde/INCA; 2014; [acesso em 2020 Ago 08]. Disponível em: https://www.inca.gov.br
2. Al-Kalla T, Komorowska-T E. Total male breast reconstruction with fat grafting. Plast Reconstr Surg Glob Open. 2014 Nov;2:e257.
3. Mestak O, Mestak J, Bohac M, Edriss A, Sukop A. Breast reconstruction after a bilateral mastectomy using the BRAVA expansion system and fat grafting. Plast Reconstr Surg Glob Open. 2013 Dez;1(8):71-5.
4. Bennet KG, Qi J, Kim HM, Hamill JB, Wilkins EG, Mehrara BJ, et al. Association of fat grafting with patient-reported outcomes in postmastectomy breast reconstruction. JAMA Surg. 2017 Out;152(10):944-50.
5. Conselho Federal de Medicina (BR). Resolução CFM no 1.483, de 11 de setembro de 1997. Diário Oficial da União, Brasília (DF), 22 set 1997: Seção 1: 21075.
6. Lei nº. 13.700, de 19 de dezembro de 2018 (BR). Dispõe sobre a cirurgia plástica reconstrutiva da mama em casos de mutilação decorrente de tratamento de câncer. Diário Oficial da União, Brasília (DF), 20 dez 2018: Seção 1: 1.
7. Bezerra FJF, Moura RMG, Maia Neto JD. Lipoenxertia em reconstrução mamária. Rev Bras Cir Plást. 2013;28(2):241-6.
8. Chaput B, Foucras L, Le Guellec S, Grolleau JL, Garrido I. Recurrence of an invasive ductal breast carcinoma 4 months after autologous fat grafting. Plast Reconstr Surg. 2013 Jan;131(1):123e-4e.
9. Alharbi M, Garrido I, Vaysse C, Chavoin JP, Grolleau JL, Chaput B. Latissimus dorsi flap invasion by ductal breast carcinoma after lipofilling. Plast Reconstr Surg Glob Open. 2013 Nov;1(8):e68.
10. Skendelas JP, Lee C, Mangino A, Carson WE. Unusual recurrence of breast cancer in a BRCA-variant patient after fat grafting. Clin Case Rep. 2018 Dez;6(12):2457-62.
11. Ministério da Saúde (BR). Departamento de Informática do Sistema Único de Saúde (SIH/DATASUS). Portal da Saúde - SUS. Brasília (DF): Ministério da Saúde; 2020.
12. Fonseca A, Ishida LH. Censo 2018 análise comparativa das pesquisas 2014, 2016 e 2018. São Paulo (SP): Sociedade Brasileira de Cirurgia Plástica (SBCP); 2018.
13. Kolasinski J. Total breast reconstruction with fat grafting combined with internal tissue expansion. Plast Reconstr Surg Glob Open. 2019 Abr;7(4):e2009.
14. Sowa Y, Kodama T, Morita D, Numajiri T. Fat grafting with harvesting from zone IV in the DIEP flap. Eplasty. 2019 Mai;19:ic14.
15. Fujiwara T, Yano K, Tanji Y, Nomura M. Staged prosthetic reconstruction with fat grafting for severe depressive breast deformation after breast-conserving therapy. Plast Reconstr Surg Glob Open. 2018 Mar;6(3):e1717.
16. Stumpf CC, Biazus JV, Zucatto FSAE, Cericatto R, Cavalheiro JAC, Damin APS, et al. Reconstrução imediata com enxerto autólogo de gordura: influência na recorrência local de câncer de mama. Rev Col Bras Cir. 2017 Mar;44(2):179-86.
17. Cheng L, Han XF, Zhang C, Lv LL, Li FC. Occurrence of breast mucinous carcinoma after autologous fat grating for breast augmentation. Aesthetic Plast Surg. 2016 Fev;40(1):102-5.
18. Daye D, Conant E. Digital breast tomosynthesis findings after surgical lipomodeling in a breast cancer survivor. J Radiol Case Rep. 2014 Set;8(9):9-15.
19. Howes BHL, Fosh B, Watson DI, Yip JM, Eaton M, Smallman A, et al. Autologous fat grafting for whole breast reconstruction. Plast Reconstr Surg Glob Open. 2014 Mar;2(3):e124.
20. Hoppe DL, Ueberreiter K, Surlemont Y, Peltoniemi H, Stabile M, Kauhanen. Breast reconstruction de novo by water-jet assisted autologous fat grafting - a retrospective study. Ger Med Sci. 2013;11:Doc17.
21. Kim H, Yang EJ, Bang SI. Bilateral liponecrotic pseudocysts after breast augmentation by fat injection: a case report. Aesthetic Plast Surg. 2012 Abr;36(2):359-62.
22. Mojallal A, La Marca S, Shiphov C, Sinna R, Braye F. Poland syndrome and breast tumor: a case report and review of the literature. Aesthet Surg J. 2012 Jan;32(1):77-83.
23. Panettiere P, Accorsi D, Marchetti L, Sgrò F, Sbarbati A. Large-breast reconstruction using fat graft only after prosthetic reconstruction failure. Aesthetic Plast Surg. 2011 Out;35(5):703-8.
24. Rigotti G, Marchi A, Stringhini P, Baroni G, Galiè M, Molino AM, et al. Determining the oncological risk of autologous lipoaspirate grafting for post-mastectomy breast reconstruction. Aesth Plast Surg. 2010 Ago;34(4):475-80.
25. Salgarello M, Visconti G, Farallo E. Autologous fat graft in radiated tissue prior to alloplastic reconstruction of the breast: report of two cases. Aesthetic Plast Surg. 2010 Fev;34(1):5-10.
1. University of Vassouras, Medical Course, Vassouras, RJ, Brazil.
2. University Hospital of Vassouras, Plastic Surgery, Vassouras, RJ, Brazil.
Corresponding author: Thaís Moreira Lara Rua Benedito Pereira Rocha, 304, Parque das Palmeiras, Angra dos Reis, RJ, Brazil. Zip Code: 23906-485. E-mail: thais.lara@hotmail.com
Article received: September 02, 2020.
Article accepted: April 23, 2021.
Conflicts of interest: none
COLLABORATIONS
TML Analysis and/or data interpretation, Conception and design study, Conceptualization, Data Curation, Final manuscript approval, Investigation, Methodology, Project Administration, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing
VRPP Analysis and/or data interpretation, Conception and design study, Conceptualization, Data Curation, Final manuscript approval, Investigation, Methodology, Project Administration, Visualization, Writing - Original DraftPreparation, Writing - Review & Editing
LALP Conceptualization, Final manuscript approval, Project Administration, Supervision, Visualization, Writing - Review & Editing





 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter